Abstract
Purpose
To ascertain the anatomic and radiological parameters of the atlas (C1) pedicle and to explore a preferable method of C1 pedicle screw insertion.
Methods
Thirty-four conserved human cadaveric cervical spines (20 males, 14 females) underwent computed tomography (CT) scanning. Trajectories P (perpendicular to the coronal plane) and I (with medial inclination) were designed for each C1 pedicle on CT images. External pedicle wall width, medullary cavity width, transverse angle, and optimal entry point along each trajectory were measured. Cortical screws of 3.5 mm in diameter were inserted into C1 pedicles along trajectory P and I, respectively, and wall perforation was assessed (post-operative CT scanning).
Results
The external pedicle wall width and medullary cavity width along trajectory I were significantly wider than trajectory P (P < 0.01). Although external pedicle wall widths were all greater than 3.5 mm, medullary cavity width <3.5 mm was found in 16.1 % pedicles along trajectory P and only 2.9 % along trajectory I. Transverse angle was 21.8° along trajectory I and 0° along trajectory P. Optimal entry point of trajectory I was 4.1 mm lateral from that of trajectory P. The lateral wall perforation rate was significantly lower along trajectory I than trajectory P (P < 0.05).
Conclusions
C1 pedicle screw trajectory with medial inclination and more lateral entry points yielded wider medullary cavity width than that perpendicular to the coronal plane, and might minimize lateral wall perforation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The atlantoaxial motion segment is the most mobile region of the entire vertebral column. When destabilised, it is difficult to control the motion of the destabilised C1-C2 segment to achieve a satisfactory fusion [1–3]. The previous studies have reported that nonunion rates for the C1-C2 procedures range from 10 to 30 % and the fusion rate could improve if the C1-C2 motion could be controlled satisfactorily [4–8]. The most recent techniques for C1 posterior fixation in upper cervical vertebra stabilisation include lateral mass screws and pedicle screws via the posterior arch and lateral mass. In addition, a previous study has showed that biomechanical stability such as stiffness and pullout strength of a C1 pedicle screw is superior to that of a lateral mass screw [9]. However, controversy over the transverse direction of the C1 pedicle screw has existed for a long time [10–12]. Tan et al. [10] suggested that the screw trajectory should be perpendicular to the coronal plane, whereas Ma et al. [11] recommended medial inclination by about 10°, because complications such as neurovascular injury could arise from the lateral mass screw technique [13, 14].
In present study, we designed two trajectories, including trajectory P (trajectory perpendicular to the coronal plane) and trajectory I (trajectory with medial inclination), which were respectively similar to Tan et al.’s and Ma et al.’s methods. Morphological measurements and pedicle screw insertion were performed in order to determine a preferable screw trajectory.
Materials and methods
Specimens
Thirty-seven formalin-fixed Chinese cadavers were provided by the Department of Human Anatomy of Xuzhou Medical College. Informed written consents were obtained from donors’ relatives. The study was approved by the Institutional Review Board of Xuzhou Medical College (No. XMC01336). Cervical CT scanning for each specimen was performed using a Siemens 128-slice spiral CT scanner (Siemens Medical Solutions, Shanghai, China). Subjects with evidence of fracture, congenital anomalies or structural abnormality of C1 were excluded. Accordingly, three specimens (two males and one female) were excluded. CT images using 1.0-mm thick slices of the remaining specimens were delivered to the Syngo image workstation (Siemens Medical Solutions, Shanghai, China). Multiplanar reformation (axial, sagittal and coronal plane) was performed on each C1 pedicle (40 pedicles in 20 males and 28 in 14 females).
Establishment of pedicle screw trajectories
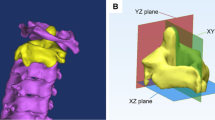
Two screw trajectories (trajectory P and I) for each C1 pedicle were established on CT images as illustrated in Fig. 1. On C1 axial image, the central axis of trajectory P was parallel to C1 midline (Fig. 1, left), and that of trajectory I was parallel to the lateral border tangent to the odontoid foramen and vertebral canal of C1 (Fig. 1, right). The central axis of each trajectory on the sagittal image was modulated through the centre of the posterior arch under the vertebral artery groove.
