Abstract
Purpose
Aim of this study was to investigate a dose-response relationship, dose-toxicity relationship, progression free survival (PFS) and overall survival (OS) in neuroendocrine tumour liver metastases (NELM) treated with holmium-166-microspheres radioembolization ([166Ho]-radioembolization).
Materials and methods
Single center, retrospective study included patients with NELM that received [166Ho]-radioembolization with post-treatment SPECT/CT and CECT or MRI imaging for 3 months follow-up. Post-treatment SPECT/CT was used to calculate tumour (Dt) and whole liver healthy tissue (Dh) absorbed dose. Clinical and laboratory toxicity was graded by Common Terminology Criteria for Adverse Events (CTCAE), version 5 at baseline and three-months follow-up. Response was determined according to RECIST 1.1. The tumour and healthy doses was correlated to lesion-based objective response and patient-based toxicity. Kaplan Meier analyses were performed for progression free survival (PFS) and overall survival (OS).
Results
Twenty-seven treatments in 25 patients were included, with a total of 114 tumours. Median follow-up was 14 months (3 – 82 months). Mean Dt in non-responders was 68 Gy versus 118 Gy in responders, p = 0.01. ROC analysis determined 86 Gy to have the highest sensitivity and specificity, resp. 83% and 81%. Achieving a Dt of ≥ 120 Gy provided the highest likelihood of response (90%) for obtaining response. Sixteen patients had grade 1–2 clinical toxicity and only one patient grade 3. No clear healthy liver dose-toxicity relationship was found. The median PFS was 15 months (95% CI [10.2;19.8]) and median OS was not reached.
Conclusion
This study confirms the safety and efficacy of [166Ho]-radioembolization in NELM in a real-world setting. A clear dose–response relationship was demonstrated and future studies should aim at a Dt of ≥ 120 Gy, being predictive of response. No dose-toxicity relationship could be established.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine neoplasms constitute 2% of all malignancies and comprise a very heterogenous group of tumours with diverse clinical behaviour, histology and responses to treatments [1, 2]. Tumour grading is defined on the WHO/ENETS criteria [3]. Neuroendocrine tumours (NET) with a low or intermediate grade (G1-/G2NET) have a better survival compared to a high-grade NET (G3NET) or neuroendocrine carcinoma. At time of diagnosis, metastases are present in approximately 23% of cases, with the liver being the most common site for distant metastases [4]. As the presence of neuroendocrine liver metastases (NELM) negatively affects survival, safe and effective treatments are necessary to prolong survival. As NELM are supplied by arterial blood supply and commonly present with a multifocal distribution, trans-arterial treatments have gained great interest [5, 6]. Particularly radioembolization, a.k.a. selective internal radiation therapy (SIRT), has shown great promise by reported high tumour objective response rates and limited toxicities. This is further amplified by The European Neuroendocrine Tumour Society (ENETS) guideline from 2016 and the European Society for Medical Oncology (ESMO) guideline from 2020 that have extended the role of radioembolization in NELM, including early application as a tumour debulking treatment or as a salvage treatment in selected cases, after failure of systemic treatments [7, 8]. However, there is a clear absence on dosimetry data in almost all the studies on radioembolization in NELM.
Although the importance of dosimetry in radioembolization has already been clearly demonstrated in the landmark studies in other tumour types (e.g., DOSISPHERE-1 in hepatocellular carcinoma), to date only one study examined dosimetry in NELM [9, 10]. Ebbers et al. established a clear dose-survival and dose–response relationship with a minimum tumour absorbed dose (Dt) of 150 Gy in NELM patients treated with yttrium-90 [90Y] glass microspheres. These studies confirmed that with increasing Dt, likelihood of objective response will also increase. However, due to the intrinsic differences of commercially available therapeutic particles, dose thresholds of one particle type, cannot be translated one-to-one to another particle [11]. Although holmium-166 [166Ho] microspheres and [90Y]-microspheres are both used for tumour irradiation, [166Ho]-microspheres have better imaging properties. Through emission of gamma photons and being a lanthanide, visualization of distribution of [166Ho]-microspheres in the liver and quantification of the absorbed tumour dose on SPECT/CT and MRI is possible. Furthermore, by using a low dose of [166Ho]-microspheres in the work-up procedure, the discrepancy between planning and treatment is reduced in comparison to 99mTc-MAA [12].
