Abstract
Objectives
To determine the diagnostic value of monoexponential, biexponential and stretched exponential models for identifying lymph nodes (LNs) in patients with cervical cancer.
Materials and methods
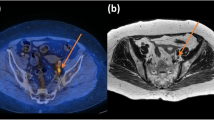
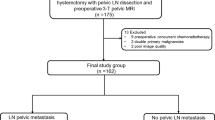
Fifty female patients with cervical cancer underwent preoperative magnetic resonance imaging. The diffusion parameters of the LNs were calculated by fitting the values to monoexponential, biexponential and stretched exponential models and were compared between the metastatic and non-metastatic LN groups.
Results
A total of 157 LNs with high signal intensity on multi-b-value DWI were detected, 41 of which were pathologically shown to be metastatic. Metastatic LNs presented with higher pure water diffusion (D) values, lower perfusion fraction (f) values, higher diffusion heterogeneity (α) values, higher short diameter (Size-S), long diameter (Size-L) and short long diameter ratio (S/L Ratio) than non-metastatic LNs (P<0.05). The Size-S of LNs exhibited the highest diagnostic value, with an area under the curve of 0.844.
Conclusions
Compared with the size parameters, the diffusion parameters derived from multi-b-value diffusion-weighted imaging cannot reliably discriminate metastatic from non-metastatic LNs in daily clinical routine due to limited sensitivity and specificity.
Key Points
• Biexponential and stretched exponential diffusion models can help to characterise LN status.
• Metastatic LNs present with higher D and α values, lower f values.
• Diffusion parameters were less reliable in discriminating LNs than size parameters.



Similar content being viewed by others
Abbreviations
- α:
-
Intravoxel water diffusion heterogeneity
- ADC:
-
Apparent diffusion coefficients
- AUC:
-
Area under the curve
- CCRT:
-
Concurrent chemoradiotherapy
- D:
-
Pure water diffusion
- D*:
-
Pseudodiffusion
- DDC:
-
Distributed diffusion coefficient
- DWI:
-
Diffusion-weighted imaging
- f:
-
Perfusion fraction
- FIGO:
-
International Federation of Gynaecology and Obstetrics
- G1/2:
-
Well and moderately differentiated tumours
- G3:
-
Poorly differentiated tumours
- IVIM:
-
Intravoxel incoherent motion
- LN:
-
Lymph node
- MRI:
-
Magnetic resonance imaging
- NEX:
-
Number of excitation
- ROI:
-
Region of interest
- S/L:
-
Ratio Short-long diameter ratio
- Size-L:
-
Long diameter
- Size-S:
-
Short diameter
- TR/TE:
-
Repetition time/echo time
References
Follen M, Levenback CF, Iyer RB et al (2003) Imaging in cervical cancer. Cancer 98:2028–2038
Shen G, Zhou H, Jia Z, Deng H (2015) Diagnostic performance of diffusion-weighted MRI for detection of pelvic metastatic lymph nodes in patients with cervical cancer: a systematic review and meta-analysis. Br J Radiol 88:20150063
Thoeny HC, Froehlich JM, Triantafyllou M et al (2014) Metastases in normal-sized pelvic lymph nodes: detection with diffusion-weighted MR imaging. Radiology 273:125–135
Vandecaveye V, De Keyzer F, Vander Poorten V et al (2009) Head and neck squamous cell carcinoma: value of diffusion-weighted MR imaging for nodal staging. Radiology 251:134–146
Marti-Bonmati L (2011) Lymph node assessment by diffusion weighted imaging in cervical cancer. Eur Radiol 21:474–477
Lin G, Ho KC, Wang JJ et al (2008) Detection of lymph node metastasis in cervical and uterine cancers by diffusion-weighted magnetic resonance imaging at 3T. J Magn Reson Imaging 28:128–135
Kim JK, Kim KA, Park BW, Kim N, Cho KS (2008) Feasibility of diffusion-weighted imaging in the differentiation of metastatic from nonmetastatic lymph nodes: early experience. J Magn Reson Imaging 28:714–719
Wendl CM, Müller S, Eiglsperger J, Fellner C, Jung EM, Meier JK (2016) Diffusion-weighted imaging in oral squamous cell carcinoma using 3 Tesla MRI: is there a chance for preoperative discrimination between benign and malignant lymph nodes in daily clinical routine? Acta Radiol 57:939–946
Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407
