Abstract
Retroperitoneal soft tissue lesions represent a wide range of disease processes with overlapping imaging findings. Familiarity with the CT and MR characteristics of these conditions is important to guide clinical evaluation. We review the tissue types, characteristic clinical, demographic, and imaging features of retroperitoneal tumors and tumor-like non-neoplastic conditions with CT and MR correlation, including anatomic and imaging clues, and provide a diagnostic approach to aide the radiologist in making a specific diagnosis.
















Similar content being viewed by others
References
Mota M, Bezerra ROF, Garcia MRT (2018) Practical approach to primary retroperitoneal masses in adults. Radiol Bras 51 (6):391-400. https://doi.org/10.1590/0100-3984.2017.0179
Goenka AH, Shah SN, Remer EM (2012) Imaging of the retroperitoneum. Radiol Clin North Am 50 (2):333-355, vii. https://doi.org/10.1016/j.rcl.2012.02.004
Elsayes KM, Staveteig PT, Narra VR, Chen ZM, Moustafa YL, Brown J (2007) Retroperitoneal masses: magnetic resonance imaging findings with pathologic correlation. Curr Probl Diagn Radiol 36 (3):97-106. https://doi.org/10.1067/j.cpradiol.2006.12.003
Scali EP, Chandler TM, Heffernan EJ, Coyle J, Harris AC, Chang SD (2015) Primary retroperitoneal masses: what is the differential diagnosis? Abdom Imaging 40 (6):1887-1903. https://doi.org/10.1007/s00261-014-0311-x
Rajiah P, Sinha R, Cuevas C, Dubinsky TJ, Bush WH, Jr., Kolokythas O (2011) Imaging of uncommon retroperitoneal masses. Radiographics 31 (4):949-976. https://doi.org/10.1148/rg.314095132
Nishino M, Hayakawa K, Minami M, Yamamoto A, Ueda H, Takasu K (2003) Primary retroperitoneal neoplasms: CT and MR imaging findings with anatomic and pathologic diagnostic clues. Radiographics 23 (1):45-57. https://doi.org/10.1148/rg.231025037
Shaaban AM, Rezvani M, Tubay M, Elsayes KM, Woodward PJ, Menias CO (2016) Fat-containing Retroperitoneal Lesions: Imaging Characteristics, Localization, and Differential Diagnosis. Radiographics 36 (3):710-734. https://doi.org/10.1148/rg.2016150149
Craig WD, Fanburg-Smith JC, Henry LR, Guerrero R, Barton JH (2009) Fat-containing lesions of the retroperitoneum: radiologic-pathologic correlation. Radiographics 29 (1):261-290. https://doi.org/10.1148/rg.291085203
Jagannathan JP, Tirumani SH, Ramaiya NH (2016) Imaging in Soft Tissue Sarcomas: Current Updates. Surg Oncol Clin N Am 25 (4):645-675. https://doi.org/10.1016/j.soc.2016.05.002
Elnemr A, Yonemura Y, Shinbo M, Nishino E (2010) Primary retroperitoneal mullerian adenocarcinoma. Rare Tumors 2 (1):e6. https://doi.org/10.4081/rt.2010.e6
Weiss SW (1996) Lipomatous tumors. Monogr Pathol 38:207-239
Fiore M, Grosso F, Lo Vullo S, Pennacchioli E, Stacchiotti S, Ferrari A, Collini P, Lozza L, Mariani L, Casali PG, Gronchi A (2007) Myxoid/round cell and pleomorphic liposarcomas: prognostic factors and survival in a series of patients treated at a single institution. Cancer 109 (12):2522-2531. https://doi.org/10.1002/cncr.22720
Hekimoglu K (2013) Giant retroperitoneal liposarcomas: diagnostic approach with multidetector computed tomography and magnetic resonance imaging. Jbr-Btr 96 (6):375-377. https://doi.org/10.5334/jbr-btr.466
Ghadimi MP, Al-Zaid T, Madewell J, Peng T, Colombo C, Hoffman A, Creighton CJ, Zhang Y, Zhang A, Lazar AJ, Pollock RE, Lev D (2011) Diagnosis, management, and outcome of patients with dedifferentiated liposarcoma systemic metastasis. Ann Surg Oncol 18 (13):3762-3770. https://doi.org/10.1245/s10434-011-1794-0