Therefore, the aim of this study is to examine dose–response relationship and dose-toxicity relationship in NELM treated with [166Ho]-microspheres radioembolization ([166Ho]-radioembolization).
Methods
Patients
All patients from 2012–2022 who underwent [166Ho]-radioembolization (Quiremspheres®, Terumo) for NELM were included in this single center, retrospective study. Inclusion criteria were availability of contrast-enhanced computed tomography (CECT) or magnetic resonance imaging (MRI) of the liver at baseline, presence of at least one measurable target lesion according to the Response Evaluation Criteria In Solid Tumours version 1.1 (RECIST 1.1), and presence of a post-treatment [166Ho]-SPECT/CT for dosimetric purposes. Need for informed consent was waived by the institutional medical ethics committee for this retrospective cohort study.
Treatment procedures
All patients had either progressive disease on imaging or deterioration of clinical status due to increased hormone related complaints (e.g., flushing, diarrhoea) prior to 166Ho-radioembolization and were discussed in a multidisciplinary tumour board.
In preparation of the radioembolization procedure, 1–3 weeks before treatment an hepatic angiography and administration of [166Ho]-scout dose (QuiremScout®, Terumo) or technetium-99 m macroaggregated albumin ([99mTc]-MAA; Pulmocis®, CIS-bio International) was performed in each patient followed by-SPECT/CT. The total amount of administered activity was calculated for the target liver volume, as measured on CECT. Amount of activity prescribed was determined by the treating physicians, which depended on the treatment approach (e.g., whole liver or radiation segmentectomy) and other clinical factors. Administered activity never exceeded the 60 Gy (to the entire liver volume) threshold (i.e., whole liver average absorbed dose), in line with the products instruction for use (IFU). After [166Ho]-radioembolization a post-treatment [166Ho]-SPECT/CT was acquired 3–5 days later [13]. CECT or MRI at three-months follow-up was performed.
166Ho SPECT/CT image acquisition
All [166Ho]-SPECT/CT’s were acquired and reconstructed on a Symbia T16 (Siemens, Erlangen) that uses a medium-energy low-penetration collimator, on a 128 × 128 matrix (pixel spacing, 4.8 × 4.8 mm), with 120 angles (15 s per projection) over a non-circular 360° orbit. An energy window centred at 81 keV (15% width), together with an additional energy window centred at 118 keV (12% width) to correct the [166Ho] photopeak data for down scatter using a window-based scatter correction were used [14]. Low dose non-contrast enhanced CT or CECT images were acquired simultaneously for attenuation correction.
Dosimetry assessment
Manual image segmentation of the post treatment SPECT/CT was performed in Q-suite version 2.1 (Quirem Medical B.V., The Netherlands), creating volumes of interest (VOIs) on baseline CECT or MRI, or simultaneously acquired CECT during the [166Ho]-SPECT/CT. Four distinct compartments were analysed: total liver tissue, target liver tissue (i.e., treatment volume), tumour tissue and total healthy liver tissue (i.e., total liver – tumour). Total counts in the liver in the post-treatment SPECT/CTs were scaled based on the prescribed activity to calculate mean Dt of individual tumours, the mean Dt of all tumours within the treatment volume of the patient (Dt,all), the mean absorbed dose in total healthy liver tissue (Dh). Additionally, pre-treatment total healthy liver volume and percentage (i.e., fraction of total liver), and total tumour volume and percentage were obtained. A minimum tumour diameter of 1 cm was chosen, based on the spatial resolution of [166Ho]-SPECT/CT and being measurable disease according to RECIST 1.1. In case the CT scan that was made consecutively with post-treatment SPECT was non-contrast enhanced, [166Ho]-SPECT was rigidly registered with baseline CECT or MRI.