Bennett KM, Schmainda KM, Bennett RT, Rowe DB, Lu H, Hyde JS (2003) Characterization of continuously distributed cortical water diffusion rates with a stretched-exponential model. Magn Reson Med 50:727–734
Qiu L, Liu XL, Liu SR et al (2016) Role of quantitative intravoxel incoherent motion parameters in the preoperative diagnosis of nodal metastasis in patients with rectal carcinoma. J Magn Reson Imaging 44:1031–1039
Yu XP, Wen L, Hou J et al (2016) Discrimination between metastatic and nonmetastatic mesorectal lymph nodes in rectal cancer using intravoxel incoherent motion diffusion-weighted magnetic resonance imaging. Acad Radiol 23:479–485
Pano B, Sebastia C, Ripoll E et al (2015) Pathways of lymphatic spread in gynecologic malignancies. Radiographics 35:916–945
Lengele B, Scalliet P (2009) Anatomical bases for the radiological delineation of lymph node areas. Part III: Pelvis and lower limbs. Radiother Oncol 92:22–33
Kasuya G, Toita T, Furutani K et al (2013) Distribution patterns of metastatic pelvic lymph nodes assessed by CT/MRI in patients with uterine cervical cancer. Radiat Oncol 8:139
Holman LL, Levenback CF, Frumovitz M (2014) Sentinel lymph node evaluation in women with cervical cancer. J Minim Invasive Gynecol 21:540–545
Michel G, Morice P, Castaigne D, Leblanc M, Rey A, Duvillard P (1998) Lymphatic spread in stage Ib and II cervical carcinoma: anatomy and surgical implications. Obstet Gynecol 91:360–363
Klerkx WM, Veldhuis WB, Spijkerboer AM et al (2012) The value of 3.0Tesla diffusion-weighted MRI for pelvic nodal staging in patients with early stage cervical cancer. Eur J Cancer 48:3414–3421
Heijnen LA, Lambregts DM, Mondal D et al (2013) Diffusion-weighted MR imaging in primary rectal cancer staging demonstrates but does not characterise lymph nodes. Eur Radiol 23:3354–3360
Marconi DG, Fregnani JHTG, Rossini RR et al (2016) Pre-treatment MRI minimum apparent diffusion coefficient value is a potential prognostic imaging biomarker in cervical cancer patients treated with definitive chemoradiation. BMC Cancer 16:556
Hompland T, Ellingsen C, Galappathi K, Rofstad EK (2014) Connective tissue of cervical carcinoma xenografts: associations with tumor hypoxia and interstitial fluid pressure and its assessment by DCE-MRI and DW-MRI. Acta Oncol 53:6–15
Lee EYP, Yu X, Chu MMY et al (2014) Perfusion and diffusion characteristics of cervical cancer based on intraxovel incoherent motion MR imaging-a pilot study. Eur Radiol 24:1506–1513
Winfield JM, Orton MR, Collins DJ et al (2016) Separation of type and grade in cervical tumours using non-mono-exponential models of diffusion-weighted MRI. Eur Radiol 27:627–636
Bai Y, Lin Y, Tian J et al (2016) Grading of Gliomas by Using Monoexponential, Biexponential, and Stretched Exponential Diffusion-weighted MR Imaging and Diffusion Kurtosis MR Imaging. Radiology 278:496–504
Lai V, Lee VH, Lam KO, Sze HC, Chan Q, Khong PL (2015) Intravoxel water diffusion heterogeneity MR imaging of nasopharyngeal carcinoma using stretched exponential diffusion model. Eur Radiol 25:1708–1713
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dapeng Shi.
Conflict of interest
The authors of this manuscript declare relationships with the following companies:
The author Dandan Zheng is an employee of GE Healthcare.
Funding
This study has received funding by the Chinese National Natural Science Foundation (Grant number 81271534).
Statistics and biometry
No complex statistical methods were necessary for this paper.
Ethical approval
Institutional Review Board approval was obtained.
Informed consent
Written informed consent was obtained from all patients in this study.
Methodology
• Prospective
• Diagnostic or prognostic study
• Performed at one institution
Rights and permissions
About this article
Cite this article
Wu, Q., Zheng, D., Shi, L. et al. Differentiating metastatic from nonmetastatic lymph nodes in cervical cancer patients using monoexponential, biexponential, and stretched exponential diffusion-weighted MR imaging. Eur Radiol 27, 5272–5279 (2017). https://doi.org/10.1007/s00330-017-4873-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4873-1