Trajectory P (TP) and trajectory I (TI) of C1 pedicle and relevant measurements on axial and coronal CT image TP trajectory P perpendicular to the coronal plane. TI trajectory I parallel to the lateral border tangent of the odontoid foramen and vertebral canal of C1, OEP optimal entry point for each trajectory, PT the posterior tubercle of C1, TPL the total pedicle length, EPW the external mediolateral width at the isthmus of the pedicle, MCW the medullary cavity width at the isthmus of the pedicle, TA the transverse angle of the pedicle screw projection in reference to the midline of C1
Pedicle screw insertion method
The entry point for trajectory P or trajectory I was defined with calipers (Shanghai Drawing Instruments Company, Shanghai, China) according to the pre-operatively measured distance from the posterior tubercle of C1 to the optimal screw entry point of each trajectory. C1 posterior tubercle was an obvious anatomical landmark on CT images or specimens for the measurement of the distance. The cortical bone at the entry point was removed with a grinding drill to reveal the cancellous bone. On the sagittal plane, the entry point was defined at the center of the C1 posterior lamina cancellous bone.
The transverse angle of trajectory P or trajectory I was guided with a special angular scale combined with an orientation hand (Shanghai Drawing Instruments Company, Shanghai, China) (Fig. 2). The inferior or superior wall of C1 posterior arch was subperiosteally dissected to determine the sagittal direction of the pedicle screw trajectory (Fig. 3). The pedicle screw could be placed freehand, followed by drilling the predetermined trajectory. Titanium cortical screws of 3.5 mm in diameter (Xinrong Medical Instrument Company, Suchow, China) were inserted into one side of C1 pedicle along trajectory P and the contralateral side along trajectory I.
Posterior view of C1 lamina and methods of neurovascular preservation along TI. Medial lamina (dotted arrow) is thicker than lateral one (linear arrow). Pedicle screw along TI could be placed without neurovascular injury by exposing superior and inferior wall of C1 posterior arch with careful subperiosteum stripping. It is difficult along TP because of the thicker lamina and the umbilicate posterior arch
Relevant parameters (Fig. 1):
-
1.
The distance from the posterior tubercle of C1 to the optimal screw entry point of each trajectory
-
2.
Transverse angle of trajectory I (Fig. 1, right), with that of trajectory P on the left being 0°
-
3.
Total pedicle length along each trajectory
-
4.
External pedicle wall width at the isthmus of the pedicle along each trajectory
-
5.
Medullary cavity width at the isthmus of the pedicle along each trajectory
-
6.
Superior-inferior height of the posterior arch under the vertebral artery groove
All assessments were carried out with digital measurement tools in the Syngo image workstation; the averages of the measured values were adopted.
Evaluation of screw position
Cervical CT scanning and multiplanar reconstructions were used for evaluation of post-operative screw position by an independent radiologist. The transverse angle of post-operative screw and its deviation degree from pre-operative transverse angle were also measured and calculated. The screw position was attributed one of four grades according to the evaluation criteria of Lee et al. [15]:
-
Grade 0: the entire screw was placed within the cortical bone of the pedicle.
-
Grade 1: less than 25 % of screw diameter violation.
-
Grade 2: 25–50 % of screw diameter violation.
-
Grade 3: more than 50 % of screw diameter violation.
Grades 0 and 1 were considered to be the correct positions, whereas grades 2 and 3 were considered misplacement. The direction of pedicle screw misplacement was classified as medial, lateral, superior, or inferior. If a screw breached simultaneously two pedicle walls, e.g., the superior-medial wall of C1 pedicle, the direction of the greatest wall perforation was considered the direction of screw misplacement [16].