Response assessment
Baseline and three-months follow-up CECT or MRI were assessed according to RECIST 1.1, for both lesions-based and patient-based analysis. A complete response (CR) was achieved if there was a disappearance of the tumour, a partial response (PR) was achieved when there was a decrease in diameter of at least 30%, a progressive response (PD) was characterized by an increase of at least 20%, and stable disease (SD) was a change within 30% decrease or 20% increase of the tumour. Results were also categorized as responders (CR + PR) and as non-responders (SD + PD). In line with official RECIST 1.1 (general RECIST 1.1), patient-based analysis was based on maximum of two hepatic tumours and non-treated and/or extrahepatic disease.
Toxicity assessment
Relevant clinical and biochemical data at baseline, two weeks, four weeks and at three- months follow-up were retrospectively reviewed according to Common Terminology Criteria for Adverse Events (CTCAE) version 5.0. Laboratory toxicity included albumin, total bilirubin, aspartate aminotransferase (AST), alanine aminotransferase (ALT), gamma-glutamyl transferase (GGT), alkaline phosphatase (APH) and lactate dehydrogenase (LDH). The relative and absolute difference between these laboratory parameters at baseline and after three months of follow-up was also calculated. For clinical toxicity, if symptoms were present at baseline and did not worsen or improve, the toxicity score at follow-up was omitted from the clinical toxicity analysis. If symptoms did worsen, the absolute and highest CTCAE toxicity grade at follow-up was assigned. In cases with a sequential whole liver treatment (first one lobe, several weeks later the other), the highest clinical toxicity grade between sessions or after the second session was used.
Statistical analysis
Descriptive analyses were used for patient characteristics, therapy specifications, and clinical toxicity. Lesion-based dose–response analysis included a maximum of five tumours per included patient, to avoid the data being skewed by patients with extensive disease.
Patient-based dose–response assessment included the mean dose of all tumours within a patient and general RECIST 1.1. Dose–response relationships were modelled using linear mixed-effects regression models, from which ROC curves were constructed, to incorporate any correlation between tumour doses within a patient. Optimal cut-off point (highest specificity and sensitivity) was calculated with an Youden’s J. Subsequently, a desirable dose was determined on box-plot analysis for the highest specificity (i.e. highest likelihood of response).
On a patient level, radiological PFS was defined as the time elapsed between [166Ho]-radioembolization and tumour progression on imaging. OS was assessed as the time between start of the first [166Ho]-radioembolization and death due to any cause. Patients were censored if they were still alive at the time of analysis or were lost to follow-up.
Analysis of the relationship between mean Dt,all and survival was tested in a Kaplan Meier analysis. Furthermore, dichotomized mean Dt,all (cut-off point of 80 and 120 Gy) were tested using log-rank test.
The relationship between CTCAE 5.0 absolute laboratory toxicity grade and total laboratory toxicity score (dependent variables) and total healthy liver percentage and volume and Dh (independent variables) were examined using linear regression models. The relationship between these independent variables, absolute, and percentage change in laboratory values were additionally determined by using linear regression models. Additionally, based on previous published data, the cohort was also dichotomized in Dh < 30 Gy versus ≥ 30 Gy [15]. Toxicity analyses were not adjusted for confounding. IBM SPSS (v26; IBM, Chicago, USA) and R (v4.3.2; R Core Team 2023) was used to conduct the statistical analysis. P-values < 0.05 were considered to be significant.
Results
Study population and treatment characteristics
From 2012 – 2022, a total of 30 patients were treated with [166Ho]-radioembolization, of whom one patient was excluded for all analyses due to absence of follow-up. All of the remaining 29 patients were included for the dose-toxicity analysis and 25 patients were included for the dose–response analysis, as four patients were excluded due to missing post-treatment CECT or MRI three months after [166Ho]-radioembolization (Fig. 1).
One patient had undergone three [166Ho]-radioembolization procedures, with an interval of 5 months between the first and second procedure and 4 years between the second and third procedure. Five patients had undergone two [166Ho]-radioembolization procedures and 23 patients had undergone one [166Ho]-radioembolization procedure (Table 1). A total of 18 treatments (50%) were whole-liver (single session) [166Ho]-radioembolization procedures (Table 2).
Of the included patients, 55% had a small-intestinal NET, 69% a WHO grade 2 NET, previously treated with somatostatin analogues (SSA; 79%) and/or peptide receptor radionuclide therapy (PRRT; 59%). None of the patients were treatment naïve (Table 1).