Baheti AD, O’Malley RB, Kim S, Keraliya AR, Tirumani SH, Ramaiya NH, Wang CL (2016) Soft-Tissue Sarcomas: An Update for Radiologists Based on the Revised 2013 World Health Organization Classification. AJR Am J Roentgenol 206 (5):924-932. https://doi.org/10.2214/AJR.15.15498
Levy AD, Manning MA, Al-Refaie WB, Miettinen MM (2017) Soft-Tissue Sarcomas of the Abdomen and Pelvis: Radiologic-Pathologic Features, Part 1-Common Sarcomas: From the Radiologic Pathology Archives. Radiographics 37 (2):462-483. https://doi.org/10.1148/rg.2017160157
Lahat G, Madewell JE, Anaya DA, Qiao W, Tuvin D, Benjamin RS, Lev DC, Pollock RE (2009) Computed tomography scan-driven selection of treatment for retroperitoneal liposarcoma histologic subtypes. Cancer 115 (5):1081-1090. https://doi.org/10.1002/cncr.24045
Kim EY, Kim SJ, Choi D, Lee SJ, Kim SH, Lim HK, Song SY (2008) Recurrence of retroperitoneal liposarcoma: imaging findings and growth rates at follow-up CT. AJR Am J Roentgenol 191 (6):1841-1846. https://doi.org/10.2214/AJR.07.3746
Kim T, Murakami T, Oi H, Tsuda K, Matsushita M, Tomoda K, Fukuda H, Nakamura H (1996) CT and MR imaging of abdominal liposarcoma. AJR Am J Roentgenol 166 (4):829-833. https://doi.org/10.2214/ajr.166.4.8610559
Hong SH, Kim KA, Woo OH, Park CM, Kim CH, Kim MJ, Chung JJ, Han JK, Rha SE (2010) Dedifferentiated liposarcoma of retroperitoneum: spectrum of imaging findings in 15 patients. Clin Imaging 34 (3):203-210. https://doi.org/10.1016/j.clinimag.2009.12.025
Cooley CL, Jagannathan JP, Kurra V, Tirumani SH, Saboo SS, Ramaiya NH, Shinagare AB (2014) Imaging features and metastatic pattern of non-IVC retroperitoneal leiomyosarcomas: are they different from IVC leiomyosarcomas? J Comput Assist Tomogr 38 (5):687-692. https://doi.org/10.1097/RCT.0000000000000097
Abraham JA, Weaver MJ, Hornick JL, Zurakowski D, Ready JE (2012) Outcomes and prognostic factors for a consecutive case series of 115 patients with somatic leiomyosarcoma. J Bone Joint Surg Am 94 (8):736-744. https://doi.org/10.2106/JBJS.K.00460
Ganeshalingam S, Rajeswaran G, Jones RL, Thway K, Moskovic E (2011) Leiomyosarcomas of the inferior vena cava: diagnostic features on cross-sectional imaging. Clin Radiol 66 (1):50-56. https://doi.org/10.1016/j.crad.2010.08.004
O’Sullivan PJ, Harris AC, Munk PL (2008) Radiological imaging features of non-uterine leiomyosarcoma. Br J Radiol 81 (961):73-81. https://doi.org/10.1259/bjr/18595145
Yakupoglu A, Ulus S, Cantasdemir M (2016) Leiomyosarcoma of the Inferior Vena Cava Confirmed by Aspiration Biopsy With a Catheter During Digital Subtraction Angiography. Vasc Endovascular Surg 50 (3):164-167. https://doi.org/10.1177/1538574416637445
Huang J, Liu Q, Lu JP, Wang F, Wang L, Jin AG (2011) Primary intraluminal leiomyosarcoma of the inferior vena cava: value of MRI with contrast-enhanced MR venography in diagnosis and treatment. Abdom Imaging 36 (3):337-341. https://doi.org/10.1007/s00261-010-9656-y
Brennan MF, Antonescu CR, Alektiar KM, Maki RG (2016) Undifferentiated Pleomorphic Sarcoma (UPS) (Malignant Fibrous Histiocytoma (MFH) and Myxofibrosarcoma). In: Management of Soft Tissue Sarcoma. Springer International Publishing, Cham, pp 143-152. https://doi.org/10.1007/978-3-319-41906-0_7
Cong Z, Gong J (2011) Primary malignant fibrous histiocytoma of the liver: CT findings in five histopathological proven patients. Abdom Imaging 36 (5):552-556. https://doi.org/10.1007/s00261-011-9691-3
Osman S, Lehnert BE, Elojeimy S, Cruite I, Mannelli L, Bhargava P, Moshiri M (2013) A comprehensive review of the retroperitoneal anatomy, neoplasms, and pattern of disease spread. Curr Probl Diagn Radiol 42 (5):191-208. https://doi.org/10.1067/j.cpradiol.2013.02.001
