Abstract
Purpose
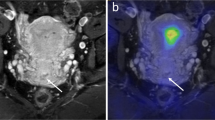
To evaluate the contributory value of positron emission tomography (PET)-intravoxel incoherent motion (IVIM) magnetic resonance imaging (MRI) in the prediction of lymphovascular space invasion (LVSI) in patients with cervical cancer without lymphatic metastasis.
Materials and methods
A total of 90 patients with cervical cancer without signs of lymph node metastasis on PET/MRI were enrolled in this study. The tumours were classified into LVSI-positive (n = 25) and LVSI-negative (n = 65) groups according to postoperative pathology. The PET-derived parameters (SUVmax, SUVmean, metabolic tumour volume (MTV) and total lesion glycolysis (TLG)) and IVIM-derived parameters (ADCmean, ADCmin, Dmean, Dmin, f, D* and gross tumour volume (GTV)) between the two groups were evaluated using a Student’s t test (Mann-Whitney U test for variables with a nonnormal distribution) and receiver operating characteristic (ROC) curves. The optimal combination of PET/MR parameters for predicting LVSI was investigated using univariate and multivariate logistic regression models and evaluated by ROC curves. The optimal cutoff threshold values corresponded to the maximal values of the Youden index. A control model was established using 1000 bootstrapped samples, for which the performance was validated using calibration curves and ROC curves.
Results
PET-derived parameters (SUVmax, SUVmean, MTV, TLG) and IVIM MRI-derived parameters (Dmin, ADCmin, GTV) were significantly different between patients with and without LVSI (P < 0.05). Logistic analyses showed that a combination of TLG and Dmin had the strongest predictive value for LVSI diagnosis (area under the curve (AUC), 0.861; sensitivity, 80.00; specificity, 86.15; P < 0.001). The optimal cutoff threshold values for Dmin and TLG were 0.58 × 10−3 mm2/s and 66.68 g/cm3, respectively. The verification model showed the combination of TLG and Dmin had the strongest predictive value, and its ROC curve and calibration curve showed good accuracy (AUC, 0.878) and consistency.
Conclusions
The combination of TLG and Dmin may be the best indicator for predicting LVSI in cervical cancer without lymphatic metastasis.





Similar content being viewed by others
Data availability
The datasets used and analysed of the current study are available from the corresponding author on reasonable request.
References
Small W Jr, Bacon MA, Bajaj A, Chuang LT, Fisher BJ, Harkenrider MM, et al. Cervical cancer: a global health crisis. Cancer. 2017;123(13):2404–12. https://doi.org/10.1097/01.ogx.0000526010.06041.5e.
Schmeler KM, Frumovitz M, Ramirez PT. Conservative management of early stage cervical cancer: is there a role for less radical surgery? Gynecol Oncol. 2011;120(3):321–5. https://doi.org/10.1016/j.ygyno.2010.12.352.
Hanprasertpong J, Jiamset I. Late recurrence of early stage cervical cancer more than 3 years after radical hysterectomy with pelvic node dissection. Oncol Res Treat. 2017;40(5):270–6. https://doi.org/10.1159/000464408.
Pol FJM, Zusterzeel PLM, van Ham MAPC, Kuijpers DAT, Bulten J, Massuger LFAG. Satellite lymphovascular space invasion: an independent risk factor in early stage cervical cancer. Gynecol Oncol. 2015;138(3):579–84. https://doi.org/10.1016/j.ygyno.2015.06.035.
Boyraz G, Basaran D, Salman MC, Ozgul N, Yuce K. Clinical and pathological characteristics related to parametrial involvement in clinical early-stage cervical cancer. Ginekol Pol. 2016;87(6):417–21. https://doi.org/10.5603/GP.2016.0018.
Yu Q, Lou XM, He Y. Prediction of local recurrence in cervical cancer by a Cox model comprised of lymph node status, lymph-vascular space invasion and intratumoralTh17 cell-infiltration. Med Oncol. 2014;31(1):795. https://doi.org/10.1007/s12032-013-0795-1.
Ahlin PA, Weiss RI. Risk management and compliance in pathology and laboratory medicine. Clin Lab Med. 2017;27(4):859–73. https://doi.org/10.1016/j.cll.2007.07.005.
Lee SI, Atri M. 2018 FIGO staging system for uterine cervical cancer: enter cross-sectional imaging. Radiology. 2019;292(1):15–24. https://doi.org/10.1148/radiol.2019190088.