Dose–response assessment
Lesion-based dose–response analysis included 25 patients with 27 treatments, with a total of 114 tumours. The median tumour size was 2.7 cm (range 1.0 – 12.7 cm).
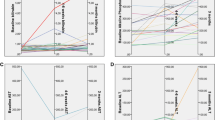
Six tumours had CR, 36 tumours had PR, 69 tumours had SD and three tumours had PD, resulting in an objective response rate (ORR) of 37% and disease control rate (DCR) of 97% of target lesions. The mean Dt in non-responding tumours (PD + SD) was 68 Gy versus 118 Gy in responding tumours (CR + PR) (p = 0.01; Fig. 2). In the ROC analysis, Youden’s-J was 86 Gy to have the highest sensitivity and specificity, resp. 83% and 81%.%. The area under the curve (AUC) was 0.891 (95% CI [0.83; 0.95]). A Dt of 120 Gy had the highest specificity (97%) and provided the highest likelihood of response (90%; Fig. 3).
In the patient-based analysis, 14 patients had PR, 2 patients had SD and 9 patients had PD, resulting in an ORR of 56% and DCR of 64%. Dose–response analysis on patient level did not show a significant difference, with a mean Dt,all of 76 Gy in non-responders (n = 11) versus 81 Gy in responders (n = 14; p = 0.7; Fig. 4).
Dose-toxicity assessment
A total of 29 patients, who underwent a total of 36 treatments, were analysed for the dose-toxicity assessment. Two of the 36 treatments were excluded due to loss of follow-up and non-[166Ho]-radioembolization related choledocholithiasis.
A total of 14 patients (16 treatments) had clinical toxicity and 15 patients (18 treatments) reported no clinical toxicity. Only one grade 3 toxicity was reported, the remaining toxicities included five grade 2 toxicities and 10 grade 1 toxicities. No new grade 4–5 toxicity or carcinoid crisis was encountered. No dose-toxicity relationship was found (p > 0.05).
Laboratory toxicity was reported in 20 patients (24 treatments). Four grade 3, four grade 2 and 16 grade 1 laboratory toxicity was reported (Table 3). No dose-toxicity relationship was found (p > 0.05).
Of the treatments with Dh < 30 Gy one patient (7%) experienced grade 2 clinical toxicity ( nausea, flushing and fatigue; Table 3) and laboratory toxicity was experienced in seven patients (eight treatments, 57% Table 3) with one grade 3 toxicity (increased APH), three grade 2 (GGT and Albumin) and four grade 1 toxicities (AST, GGT, APH and bilirubine).
Of the treatments with Dh ≥ 30 Gy, 70% experienced clinical toxicities (Table 3), with one grade 3 toxicity (liver abscess, which was treated with intravenous antibiotics) and 80% experienced laboratory toxicities (Table 3), of which three grade 3 (increased AST, GGT and APH).
In the linear regression models, no dose-toxicity relationship was found. However, after dichotomizing (Dh < 30 Gy versus ≥ 30 Gy), a significant dose-toxicity relationship in clinical toxicity (p = 0.016; supplemental Table 1) was found. None of the analyses showed a dose-toxicity relationship for laboratory toxicity, even after dichotomization (p = 0.501; supplemental Table 1).
Survival Analysis
Median follow-up time was 14 months (3–82 months) for the 29 patients included. Median overall PFS was 15 months (95% CI [10.2;19.8]). Twelve patients (41%) were censored (seven not reached and five lost-to-follow-up) (Fig. 5).
a Survival curve for PFS in which 12 patients were censored. Median overall PFS was 15 months (95% CI [10.2;19.8]). There was no significant association between Mean Dt,all and PFS. b Survival curve for OS. Mean OS was 50.5 months (95%CI [34.7;66.3]), 18 patients were censored and median OS was not reached. There was no significant association between mean Dt,all and OS
Mean Dt,all was not significantly associated with progression free survival when dichotomizing the patients in < 80 Gy versus ≥ 80 Gy (13 vs. 17 months; p = 0.9) or < 120 Gy versus ≥ 120 Gy (13 vs. 42 months; p > 0.5; supplemental Fig. 1).