Kim KH, Lee SH, Cha SH, Kim YS, Sung DJ (2012) Malignant fibrous histiocytoma arising from a hydronephrotic kidney: a case report and review of the literature. Clin Imaging 36 (3):239-242. https://doi.org/10.1016/j.clinimag.2011.09.001
Lee SY, Jee WH, Jung JY, Park MY, Kim SK, Jung CK, Chung YG (2016) Differentiation of malignant from benign soft tissue tumours: use of additive qualitative and quantitative diffusion-weighted MR imaging to standard MR imaging at 3.0 T. Eur Radiol 26 (3):743-754. https://doi.org/10.1007/s00330-015-3878-x
Gaballah AH, Jensen CT, Palmquist S, Pickhardt PJ, Duran A, Broering G, Elsayes KM (2017) Angiosarcoma: clinical and imaging features from head to toe. Br J Radiol 90 (1075):20170039. https://doi.org/10.1259/bjr.20170039
Sung CK, Kim B, Moon KC, Ku JH, Ha SB (2017) Retroperitoneal Tumors. In: Kim SH, Cho JY (eds) Oncologic Imaging: Urology. Springer Berlin Heidelberg, Berlin, Heidelberg, pp 227-260. https://doi.org/10.1007/978-3-662-45218-9_6
Miao C, Luo C-H (2018) Retroperitoneal Rhabdomyosarcoma. In: Luo C-H (ed) Retroperitoneal Tumors. Springer Netherlands, Dordrecht, pp 183-184. https://doi.org/10.1007/978-94-024-1167-6_17
Miao C, Luo C-H (2018) Retroperitoneal Synovial Sarcoma. In: Luo C-H (ed) Retroperitoneal Tumors. Springer Netherlands, Dordrecht, pp 259-261. https://doi.org/10.1007/978-94-024-1167-6_33
Thway K, Fisher C (2015) PEComa: morphology and genetics of a complex tumor family. Ann Diagn Pathol 19 (5):359-368. https://doi.org/10.1016/j.anndiagpath.2015.06.003
Crino PB, Nathanson KL, Henske EP (2006) The tuberous sclerosis complex. N Engl J Med 355 (13):1345-1356. https://doi.org/10.1056/NEJMra055323
Phillips CH, Keraliya AR, Shinagare AB, Ramaiya NH, Tirumani SH (2016) Update on the imaging of malignant perivascular epithelioid cell tumors (PEComas). Abdom Radiol (NY) 41 (2):368-376. https://doi.org/10.1007/s00261-015-0568-8
Liang W, Xu C, Chen F (2015) Primary retroperitoneal perivascular epithelioid cell neoplasm: A case report. Oncol Lett 10 (1):469-472. https://doi.org/10.3892/ol.2015.3210
Hedgire SS, Kudrimoti S, Oliveira IS, Nadkarni N, McDermott S, Hahn PF, Mino-Kenudson M, Harisinghani MG (2017) Extranodal lymphomas of abdomen and pelvis: imaging findings and differential diagnosis. Abdom Radiol (NY) 42 (4):1096-1112. https://doi.org/10.1007/s00261-016-0964-8
Rosenkrantz AB, Spieler B, Seuss CR, Stifelman MD, Kim S (2012) Utility of MRI features for differentiation of retroperitoneal fibrosis and lymphoma. AJR Am J Roentgenol 199 (1):118-126. https://doi.org/10.2214/AJR.11.7822
Neville A, Herts BR (2004) CT characteristics of primary retroperitoneal neoplasms. Crit Rev Comput Tomogr 45 (4):247-270
Rha SE, Byun JY, Jung SE, Chun HJ, Lee HG, Lee JM (2003) Neurogenic tumors in the abdomen: tumor types and imaging characteristics. Radiographics 23 (1):29-43. https://doi.org/10.1148/rg.231025050
MJ, Thomas JM, Fisher C, Moskovic EC (2005) Imaging features of retroperitoneal and pelvic schwannomas. Clin Radiol 60 (8):886-893. https://doi.org/10.1016/j.crad.2005.01.016
Erickson D, Kudva YC, Ebersold MJ, Thompson GB, Grant CS, van Heerden JA, Young WF, Jr. (2001) Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. J Clin Endocrinol Metab 86 (11):5210-5216. https://doi.org/10.1210/jcem.86.11.8034
Lonergan GJ, Schwab CM, Suarez ES, Carlson CL (2002) Neuroblastoma, ganglioneuroblastoma, and ganglioneuroma: radiologic-pathologic correlation. Radiographics 22 (4):911-934. https://doi.org/10.1148/radiographics.22.4.g02jl15911
