Abstract
Purpose
To compare conventional and dual-energy CT (DECT) for the diagnosis of acute cholecystitis and gangrene.
Methods
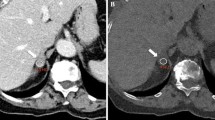
Fifty-seven consecutive adult patients with abdominal pain who underwent IV contrast-enhanced abdominal DECT on a dual-layer (dlDECT) or rapid-switching (rsDECT) scanner from September, 2018 to April, 2021 with cholecystectomy and pathology-confirmed cholecystitis were retrospectively reviewed, and compared with 57 consecutive adult patients without cholecystitis from the same interval scanned with DECT. Images were reviewed independently by two abdominal radiologists with 12 and 16 years of experience in two sessions 4 weeks apart, blinded to clinical data. Initially, only blended reconstructions (simulating conventional single-energy CT images) were reviewed (CT). Subsequently, CT and DECT reconstructions including low-keV virtual monoenergetic images and iodine maps were reviewed. Gallbladder fossa hyperemia, pericholecystic fluid, subjective presence of gangrene, heterogeneous wall enhancement, sloughed membranes, intramural air, abscess, overall impression of the presence of acute cholecystitis, and intramural iodine density were assessed.
Results
Gallbladder fossa hyperemia was detected with increased sensitivity on DECT (R1, 61.4%; R2, 75.4%) vs. CT (R1, 22.8%; R2, 15.8%). DECT showed increased sensitivity for gangrene (R1, 24.6%; R2, 38.6%) vs. CT (R1, 5.3%; R2, 14%), heterogeneous wall enhancement (DECT: R1, 33.3%; R2, 63.2% vs. CT: R1, 7%; R2, 31.6%), and cholecystitis (DECT: R1, 86%; R2, 89.5% vs. CT: R1, 77.2%; R2, 70.2%). In addition, DECT was more sensitive for the detection of acute cholecystitis (R1, 86%; R2, 89.5%) vs. CT (R1, 77.2%; R2, 70.2%). Iodine density threshold of 1.2 mg/ml, 0.8 mg/mL, and 0.5 mg/mL showed specificity for gangrenous cholecystitis of 78.26%, 86.96%, and 95.65%, respectively, using the rsDECT platform.
Conclusion
DECT showed improved sensitivity compared to conventional CT for detection of acute cholecystitis. Iodine density measurements may be helpful to diagnose gangrene.


Similar content being viewed by others
References
Wertz, J.R., Lopez, J.M., Olson, D. and Thompson, W.M., 2018. Comparing the diagnostic accuracy of ultrasound and CT in evaluating acute cholecystitis. American Journal of Roentgenology, 211(2), pp.W92-W97. https://doi.org/10.2214/AJR.17.18884
Bennett, G.L. and Balthazar, E.J., 2003. Ultrasound and CT evaluation of emergent gallbladder pathology. Radiologic Clinics, 41(6), pp.1203–1216. https://www.radiologic.theclinics.com/article/S0033-8389(03)00097-6/abstract
Pinto A, Romano S, Del Vecchio W, et al. (2000) Personal experience in 71 consecutive patients with acute cholecystitis. Radiol Med (Torino) 99:62–67. https://europepmc.org/article/med/10803189
Bennett, G.L. and Balthazar, E.J., 2003. Ultrasound and CT evaluation of emergent gallbladder pathology. Radiologic Clinics, 41(6), pp.1203–1216. https://jamanetwork.com/journals/jamasurgery/article-abstract/566942
Mentzer Jr, R.M., Golden, G.T., Chandler, J.G. and Horsley 3rd, J.S., 1975. A comparative appraisal of emphysematous cholecystitis. American journal of surgery, 129(1), pp.10–15. https://europepmc.org/article/med/174453
Fry, D.E., Cox, R.A. and Harbrecht, P.J., 1981. Gangrene of the gallbladder: a complication of acute cholecystitis. Southern medical journal, 74(6), pp.666–668. https://europepmc.org/article/med/7244741
Cotran, R.S. and Kumar, V., 1989. Robbins pathologic basis of disease. WB Saunders Company. Philadelphia, PA.