Marchiole P, Buenerd A, Benchaib M, Nezhat K, Dargent D, Mathevet P. Clinical significance of lympho vascular space involvement and lymph node micrometastases in early-stage cervical cancer: a retrospective case-control surgico-pathological study. Gynecol Oncol. 2005;97(3):727–32. https://doi.org/10.1016/j.ygyno.2005.01.004.
Ramirez PT, Milam MR. Laparoscopic extraperitoneal paraaortic lymphadenectomy in patients with locally advanced cervical cancer. Gynecol Oncol. 2007;104(2):9–12. https://doi.org/10.1016/j.ygyno.2006.10.032.
Kidd EA, Thomas M, Siegel BA, Dehdashti F, Grigsby PW. Changes in cervical cancer FDG uptake during chemoradiation and association with response. Int J Radiat Oncol Biol Phys. 2013;85(1):116–22. https://doi.org/10.1016/j.ijrobp.2012.02.056.
Akkas BE, Demirel BB, Dizman A, Vural GU. Do clinical characteristics and metabolic markers detected on positron emission tomography/computerized tomography associate with persistent disease in patients with in-operable cervical cancer? Ann Nucl Med. 2013;27(8):756–63. https://doi.org/10.1007/s12149-013-0745-1.
Le Bihan D, Breton E, Lallemand D, Aubin ML, Vignaud J, Laval-Jeantet M. Separation of diffusion and perfusion in intravoxel incoherent motion MRI imaging. Radiology. 1988;168(2):497–505. https://doi.org/10.1148/radiology.168.2.3393671.
Beiderwellen K, Grueneisen J, Ruhlmann V, Buderath P, Aktas B, Heusch P, et al. [18F] FDG PET/MRI vs. PET/CT for whole-body staging in patients with recurrent malignancies of the female pelvis: initial results. Eur J Nucl Med Mol Imaging. 2015;42(1):56–65. https://doi.org/10.1007/s00259-014-2902-8.
Xu C, Du S, Zhang S, Wang B, Dong C, Sun H. Value of integrated PET-IVIM MR in assessing metastases in hypermetabolic pelvic lymph nodes in cervical cancer: a multi-parameter study. Eur Radiol. 2020;30(5):2483–92. https://doi.org/10.1007/s00330-019-06611-z.
Noda Y, Goshima S, Kanematsu M, Watanabe H, Kawada H, Kawai N, et al. F-18 FDG uptake on positron emission tomography as a predictor for lymphovascular invasion in patients with lung adenocarcinoma. Ann Nucl Med. 2016;30(1):11–7. https://doi.org/10.1007/s12149-015-1023-1.
Yang W, Qiang JW, Tian HP, Chen B, Wang AJ, Zhao JG. Minimum apparent diffusion coefficient for predicting lymphovascular invasion in invasive cervical cancer. J Magn Reson Imaging. 2017;45(6):1771–9. https://doi.org/10.1002/jmri.25542.
Igarashi T. furube H, Ashida H, Ojiri H. Breast MRI for prediction of lymphovascular invasion in breast cancer patients with clinically negative axillary lymph nodes. Eur J Radiol. 2018;107:111–8. https://doi.org/10.1016/j.ejrad.2018.08.024.
Xu C, Sun H, Du S, Xin J. Early treatment response of patients undergoing concurrent chemoradiotherapy for cervical cancer: an evaluation of integrated multi-parameter PET-IVIM MR. Eur J Radiol. 2019;117:1–8. https://doi.org/10.1016/j.ejrad.2019.05.012.
Morsing A, Hildebrandt MG, Vilstrup MH, Wallenius SE, Gerke O, Petersen H, et al. Hybrid PET/MRI in major cancers: a scoping review. Eur J Nucl Med Mol Imaging. 2019;46(10):2138–51. https://doi.org/10.1007/s00259-019-04402-8.
Sarabhai T, Schaarschmidt BM, Wetter A, Kirchner J, Aktas B, Forsting M, et al. Comparison of 18 F-FDG PET/MRI and MRI for pre-therapeutic tumor staging of patients with primary cancer of the uterine cervix. Eur J Nucl Med Mol Imaging. 2018;45(1):67–76. https://doi.org/10.1007/s00259-017-3809-y.
Wang T, Sun HZ, Han FF, Sun WZ, Chen ZW. Evaluation of parametrial infiltration in cervical cancer with voxel-based segmentation of integrated F-FDG PET/MRI images: a preliminary study. Eur J Radiol. 2019;118:147–52. https://doi.org/10.1016/j.ejrad.2019.07.020.