Statistics
Statistical analysis was performed using the software of Statistical Program for Social Sciences 16.0 (SPSS 16.0 for Windows; SPSS, Chicago, IL, USA). C1 pedicle measurement data were displayed as mean ± SD. Enumerated data were displayed as percentage. Data associated with the C1 pedicle (the distance from the posterior tubercle of C1 to the optimal screw entry point, total pedicle length, external pedicle wall width, medullary cavity width, and superior-inferior height of the posterior arch) between trajectories were compared using the paired t-test. Male versus female differences were determined with the independent samples t-test. The rate of pedicle wall perforation between trajectory P and trajectory I was compared using the chi-square test.
P < 0.05 was considered statistically significant.
Results
Morphological observation of C1 pedicles on CT images
The axial CT images showed that the medial cortex of C1 pedicle was thicker than the lateral (Fig. 1). On sagittal CT images, the superior surfaces of C1 posterior arch were flat along trajectory I in all pedicles, but only 17.7 % (12 of 68) along trajectory P. The inferior surface of C1 posterior arch along each trajectory was smooth (Fig. 4a, b). On the posterior view of C1, the medial lamina was thicker than lateral, and C1 lamina became gradually thin laterally (Fig. 3).
Parameters of C1 pedicles along each trajectory
The measurements associated with C1 pedicle screw insertion along each trajectory are provided in Table 1. The results demonstrated that external pedicle wall width and medullary cavity width along trajectory I were significantly wider than that along trajectory P (P < 0.01). Although external pedicle wall width along each trajectory was greater than the screw diameter (3.5 mm), a value of medullary cavity width less than 3.5 mm was found in 16.1 % (11 of 68) pedicles along trajectory P (nine pedicles in females and two in males), but only 2.9 % (2 of 68) pedicles along trajectory I (all in females). Transverse angles for C1 pedicles were averaged 21.8 ± 8.2° along trajectory I and 0° along trajectory P. The optimal screw entry point of trajectory I was significantly lateral from that of trajectory P. The superior-inferior height of the posterior arch along each trajectory was the same (4.3 ± 0.9 mm). Twenty-two percent (15/68) of pedicles (including six pedicles in males and nine in females) had superior-inferior height of the posterior arch less than the 3.5 mm screw diameter. There was no statistically significant difference between trajectories for total pedicle length (P >0.05).
Evaluation of C1 pedicle screw position and pedicle screw perforation
Sixty-eight pedicles were successfully inserted with cortical screws, including 34 screws in each (trajectory P and trajectory I) group (Figs. 3 and 5). Data of post-operative transverse angle, and its deviation degree from pre-operative transverse angle, perforation of post-operative C1 pedicle screw were shown in Table 2. The results indicated that post-operative transverse angle along each trajectory deviated from the direction determined pre-operatively. However, there was no significant difference in its deviation degree between trajectory P and trajectory I (P > 0.05). The rate of lateral wall perforation was higher along trajectory P than trajectory I (29.4 % versus 8.8 %, P < 0.05). There were no differences between trajectory P and trajectory I in the rates of medial, superior or inferior wall perforation (P > 0.05).
a Post-operative CT images of C1 pedicles screw along TP and TI. The right screw along TP perforates the lateral wall of C1 pedicle. The left screw along TI is fully in the pedicle without perforation. b, c Post-operative anteriorposterior and lateral X-rays of C1 pedicles screw. The right screw along TP and the left along TI
Discussion
The technique of C1 pedicle screw placement was initially developed by Resnick and Benzel [17]: the screw was inserted through the posterior arch or “pedicle” into the lateral mass. Since then, multiple studies have investigated the anatomy and feasibility of C1 pedicle screw placement [10–12, 18–22]. Most investigations insisted that the mediolateral width at the isthmus of the C1 pedicle was large enough to insert a 3.5-mm diameter screw [11, 12]. In fact, these authors measured the external pedicle wall width, including the cortex thickness and medullary cavity width of C1 posterior arch. Gebauer et al. [12] reported that the width of the posterior arch at the vertebral artery (VA) groove was 9.8 ± 1.7 mm for males and 8.9 ± 0.7 mm for females. Meanwhile, Ma et al. [11] found that it was on average 8.46 ± 0.57 mm. In our research, external pedicle wall width along trajectory P was 9.3 ± 1.5 mm for males and 7.0 ± 1.6 mm for females, also greater than 3.5-mm or 4.0-mm screw diameter, in agreement with the studies published by Gebauer et al. and Ma et al. The external pedicle wall width along trajectory I was even greater than that along trajectory P, due to larger available mediolateral width.