Median OS was not reached (Fig. 5). In the OS analyses, dichotomization in < 80 Gy versus ≥ 80 Gy or < 120 Gy versus ≥ 120 Gy, yielded no significant association (p > 0.5; supplemental Fig. 2).
Discussion
This study is the first to investigate a dose–response relationship, and a dose-toxicity relationship in NELM treated with [166Ho]-radioembolization. A clear dose–response relationship was demonstrated with a Dt of ≥ 120 Gy showing a high 90% positive predictive value for an objective response according to RECIST 1.1.
There was no significant difference in Dt,all between responders and non-responders in the patient-based analysis and no linear dose-toxicity relationship was found. However, patients with a Dh < 30 Gy showed significantly less short-term clinical toxicity (p = 0.016).
In this cohort, median PFS was 15 months (95% CI [10.2;19.8]) and median OS was not reached. PFS and OS were found not to be significantly associated with mean Dt,all, however number of patients in this analysis was limited.
Earlier studies demonstrated dose thresholds in patients with other tumour types treated with [166Ho]-radioembolization. Bastiaannet et al. conducted a prospective study in 36 patients with liver metastases of various origins (with only one patient having NELM). They demonstrated a significant difference in tumour-absorbed dose between CR and SD (232 Gy vs 147 Gy; p = 0.01) and between CR and PD (232 Gy vs 117 Gy; p = 0.0008) [16]. A follow-up study by Roekel et al. in 40 patients with colorectal liver metastases (mCRC) also demonstrated a significant dose–response relationship. The authors advocated to personalize the administered treatment dose to achieve a mean Dt,all of > 90 Gy [17]. The present study showed a dose threshold in [166Ho]-radioembolization in NELM, as previously shown by Ebbers et al. for [90Y]-glass radioembolization. In the present cohort study with [166Ho]-radioembolization, a Dt of ≥ 120 Gy resulted in 90% likelihood of objective response. For [90Y]-glass radioembolization, the authors proposed a Dt of > 150 Gy. The difference in dose thresholds can likely be explained by intrinsic differences of the products used, especially differences in specific activity of the used microspheres and differences in physical half-life. This was recently emphasized by the EANM guideline that specifically stated (the need for) different dose thresholds for the different microspheres and for different tumour types [11].
Ebbers et al. suggested a patient-based dose survival relationship using a dose threshold of 150 Gy using [90Y]-glass microspheres, however this was not sustained after correction for confounders [10]. In this study, a patient-based dose survival relationship could not be established. An explanation for lack of significance in the patient based dose–response analysis is due to the multitude of tumours within a patient and the spatial resolution of [166Ho]-SPECT/CT, in which Dt in small tumours(< 1 cm) are not accounted for.
There was no dose-toxicity relationship in our study. Van Roekel et al. advocated a dose threshold with a Dh of < 55 Gy in mCRC. All the patients in the current study had a calculated Dh below this threshold (all < 50 Gy), and no radioembolization- induced liver disease (REILD) was encountered. The suggested threshold by van Roekel et al. cannot be directly translated to NELM due to intrinsic tumour differences, differences in disease course, differences in treatment algorithm etc. A recent study by Stella et al. investigated automatic healthy liver segmentation in 31 patients with NELM who were treated with [166Ho]-radioembolization sequentially after PRRT (i.e., HEPAR PLuS study). They also found no dose-toxicity relationship [15, 18]. In that post-hoc analysis study, all patients had Dh of ≤ 35 Gy and only two cases of significant hepatoxicity were reported, respectively one REILD case with a Dh of 30 Gy and one patient with a CTCAE grade 4 toxicity, with a Dh of 23 Gy. The authors concluded that no conclusions can be drawn on the limited occurrence of hepatotoxicity. Although our study did not find a significant dose-toxicity relationship, significantly less (clinical) toxicity was reported when Dh was < 30 Gy. In line with the presence of dose–response relationships, these results indirectly suggest the presence of a dose-toxicity relationship. Disease course of patients suffering from NELM is significantly different compared to other tumour types (e.g., mCRC), thus one may adhere to this suggested 30 Gy Dh threshold to remain conservatively safe. However, the current study showed no major toxicities with a Dh up to 50 Gy. The current study is underpowered due to lack of significant toxicity.
