Abstract
Purpose
To investigate incidental pancreatic cysts (IPCs) size discrepancy in a cohort of patients receiving both computed tomography (CT) and magnetic resonance imaging (MRI) and its impact on clinical management based on the 2010 American College of Radiology (ACR) guidelines.
Methods
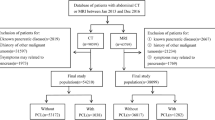
This was a HIPAA-compliant, retrospective, IRB-approved study. Informed consent was waived. Patients with known IPCs and at least one case-pair, consisting of an abdominal CT and MRI examination within 180 days between 05/1999 and 12/2011, were included. Maximum diameter of cysts was measured in both the CT and MR examinations. A subset of 30 patients was measured by three radiologists independently to assess inter-observer variability. Absolute difference in diameter measurements between CT and MRI was calculated. Influence of cyst size, cyst location, and patient characteristics such as weight, height, and body mass index (BMI) on variability of size measurements were evaluated. Clinical impact in terms of current ACR guidelines was assessed.
Results
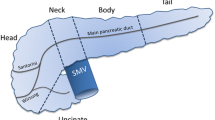
Overall, 267 case-pairs of cysts in 113 patients were included in this study. 59/267 cysts were visualized on MRI but not on CT (22.1%, 95% CI 17.1%–27.1%; 32 patients, 64.6 ± 11.7 years, BMI 28.5 ± 4.8 kg/m2), with a median MRI cyst size of 7.8 mm, IQR 6.0–9.0 mm, range 2–17.8 mm. 208 case-pairs in 113 patients with a mean BMI of 26.9 ± 5.1 kg/m2 (range 16.9–39.5 kg/m2) and mean cysts size of 13.4 ± 8.1 mm (range 3–49 mm) were seen in both CT and MRI. The mean absolute size difference for IPCs measured on MRI and CT was 2.1 ± 1.8 mm (median 1.5 mm, IQR 0.9–2.9 mm, range 0–9 mm). Absolute size difference between CT and MRI measurements increased with size of the cyst (r = 0.31, p < 0.001), whereas location of the cyst did not influence the absolute difference between CT and MRI measurements (p = 0.44). Patient weight and BMI had a negative correlation with the difference in cyst size between CT and MRI (weight r = −0.17, p = 0.023; BMI r = −0.17, p = 0.027), with cyst measurements being larger on MRI in thin patients and on CT in obese patients. Inter-reader variability was excellent (ICC = 0.99). In 12/208 (5.7%, 95% CI 2.7%–9.1%), variability between CT and MRI would have changed ACR-based follow-up recommendation.
Conclusion
There was a median difference of 1.5 mm between measurements of IPCs on CT vs. MRI. If imaging modality was switched during follow-up, variability of measurements may lead to inappropriate change of follow-up regimen in 6% of all cases. A single follow-up CT for incidental IPCs does not seem sufficient due to a high number (22%) of missed IPCs on CT.








Similar content being viewed by others
References
Zaheer A, Pokharel SS, Wolfgang C, Fishman EK, Horton KM (2013) Incidentally detected cystic lesions of the pancreas on CT: review of literature and management suggestions. Abdom Imaging 38(2):331–341
Laffan TA, Horton KM, Klein AP, et al. (2008) Prevalence of unsuspected pancreatic cysts on MDCT. AJR Am J Roentgenol 191(3):802–807
Maimone S, Agrawal D, Pollack MJ, et al. (2010) Variability in measurements of pancreatic cyst size among EUS, CT, and magnetic resonance imaging modalities. Gastrointest Endosc 71(6):945–950
Lee KS, Sekhar A, Rofsky NM, Pedrosa I (2010) Prevalence of incidental pancreatic cysts in the adult population on MR imaging. Am J Gastroenterol 105(9):2079–2084
Zhang X-M, Mitchell DG, Dohke M, Holland GA, Parker L (2002) Pancreatic cysts: depiction on single-shot fast spin-echo MR images. Radiology 223(2):547–553
Ip IK, Mortele KJ, Prevedello LM, Khorasani R (2011) Focal cystic pancreatic lesions: assessing variation in radiologists’ management recommendations. Radiology 259(1):136–141
Dewhurst CE, Mortele KJ (2012) Cystic tumors of the pancreas: imaging and management. Radiol Clin North Am 50(3):467–486
Berland LL, Silverman SG, Gore RM, et al. (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol JACR 7(10):754–773
Tanaka M, Chari S, Adsay V, et al. (2006) International consensus guidelines for management of intraductal papillary mucinous neoplasms and mucinous cystic neoplasms of the pancreas. Pancreatol Off J Int Assoc Pancreatol IAP Al 6(1–2):17–32
Tanaka M, Fernández-del Castillo C, Adsay V, et al. (2012) International consensus guidelines 2012 for the management of IPMN and MCN of the pancreas. Pancreatol Off J Int Assoc Pancreatol IAP Al 12(3):183–197
Vege SS, Ziring B, Jain R, Moayyedi P (2015) Clinical guidelines committee, American gastroenterology association. American gastroenterological association institute guideline on the diagnosis and management of asymptomatic neoplastic pancreatic cysts. Gastroenterology 148(4):819–822
Sahani DV, Kambadakone A, Macari M, et al. (2013) Diagnosis and management of cystic pancreatic lesions. Am J Roentgenol 200(2):343–354
Brook OR, Beddy P, Pahade J, et al. (2016) Delayed growth in incidental pancreatic cysts: are the current American college of radiology recommendations for follow-up appropriate? Radiology 278(3):752–761
Dunn DP, Brook OR, Brook A, et al. (2016) Measurement of pancreatic cystic lesions on magnetic resonance imaging: efficacy of standards in reducing inter-observer variability. Abdom Radiol 41(3):500–507
Waters JA, Schmidt CM, Pinchot JW, et al. (2008) CT vs. MRCP: optimal classification of IPMN type and extent. J Gastrointest Surg Off J Soc Surg Aliment Tract 12(1):101–109
Gupta S, Wagner-Bartak N, Jensen CT, et al. (2016) Dual-energy CT of pancreatic adenocarcinoma: reproducibility of primary tumor measurements and assessment of tumor conspicuity and margin sharpness. Abdom Radiol N Y:1–8
McErlean A, Panicek DM, Zabor EC, et al. (2013) Intra- and interobserver variability in CT measurements in oncology. Radiology 269(2):451–459
Remotti HE, Winner M, Saif MW (2012) Intraductal papillary mucinous neoplasms of the pancreas: clinical surveillance and malignant progression, multifocality and implications of a field-defect. JOP J Pancreas 13(2):135–138
Uehara H, Nakaizumi A, Ishikawa O, et al. (2008) Development of ductal carcinoma of the pancreas during follow-up of branch duct intraductal papillary mucinous neoplasm of the pancreas. Gut 57(11):1561–1565
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they do not have conflict of interest pertaining to this study.
Ethical approval
This study was approved by institutional IRB with waiver of informed consent.
Rights and permissions
About this article
Cite this article
Boos, J., Brook, A., Chingkoe, C.M. et al. MDCT vs. MRI for incidental pancreatic cysts: measurement variability and impact on clinical management. Abdom Radiol 42, 521–530 (2017). https://doi.org/10.1007/s00261-016-0883-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00261-016-0883-8