Boellaard R, Krak NC, Hoekstra OS, Lammertsma AA. Effects of noise, image resolution, and ROI definition on the accuracy of standard uptake values: a simulation study. J Nucl Med. 2004;45(9):1519–27. https://doi.org/10.1016/j.nuclcard.2004.07.002.
Chen XL, Chen GW, Xu GH, Ren J, Li ZL, Pu H, et al. Tumor size at magnetic resonance imaging association with lymph node metastasis and lymphovascular space invasion in resectable cervical cancer a multicenter evaluation of surgical specimens. Int J Gynecol Cancer. 2018;28(8):1545–52. https://doi.org/10.1097/IGC.0000000000001327.
Kim CK, Park BK, Kim B. Diffusion-weighted MRI at 3T for the evaluation of prostate cancer. AJR Am J Roentgenol. 2010;194(6):1461–9. https://doi.org/10.2214/AJR.09.3654.
Winfield JM, Orton MR, Collins DJ, Ind TEJ, Attygalle A, Hazell S, et al. Separation of type and grade in cervical tumours using non-mono-exponential models of diffusion-weighted MRI. Eur Radiol. 2017;27:627–36. https://doi.org/10.1007/s00330-016-4417-0.
Li X, Wang P, Li D, Zhu H, Meng L, Song Y, et al. Intravoxel incoherent motion MR imaging of early cervical carcinoma: correlation between imaging parameters and tumor-stroma ratio. Eur Radiol. 2018;28(5):1875–83. https://doi.org/10.1007/s00330-017-5183-3.
Wu Q, Zheng D, Shi L, Liu M, Wang M, Shi D. Differentiating metastatic from nonmetastatic lymph nodes in cervical cancer patients using monoexponential, biexponential, and stretched exponential diffusion-weighted MR imaging. Eur Radiol. 2017;27:5272–9. https://doi.org/10.1007/s00330-017-4873-1.
Morice P, Piovesan P, Rey A, Atallah D, Haie Meder C, Pautier P, et al. Prognostic value of lymphovascular space invasion determined with hematoxylin eosin staining in early stage cervical carcinoma: results of a multivariate analysis. Ann Oncol. 2003;14(10):1511–7. https://doi.org/10.1093/annonc/mdg412.
Silva-filho AL, Traiman P, Triginelli SA, Reis FM, Pedrosa MS, Miranda D, et al. Association between CD31 expression and histopathologic features in stage IB squamous cell carcinoma of the cervix. J Gynecol Cancer. 2006;16(2):757–62. https://doi.org/10.1111/j.1525-1438.2006.00362.x.
Lee EY, Yu X, Chu MM, Ngan HY, Siu SW, Soong IS, et al. Perfusion and diffusion characteristics of cervical cancer based on intraxovel incoherent motion MR imaging-a pilot study. Eur Radiol. 2014;24(7):1506–13. https://doi.org/10.1007/s00330-014-3160-7.
Zhang L, Sun H, Du S, Xu W, Xin J, Guo Q. Evaluation of 18F-FDG PET/CT parameters for reflection of aggressiveness and prediction of prognosis in early-stage cervical cancer. Nucl Med Commun. 2018;39(11):1045–52. https://doi.org/10.1097/MNM.0000000000000909.
Acknowledgements
We would like to thank the native English-speaking scientists of BioMed Proofreading Company and Springer Nature Proofreading Company for editing our manuscript.
Funding
This study was funded by the LIAONING Science & Technology Project (2017225012), LIAONING Science Natural Science Foundation (2019-MS-373) and 345 Talent Project.
Author information
Authors and Affiliations
Contributions
Conceptualisation: Chen Xu, Hongzan Sun; methodology: Chen Xu, Xiaoran Li; formal analysis: Chen Xu; investigation: Yang Yu; resources: Chen Xu, Hongzan Sun; data curation: Chen Xu; writing-original draft preparation: Chen Xu; writing - review and editing: Chen Xu; supervision: Hongzan Sun; project administration: Hongzan Sun; and funding acquisition: Hongzan Sun. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The present study was approved by the Shengjing Hospital of China Medical University Technology ethics committees.
Consent for publication
The publication of this paper is approved by all authors and tacitly or explicitly by the responsible authorities where the work was carried out.
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Oncology – Genitourinary
Rights and permissions
About this article
Cite this article
Xu, C., Yu, Y., Li, X. et al. Value of integrated PET-IVIM MRI in predicting lymphovascular space invasion in cervical cancer without lymphatic metastasis. Eur J Nucl Med Mol Imaging 48, 2990–3000 (2021). https://doi.org/10.1007/s00259-021-05208-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-021-05208-3