Correlation to mean dose to the whole non-tumour liver tissue (Dh) was deliberately chosen, as in previous studies on HCC (also hypervascular disease), Dh is more predictive for post-treatment toxicity than mean dose to the non-tumour target volume alone [19, 20]. On the one hand, in first-line setting less toxicity is accepted as other subsequential treatments (e.g. PRRT) are still readily available. On the other hand, patients in salvage setting, having a worse prognosis, more toxicity may be accepted. Nonetheless, future studies on 166Ho-microsphere radioembolization should provide more insights into acceptable Dh threshold.
This cohort study further confirmed the results published on radioembolization in patients with NELM, as reported median PFS and OS in other studies vary between 16 – 25 months and 29 – 35 months, respectively [5]. The median PFS of 15 months in this cohort study fits within that range. Median OS in the current study was not reached. In our survival analysis, mean Dt,all was not significantly associated with PFS or OS. However, a trend can be noted in the analyses dichotomizing for a mean Dt ≥ 120 Gy, giving the highest PFS and OS. This may resemble the previously published study by Ebbers et al. who showed an improved survival in NELM patients treated with [90Y]-glass microspheres, receiving Dt,all ≥ 150 Gy compared to < 150 Gy, 29 versus 12 months (p = 0.018), respectively. However, the current study was underpowered to draw a firm conclusion.
The patient-based ORR at three months of 37% in this cohort study is in line with previous studies (16%-50%) and with the previously published HEPAR PLuS study (43%) [5, 21]. In the NETTER-1 trial on [177Lu]Lu-DOTATATE with long-acting octreotide, ORR at three months was only 18%.The current cohort study demonstrates the effectiveness of [166Ho]-radioembolization as either a debulking or salvage treatment, confirming the current place of radioembolization in both the ENETS and ESMO guidelines [7, 8]. The application of Dt > 120 Gy threshold with prospective dosimetry in future studies will probably show further improvement of outcomes.
This study had several limitations. Besides being a retrospective study and relatively small population, the chosen follow-up period for radiological response assessment of three months was relatively short. Especially considering that studies have shown that up to 25% of response assessments can change at six months [22]. In line with other studies on radioembolization, the included patients were heterogeneous (different tumour grade, different tumour origins, etc.), had different lines of previous treatments and none were treatment naïve, therefore creating bias. Follow-up duration in this cohort study was relatively short, limiting the number of events in our survival analyses (in particular OS). Due to the limited number of patients, the survival analyses were not corrected for known clinical factors (e.g. tumour grading, etc.). Number of reported and encountered adverse events was limited, illustrating that radioembolization is a safe and effective treatment, but probably also suffers from a reporting bias in a retrospective setting. Long-term toxicity, and especially long term hepatotoxicity was not investigated in this current study. Concerns have been raised in the past, mainly in North America, after cirrhosis-like morphology (without clinical complaints) was reported on imaging studies in patients treated with radioembolization.
However in a prospective study and larger retrospective studies these concerns could not be affirmed. Furthermore, a recent single center study, demonstrated no significant difference (22% vs. 29%, respectively) in long-term hepatotoxicity between patients treated with TACE and radioembolization [5].
This is the first study to demonstrate a dose–response relationship with [166Ho]-radioembolization. Prospective studies are necessary to further evaluate [166Ho]-radioembolization in treatment of NELM. These must incorporate prospective dosimetry and individualized treatment planning. Besides dosimetry, future studies should include longer follow-up than in radioembolization studies in other tumour types.
As inclusion of prospective dosimetry in multicenter studies is challenging, the suggested [166Ho]–[99mTc] dual-isotope SPECT/CT by Stella et al. may ease translation and broad implementation [15]. They concluded that automatic segmentation of the healthy liver tissue could optimize [166Ho]-radioembolization, as the total healthy liver dose is dose-limiting, thus accurate assessment of Dh is essential to mitigate possible hepatotoxicity in NELM.
Conclusion
This study confirms the safety and efficacy of [166Ho]-radioembolization in NELM in a real-world setting, with a clear dose–response relationship. Future prospective studies should include prospective dosimetry and aim for a tumour absorbed dose of at least 120 Gy. No dose-toxicity relationship could be demonstrated.