Choyke PL, Hayes WS, Sesterhenn IA (1993) Primary extragonadal germ cell tumors of the retroperitoneum: differentiation of primary and secondary tumors. Radiographics 13 (6):1365-1375; quiz 1377-1368. https://doi.org/10.1148/radiographics.13.6.8290730
Keitoku M, Konishi I, Nanbu K, Yamamoto S, Mandai M, Kataoka N, Oishi T, Mori T (1997) Extraovarian sex cord-stromal tumor: case report and review of the literature. Int J Gynecol Pathol 16 (2):180-185. https://doi.org/10.1097/00004347-199704000-00017
Trabelsi A, Ben Abdelkarim S, Hadfi M, Fatnaci R, Stita W, Sriha B, Korbi S (2008) Primary mesenteric Sertoli–Leydig cell tumor: a case report and review of the literature. J Oncol 2008:619637. https://doi.org/10.1155/2008/619637
Ueno T, Tanaka YO, Nagata M, Tsunoda H, Anno I, Ishikawa S, Kawai K, Itai Y (2004) Spectrum of germ cell tumors: from head to toe. Radiographics 24 (2):387-404. https://doi.org/10.1148/rg.242035082
Gatcombe HG, Assikis V, Kooby D, Johnstone PA (2004) Primary retroperitoneal teratomas: a review of the literature. J Surg Oncol 86 (2):107-113. https://doi.org/10.1002/jso.20043
Davidson AJ, Hartman DS, Goldman SM (1989) Mature teratoma of the retroperitoneum: radiologic, pathologic, and clinical correlation. Radiology 172 (2):421-425. https://doi.org/10.1148/radiology.172.2.2664866
Mathur P, Lopez-Viego MA, Howell M (2010) Giant primary retroperitoneal teratoma in an adult: a case report. Case Rep Med 2010. https://doi.org/10.1155/2010/650424
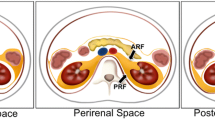
Surabhi VR, Menias C, Prasad SR, Patel AH, Nagar A, Dalrymple NC (2008) Neoplastic and non-neoplastic proliferative disorders of the perirenal space: cross-sectional imaging findings. Radiographics 28 (4):1005-1017. https://doi.org/10.1148/rg.28407515
Mesurolle B, Sayag E, Meingan P, Lasser P, Duvillard P, Vanel D (1996) Retroperitoneal extramedullary hematopoiesis: sonographic, CT, and MR imaging appearance. AJR Am J Roentgenol 167 (5):1139-1140. https://doi.org/10.2214/ajr.167.5.8911166
Georgiades CS, Neyman EG, Francis IR, Sneider MB, Fishman EK (2002) Typical and atypical presentations of extramedullary hemopoiesis. AJR Am J Roentgenol 179 (5):1239-1243. https://doi.org/10.2214/ajr.179.5.1791239
Orphanidou-Vlachou E, Tziakouri-Shiakalli C, Georgiades CS (2014) Extramedullary hemopoiesis. Semin Ultrasound CT MR 35 (3):255-262. https://doi.org/10.1053/j.sult.2013.12.001
Zhou LP, Zhang B, Peng WJ, Yang WT, Guan YB, Zhou KR (2008) Imaging findings of Castleman disease of the abdomen and pelvis. Abdom Imaging 33 (4):482-488. https://doi.org/10.1007/s00261-007-9282-5
Cohn JE, Zhou J, Hu A (2018) Castleman disease. Ear Nose Throat J 97 (8):233-234. https://doi.org/10.1177/014556131809700819
Meador TL, McLarney JK (2000) CT features of Castleman disease of the abdomen and pelvis. AJR Am J Roentgenol 175 (1):115-118. https://doi.org/10.2214/ajr.175.1.1750115
Irsutti M, Paul JL, Selves J, Railhac JJ (1999) Castleman disease: CT and MR imaging features of a retroperitoneal location in association with paraneoplastic pemphigus. Eur Radiol 9 (6):1219-1221. https://doi.org/10.1007/s003300050821
Czeyda-Pommersheim F, Hwang M, Chen SS, Strollo D, Fuhrman C, Bhalla S (2015) Amyloidosis: Modern Cross-sectional Imaging. Radiographics 35 (5):1381-1392. https://doi.org/10.1148/rg.2015140179
Kawashima A, Alleman WG, Takahashi N, Kim B, King BF, Jr., LeRoy AJ (2011) Imaging evaluation of amyloidosis of the urinary tract and retroperitoneum. Radiographics 31 (6):1569-1582. https://doi.org/10.1148/rg.316115519
Acknowledgements