However, it has been demonstrated that the stability of cervical pedicle screw largely depends on the internal characteristics of the pedicle, and not so much on its external dimensions [23]. Unfortunately, reports on the C1 pedicle’s medullary cavity width are scarce. In recent years, multiplanar CT renders possibility of the precise measurement of the inner as well as outer pedicle diameters [24]. Measurement of C1 pedicle’s medullary cavity width on axial CT image is becoming more and more important for choosing an optimal trajectory, and evaluating the safety of C1 pedicle screw trajectory.
Different from sub-axial cervical vertebra, the vertebral canal of C1 consists of two parts, which contains the odontoid process and the spinal cord. So we designed two trajectories named trajectory P and trajectory I for C1 pedicle screw insertion. As demonstrated above, the rate of lateral wall perforation was higher along trajectory P (29.4 %) than trajectory I (8.8 %). Two reasons could explain these differences. First, the medullary cavity width along trajectory P is lesser than that along trajectory I by 1.4 mm; in addition, medullary cavity width <3.5 mm was found in 16.1 % of pedicles along trajectory P, and only 2.9 % along trajectory I. Another reason is that the lateral wall of C1 pedicle is thinner than the medial wall, similar to sub-axial cervical vertebra [23–25]. As a result, the lateral wall perforation is more frequent than the medial one. If trajectory P is not wide enough to contain a pedicle screw, trajectory I would be a better choice. In fact, any trajectory with entry points from trajectory P to trajectory I and introversion direction from parallel to C1 midline to parallel to the lateral border tangent to the odontoid foramen and vertebral canal of C1 could insert pedicle screw. If a trajectory with small transverse angle could not contain a 3.5-mm diameter pedicle screw, more adequate introversion of the transverse angle with more lateral entry points could make a wider medullary cavity width in order to minimize the risk of lateral wall perforation. The individual maximum medial inclination angle might be transverse angle of trajectory I measured pre-operatively on CT images.
Numerous studies have indicated that the limited superior-inferior height of C1 posterior arch under the vertebral artery groove restricts C1 pedicle screw application [18–20]. If the height is less than 3.5 or 4.0 mm screw diameter, the superior or inferior wall would be penetrated during screw placement. Our research demonstrated that the superior-inferior height of the posterior arch under the vertebral artery groove was 4.3 ± 0.9 mm, which was similar to data reported by Ma et al. [18] and Qian et al.[19] The superior-inferior height of the posterior arch <3.5 mm screw diameter was found 22.0 % (15/68) of pedicles. However, the main handicap to C1 pedicle screw insertion was injury of the VA running along the vertebral artery groove, or venous plexus and C2 nerve root. Deviant direction of pedicle screw insertion on sagittal plane would result in penetration of the posterior arch even with superior-inferior height of the posterior arch larger than screw diameter. We took a measurement to prevent injury of the neurovascular structure. Superior and inferior wall of C1 posterior arch could be subperiosteally dissected. Then, the direction of C1 pedicle on sagittal plane was evident. Drilling holes along the C1 pedicle trajectory and screw insertion could be performed following this direction.