Data Availability
The data that support the findings of this study are available upon reasonably request via contacting the corresponding author.
References
Oronsky B, Ma PC, Morgensztern D, Carter CA. Nothing But NET: A Review of Neuroendocrine Tumors and Carcinomas. Neoplasia. 2017;19:991–1002.
Basu B, Sirohi B, Corrie P. Systemic therapy for neuroendocrine tumours of gastroenteropancreatic origin. Endocr Relat Cancer. 2010;17:R75-90. https://doi.org/10.1677/erc-09-0108.
Rindi G, Mete O, Uccella S, Basturk O, La Rosa S, Brosens LAA, et al. Overview of the 2022 WHO Classification of Neuroendocrine Neoplasms. Endocr Pathol. 2022;33:115–54. https://doi.org/10.1007/s12022-022-09708-2.
Riihimäki M, Hemminki A, Sundquist K, Sundquist J, Hemminki K. The epidemiology of metastases in neuroendocrine tumors. Int J Cancer. 2016;139:2679–86. https://doi.org/10.1002/ijc.30400.
Ramdhani K, Braat A. The Evolving Role of Radioembolization in the Treatment of Neuroendocrine Liver Metastases. Cancers (Basel). 2022;14. https://doi.org/10.3390/cancers14143415.
Cives M, Pelle E, Quaresmini D, Rizzo FM, Tucci M, Silvestris F. The Tumor Microenvironment in Neuroendocrine Tumors: Biology and Therapeutic Implications. Neuroendocrinology. 2019;109:83–99. https://doi.org/10.1159/000497355.
Pavel M, O’Toole D, Costa F, Capdevila J, Gross D, Kianmanesh R, et al. ENETS Consensus Guidelines Update for the Management of Distant Metastatic Disease of Intestinal, Pancreatic, Bronchial Neuroendocrine Neoplasms (NEN) and NEN of Unknown Primary Site. Neuroendocrinology. 2016;103:172–85. https://doi.org/10.1159/000443167.
Pavel M, Öberg K, Falconi M, Krenning EP, Sundin A, Perren A, Berruti A. Gastroenteropancreatic neuroendocrine neoplasms: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:844–60. https://doi.org/10.1016/j.annonc.2020.03.304.
Garin E, Tselikas L, Guiu B, Chalaye J, Edeline J, de Baere T, et al. Personalised versus standard dosimetry approach of selective internal radiation therapy in patients with locally advanced hepatocellular carcinoma (DOSISPHERE-01): a randomised, multicentre, open-label phase 2 trial. Lancet Gastroenterol Hepatol. 2021;6:17–29. https://doi.org/10.1016/s2468-1253(20)30290-9.
Ebbers SC, van Roekel C, Braat M, Barentsz MW, Lam M, Braat A. Dose-response relationship after yttrium-90-radioembolization with glass microspheres in patients with neuroendocrine tumor liver metastases. Eur J Nucl Med Mol Imaging. 2022;49:1700–10. https://doi.org/10.1007/s00259-021-05642-3.
Weber M, Lam M, Chiesa C, Konijnenberg M, Cremonesi M, Flamen P, et al. EANM procedure guideline for the treatment of liver cancer and liver metastases with intra-arterial radioactive compounds. Eur J Nucl Med Mol Imaging. 2022;49:1682–99. https://doi.org/10.1007/s00259-021-05600-z.
Smits MLJ, Dassen MG, Prince JF, Braat A, Beijst C, Bruijnen RCG, et al. The superior predictive value of (166)Ho-scout compared with (99m)Tc-macroaggregated albumin prior to (166)Ho-microspheres radioembolization in patients with liver metastases. Eur J Nucl Med Mol Imaging. 2020;47:798–806. https://doi.org/10.1007/s00259-019-04460-y.
Stella M, Braat A, Lam M, de Jong H, van Rooij R. Gamma camera characterization at high holmium-166 activity in liver radioembolization. EJNMMI Phys. 2021;8:22. https://doi.org/10.1186/s40658-021-00372-9.
Stella M, Braat A, van Rooij R, de Jong H, Lam M. Holmium-166 Radioembolization: Current Status and Future Prospective. Cardiovasc Intervent Radiol. 2022;45:1634–45.