The authors thank Henry Douglas for his help with images.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
CME activity This article has been selected as the CME activity for the current month. Please visit https://ce.mayo.edu/node/103122 and follow the instructions to complete this CME activity.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Video 1: Follicular Lymphoma in a 38-year-old female. Coronal reconstruction of a contrast enhanced abdomen CT cine clip show a large confluent nodal mass (arrows) in the retroperitoneum and the mesenteric root. Note the relatively homogenous (for the size of the nodal mass) contrast enhancement and contiguous but discrete enlarged lymph nodes in the mesentery. The retroperitoneal mass splays and narrows but doesn’t obstruct the right main renal artery (RMRA) and the left main renal artery (LMRA). Supplementary Material 1 (AVI 409318 kb)
Video 2 a,b: Paraganglioma in a 54-year-old male with retroperitoneal mass. A. Axial contrast enhanced CTcine clip shows a heterogeneous but predominantly markedly enhancing mass (M) in the retroperitoneum adjacent to the left kidney and adrenal gland. B. F-18 FDG Body PET-CT fusion cine clip obtained in axial plane demonstrates a very intense uptake in the locally invasive left retroperitoneal mass (SUVmax 26.3, image 145), consistent with malignancy. Supplementary Material 2 (AVI 174740 kb)
Video 3: Germ Cell tumor with retroperitoneal metastases in a 52-year-old male. Coronal T2W MRI cine clip of the abdomen and pelvis shows a large, confluent heterogeneous hyperdense to the skeletal muscle nodal mass (arrows) causing significant displacement of the left kidney (LK) and narrowing of the retroperitoneal vasculature most pronounced of the left renal vein. Note large well-circumscribed primary germ cell tumor in the scrotum. Multiple simple renal cysts are also present. Supplementary Material 3 (AVI 131472 kb)
Supplementary Material 4 (AVI 278170 kb)
Video 4 a, b: Presacral Epidermoid in a 29-year-old female with complex pelvic cyst. A. Sagittal T2 TSE cine clip shows a well-circumscribed lesion (M) with a T2 hypointense wall and T2 hyperintense internal contents in the presacral tissues. The contents are markedly T2 hyperintense due to gross fat. B. Axial T1W FS post-contrast image of the pelvis shows a cystic lesion (M) with a thin, enhancing wall and no internal enhancing components in the presacral tissues. Note that on the fat saturated image the cyst contents show complete signal loss due to gross fat content. Supplementary material 5 (AVI 197048 kb)
Supplementary Material 6 (AVI 371462 kb)
Video 5: Retroperitoneal fibrosis in a middle-aged woman. Contrast-enhanced T1 weighed fat suppressed axial image through the abdomen and pelvis shows enhancing soft tissue encircling the aorta (yellow arrows). Although less noticeable the ureters also were involved resulting in enhancing tissue thickening of the ureteral wall (green arrows) and resulting in ureteral obstruction for which bilateral nephroureteral stents (seen as signal void within the ureter lumen) were placed. The soft tissue tethers the right ovary (red arrow) which is anteriorly displaced. Supplementary material 7 (AVI 116773 kb)
Rights and permissions
About this article
Cite this article
Czeyda-Pommersheim, F., Menias, C., Boustani, A. et al. Diagnostic approach to primary retroperitoneal pathologies: what the radiologist needs to know. Abdom Radiol 46, 1062–1081 (2021). https://doi.org/10.1007/s00261-020-02752-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-020-02752-8