Many researchers agreed that the C1 posterior arches could be divided into four different categories: superficial groove, deep groove, semi-foramen–shaped, and foramen-shaped [18, 21]. In the latter three categories, the superior wall of the posterior arch is difficult to be subperiosteally dissected. However, we found that the superior wall of the C1 posterior arch was flat along trajectory I and groove-shaped along trajectory P, likely because the C1 lamina became gradually thin laterally (Fig. 3). This was in agreement with Kim et al. [22], who showed that orientation of C1 lamina was changed from vertical to horizontal direction in the posterior view. Therefore, exposure of the superior wall of the C1 posterior arch by subperiosteum dissection was easier along trajectory I than trajectory P. Inferior wall of C1 posterior arch could also be subperiosteally dissected. They were useful to determine sagittal direction of pedicle screw insertion and avoid inferior or superior wall perforation.
Several limitations of the current study should also be mentioned. Limited to the number of cadavers, the data of the study are primarily used only as a reference. More measurements could be taken to minimize the deviation of C1 pedicle screw insertion from preoperatively determined direction on CT images. In addition, clinical researches need to be performed on the safety and possibility of pedicle screw insertion along different trajectories.
Conclusion
C1 pedicle screw trajectory with more medial inclination of the transverse angle and more lateral entry points could make a wider medullary cavity compared with the trajectory perpendicular to the coronal plane. The maximum medial inclination might be the transverse angle of trajectory I measured preoperatively on CT images. Neurovascular injury could be avoided by exposing the superior and inferior walls with careful subperiosteum dissection.
References
Dickman CA, Sonntag VK (1995) Surgical management of atlantoaxial nonunions. J Neurosurg 83(2):248–253. doi:10.3171/jns.1995.83.2.0248
Grob D, Crisco JJ 3rd, Panjabi MM, Wang P, Dvorak J (1992) Biomechanical evaluation of four different posterior atlantoaxial fixation techniques. Spine 17(5):480–490
Montesano PX, Juach EC, Anderson PA, Benson DR, Hanson PB (1991) Biomechanics of cervical spine internal fixation. Spine 16(3 Suppl):S10–S16
Glynn MK, Sheehan JM (1983) Fusion of the cervical spine for instability. Clin Orthop Relat Res 179:97–101
Fielding JW, Hensinger RN, Hawkins RJ (1980) Os Odontoideum. J Bone Joint Surg Am 62(3):376–383
Griswold DM, Albright JA, Schiffman E, Johnson R, Southwick W (1978) Atlanto-axial fusion for instability. J Bone Joint Surg Am 60(3):285–292
Husby J, Sorensen KH (1974) Fracture of the odontoid process of the axis. Acta Orthop Scand 45(2):182–192
Schatzker J, Rorabeck CH, Waddell JP (1971) Fractures of the dens (odontoid process). An analysis of thirty-seven cases. J Bone Joint Surg Br 53(3):392–405
Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Xiang M, Zhao WD, Zhong SZ (2009) C1 pedicle screws versus C1 lateral mass screws: comparisons of pullout strengths and biomechanical stabilities. Spine 34(4):371–377. doi:10.1097/BRS.0b013e318193a21b
Tan M, Wang H, Wang Y, Zhang G, Yi P, Li Z, Wei H, Yang F (2003) Morphometric evaluation of screw fixation in atlas via posterior arch and lateral mass. Spine 28(9):888–895. doi:10.1097/01.brs.0000058719.48596.cc
Ma XY, Yin QS, Wu ZH, Xia H, Liu JF, Zhong SZ (2005) Anatomic considerations for the pedicle screw placement in the first cervical vertebra. Spine 30(13):1519–1523