Stella M, van Rooij R, Lam M, de Jong H, Braat A. Automatic healthy liver segmentation for holmium-166 radioembolization dosimetry. EJNMMI Res. 2023;13:68.
Bastiaannet R, van Roekel C, Smits MLJ, Elias SG, van Amsterdam WAC, Doan D, et al. First Evidence for a Dose-Response Relationship in Patients Treated with (166)Ho Radioembolization: A Prospective Study. J Nucl Med. 2020;61:608–12. https://doi.org/10.2967/jnumed.119.232751.
van Roekel C, Bastiaannet R, Smits MLJ, Bruijnen RC, Braat A, de Jong H, et al. Dose-Effect Relationships of (166)Ho Radioembolization in Colorectal Cancer. J Nucl Med. 2021;62:272–9. https://doi.org/10.2967/jnumed.120.243832.
Braat A, Bruijnen RCG, van Rooij R, Braat M, Wessels FJ, van Leeuwaarde RS, et al. Additional holmium-166 radioembolisation after lutetium-177-dotatate in patients with neuroendocrine tumour liver metastases (HEPAR PLuS): a single-centre, single-arm, open-label, phase 2 study. Lancet Oncol. 2020;21:561–70. https://doi.org/10.1016/s1470-2045(20)30027-9.
Chiesa C, Mira M, Bhoori S, Bormolini G, Maccauro M, Spreafico C, et al. Radioembolization of hepatocarcinoma with (90)Y glass microspheres: treatment optimization using the dose-toxicity relationship. Eur J Nucl Med Mol Imaging. 2020;47:3018–32. https://doi.org/10.1007/s00259-020-04845-4.
Chiesa C, Mira M, Maccauro M, Spreafico C, Romito R, Morosi C, et al. Radioembolization of hepatocarcinoma with (90)Y glass microspheres: development of an individualized treatment planning strategy based on dosimetry and radiobiology. Eur J Nucl Med Mol Imaging. 2015;42:1718–38. https://doi.org/10.1007/s00259-015-3068-8.
Braat A, Kwekkeboom DJ, Kam BLR, Teunissen JJM, de Herder WW, Dreijerink KMA, et al. Additional hepatic (166)Ho-radioembolization in patients with neuroendocrine tumours treated with (177)Lu-DOTATATE; a single center, interventional, non-randomized, non-comparative, open label, phase II study (HEPAR PLUS trial). BMC Gastroenterol. 2018;18:84.
Braat A, Kappadath SC, Ahmadzadehfar H, Stothers CL, Frilling A, Deroose CM, et al. Radioembolization with (90)Y Resin Microspheres of Neuroendocrine Liver Metastases: International Multicenter Study on Efficacy and Toxicity. Cardiovasc Intervent Radiol. 2019;42:413–25. https://doi.org/10.1007/s00270-018-2148-0.
Funding
No funding was received for this work.
Author information
Authors and Affiliations
Contributions
KR, JBV and AJATB collected the data. KR and AJATB analyzed the data, KR and AJATB wrote the manuscript draft with input from all authors. All authors read, critically reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
KR, JBV, SCE and RCGB have nothing to disclose, MLJS has acted as consultant for Terumo, and has received speaking fees for Medtronic and Philips, RR and HWAMdJ have acted as consultants for Boston Scientific. MGEHL has acted as a consultant for Boston Scientific and Terumo, and receives research support from Novartis, Boston Scientific and Terumo, AJATB has acted as consultant for Boston Scientific, GE Healthcare and Terumo, and receives research support from Ariceum Therapeutics. The UMC Utrecht receives research support and royalties from Terumo and Quiremspheres.
Ethics approval and consent to participate
Need for informed consent was waived by the institutional medical ethics committee for this retrospective cohort study.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ramdhani, K., Beijer-Verduin, J., Ebbers, S.C. et al. Dose–effect relationships in neuroendocrine tumour liver metastases treated with [166Ho]-radioembolization. Eur J Nucl Med Mol Imaging 51, 2114–2123 (2024). https://doi.org/10.1007/s00259-024-06645-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-024-06645-6