Fuks, D., Mouly, C., Robert, B., Hajji, H., Yzet, T. and Regimbeau, J.M., 2012. Acute cholecystitis: preoperative CT can help the surgeon consider conversion from laparoscopic to open cholecystectomy. Radiology, 263(1), pp.128-138. https://doi.org/10.1148/radiol.12110460
Baird, D.R., Wilson, J.P., Mason, E.M., Duncan, T.D., Evans, J.S., Luke, J.P., Ruben, D.M. and Lucas, G.W., 1992. An early review of 800 laparoscopic cholecystectomies at a university-affiliated community teaching hospital. The American surgeon, 58(3), pp.206–210. https://europepmc.org/article/med/1532704
Bennett, G.L., Rusinek, H., Lisi, V., Israel, G.M., Krinsky, G.A., Slywotzky, C.M. and Megibow, A., 2002. CT findings in acute gangrenous cholecystitis. American Journal of Roentgenology, 178(2), pp.275–281. https://www.ajronline.org/doi/full/https://doi.org/10.2214/ajr.178.2.1780275
Singh, A.K. and Sagar, P., 2005. Gangrenous cholecystitis: prediction with CT imaging. Abdominal imaging, 30(2), pp.218-221. https://doi.org/10.1007/s00261-004-0217-0
Nguyen, L., Fagan, S.P., Lee, T.C., Aoki, N., Itani, K.M., Berger, D.H. and Awad, S.S., 2004. Use of a predictive equation for diagnosis of acute gangrenous cholecystitis. The American journal of surgery, 188(5), pp.463–466. https://www.sciencedirect.com/science/article/abs/pii/S0002961004003459
Teefey, S.A., Dahiya, N., Middleton, W.D., Bajaj, S., Dahiya, N., Ylagan, L. and Hildebolt, C.F., 2013. Acute cholecystitis: do sonographic findings and WBC count predict gangrenous changes? American Journal of Roentgenology, 200(2), pp.363-369. https://doi.org/10.2214/AJR.12.8956
Kiviluoto T, Siren J, Luukkonen P, et al. Randomised trial of laparoscopic versus open cholecystectomy for acute and gangrenous cholecystitis. Lancet 1998; 351:321–325. https://www.sciencedirect.com/science/article/abs/pii/S014067369708447X
Chang, W.C., Sun, Y., Wu, E.H., Kim, S.Y., Wang, Z.J., Huang, G.S. and Yeh, B.M., 2016. CT findings for detecting the presence of gangrenous ischemia in cholecystitis. American Journal of Roentgenology, 207(2), pp.302-309. https://doi.org/10.2214/AJR.15.15658
Murphy KP, Darras KE, Nicolaou S, McLaughlin PD. 2016 Oct. Emergency abdominal applications of DECT. Current Radiology Reports. 1;4(10):54. https://www.researchgate.net/publication/306308602_Emergency_Abdominal_Applications_of_DECT
Fitzgibbons RJ, Tseng A, Wang H, Ryberg A, Nguyen N, Sims KL. 1996 Dec. Acute cholecystitis. Surgical endoscopy. 10(12):1180–4. https://pubmed.ncbi.nlm.nih.gov/8939838/
Jacobsen, M.C., Schellingerhout, D., Wood, C.A., Tamm, E.P., Godoy, M.C., Sun, J. and Cody, D.D., 2018. Intermanufacturer comparison of dual-energy CT iodine quantification and monochromatic attenuation: a phantom study. Radiology, 287(1), pp.224-234. https://doi.org/10.1148/radiol.2017170896
Landis JR, Koch GG. 1977. The measurement of observer agreement for categorical data. Biometrics, 33 (1), pp. 159-174
Fidler, J., Paulson, E.K. and Layfield, L., 1996. CT evaluation of acute cholecystitis: findings and usefulness in diagnosis. AJR. American journal of roentgenology, 166(5), pp.1085-1088. https://doi.org/10.2214/ajr.166.5.8615248
Kane RA, Costello P, Duszlak E. Computed tomography in acute cholecystitis: new observations. AJR 1983; 141:697–701. https://doi.org/10.2214/ajr.141.4.697
Yamashita, K., Jin, M.J., Hirose, Y., Morikawa, M., Sumioka, H., Itoh, K. and Konish, J., 1995. CT finding of transient focal increased attenuation of the liver adjacent to the gallbladder in acute cholecystitis. AJR. American journal of roentgenology, 164(2), pp.343-346. https://doi.org/10.2214/ajr.164.2.7839966
Bennett, G.L., 2015. Evaluating patients with right upper quadrant pain. Radiologic Clinics, 53(6), pp.1093–1130.https://www.radiologic.theclinics.com/article/S0033-8389(15)00132-3/abstract
Wu, C.H., Chen, C.C., Wang, C.J., Wong, Y.C., Wang, L.J., Huang, C.C., Lo, W.C. and Chen, H.W., 2011. Discrimination of gangrenous from uncomplicated acute cholecystitis: accuracy of CT findings. Abdominal imaging, 36(2), pp.174-178. https://doi.org/10.1007/s00261-010-9612-x
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
This research study was conducted retrospectively from data obtained for clinical purposes. We consulted extensively with the IRB of Boston University Medical Center who determined that our study did not need ethical approval. An IRB official waiver of ethical approval was granted from the IRB of Boston University Medical Center (IRB Number: H-39858).
Informed consent
The IRB waived informed consent for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huda, F., LeBedis, C.A., Qureshi, M.M. et al. Acute cholecystitis: diagnostic value of dual-energy CT-derived iodine map and low-keV virtual monoenergetic images. Abdom Radiol 46, 5125–5133 (2021). https://doi.org/10.1007/s00261-021-03202-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-021-03202-9