Gebauer M, Barvencik F, Briem D, Kolb JP, Seitz S, Rueger JM, Puschel K, Amling M (2010) Evaluation of anatomic landmarks and safe zones for screw placement in the atlas via the posterior arch. Eur Spine J 19(1):85–90. doi:10.1007/s00586-009-1181-8
Squires J, Molinari RW (2010) C1 lateral mass screw placement with intentional sacrifice of the C2 ganglion: functional outcomes and morbidity in elderly patients. Eur Spine J 19(8):1318–1324. doi:10.1007/s00586-010-1452-4
Hu Y, Kepler CK, Albert TJ, Yuan ZS, Ma WH, Gu YJ, Xu RM (2013) Accuracy and complications associated with the freehand C-1 lateral mass screw fixation technique: a radiographic and clinical assessment. J Neurosurg Spine 18(4):372–377. doi:10.3171/2013.1.spine12724
Lee SH, Kim KT, Suk KS, Lee JH, Son ES, Kwack YH, Oh HS (2012) Assessment of pedicle perforation by the cervical pedicle screw placement using plain radiographs: a comparison with computed tomography. Spine 37(4):280–285. doi:10.1097/BRS.0b013e31822338ad
Nakashima H, Yukawa Y, Imagama S, Kanemura T, Kamiya M, Yanase M, Ito K, Machino M, Yoshida G, Ishikawa Y, Matsuyama Y, Ishiguro N, Kato F (2012) Complications of cervical pedicle screw fixation for nontraumatic lesions: a multicenter study of 84 patients. J Neurosurg Spine 16(3):238–247. doi:10.3171/2011.11.spine11102
Resnick DK, Benzel EC (2002) C1-C2 pedicle screw fixation with rigid cantilever beam construct: case report and technical note. Neurosurgery 50(2):426–428
He F, Yin Q, Zhao T (2008) Classification of atlas pedicles and methodological study of pedicle screw fixation. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 22(8):905–909
Qian LX, Hao DJ, He BR, Jiang YH (2013) Morphology of the atlas pedicle revisited: a morphometric CT-based study on 120 patients. Eur Spine J 22(5):1142–1146. doi:10.1007/s00586-013-2662-3
Huang DG, He SM, Pan JW, Hui H, Hu HM, He BR, Li H, Zhang XF, Hao DJ (2014) Is the 4 mm height of the vertebral artery groove really a limitation of C1 pedicle screw insertion? Eur Spine J 23(5):1109–1114. doi:10.1007/s00586-014-3217-y
Pei-Feng J, Li-Ping W, Ji-Hong F, Yi-Kai L, Manas D (2011) Morphological asymmetry of the atlas and its clinical implications. J Manip Physiol Ther 34(7):463–467. doi:10.1016/j.jmpt.2011.05.003
Kim JH, Kwak DS, Han SH, Cho SM, You SH, Kim MK (2013) Anatomic consideration of the C1 laminar arch for lateral mass screw fixation via C1 lateral lamina: a landmark between the lateral and posterior lamina of the C1. J Kor Neurosurg Soc 54(1):25–29. doi:10.3340/jkns.2013.54.1.25
Panjabi MM, Shin EK, Chen NC, Wang JL (2000) Internal morphology of human cervical pedicles. Spine 25(10):1197–1205
Reinhold M, Magerl F, Rieger M, Blauth M (2007) Cervical pedicle screw placement: feasibility and accuracy of two new insertion techniques based on morphometric data. Eur Spine J 16(1):47–56. doi:10.1007/s00586-006-0104-1
Neo M, Sakamoto T, Fujibayashi S, Nakamura T (2005) The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine 30(24):2800–2805
Acknowledgments
This work was supported by National Natural Science Foundation of China (No. 81371968), and the Foundation of Jiangsu Province Public Health Bureau of China (No. BK2012718).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Jun Ma, Jian Tang and Deguang Wang contributed equally to this work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ma, J., Tang, J., Wang, D. et al. Comparison of perpendicular to the coronal plane versus medial inclination for atlas pedicle screw insertion: an anatomic and radiological study in human cadavers. International Orthopaedics (SICOT) 40, 141–147 (2016). https://doi.org/10.1007/s00264-015-2947-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-015-2947-8