Abstract
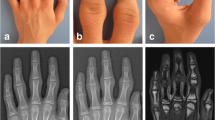
Pachydermodactyly is a rare and benign superficial fibromatosis characterized by painless and progressive swelling of periarticular soft tissues of the proximal interphalangeal (PIP) joints, most commonly of both hands. There is no tenderness, warmth, morning stiffness, or reduced range of motion associated. Our purpose is to highlight the diagnostic utility of ultrasonography, superb microvascular imaging (SMI), and elastography in pachydermodactyly. We report the case of a 15-year-old adolescent white boy, with a 6-month history of insidious and progressive, asymptomatic swelling of the lateral and dorsal regions of the metacarpophalangeal (MCP), and PIP joints of both hands. Articular ultrasonography showed thickening of the skin around the lateral regions of the PIP and MCP joints, with no synovitis, hydrarthrosis, or muscle, tendon, or bone changes. Strain elastography revealed lower elasticity in the aforementioned skin regions, corresponding to increased tissue hardness due to hyperkeratosis. No SMI or Doppler signals were detected in epidermal or dermal tissues, as well as in tendons, joints, and bone. This case report shows that ultrasonography, SMI, and elastography may play a significant role in the accurate diagnosis of pachydermodactyly and exclusion of alternative conditions. These imaging modalities have no ionizing radiation; they are fast, inexpensive, and performed on site. They do not require usage of contrast agents and thus can eliminate the need of invasive procedures such as skin biopsy. They also contribute to reduce health care costs with unnecessary complementary tests and inappropriate treatment.



Similar content being viewed by others
References
Dias JM, Costa MM, Romeu JC, Soares-Almeida L, Filipe P, Pereira da Silva JA. Pachydermodactyly in a 16-year-old adolescent boy. J Clin Rheumatol. 2012;18(5):246–8.
Vázquez Fernández R, Maneiro Fernández JR, Cervantes Pérez EC, Mera Varela A. Pachydermodactyly: a systematic review. Ir J Med Sci. 2021;190(3):1005–14.
Zabotti A, Errichetti E, Cereser L, et al. Pachydermodactyly: the role of ultrasonography and dermoscopy for diagnosis. Rheumatology. 2017;56(5):703.
Alis D, Erol BC, Akbas S, Barut K, Kasapcopur O, Adaletli I. Superb microvascular imaging compared with power Doppler ultrasound in assessing synovitis of the knee in juvenile idiopathic arthritis: a preliminary study. J Ultrasound Med. 2020;39(1):99–106.
Lin M, Wang C. Superb microvascular imaging evaluating joint lesion scores in rheumatoid arthritis compared with power Doppler imaging: a meta-analysis. Medicine. 2020;99(37):e22185.
Fujioka K, Fujioka A, Okada M. High-resolution ultrasonographic appearances in superficial fibromatoses: palmar and plantar diseases. Biomed J Sci Tech Res. 2020;27(2):20548–54.
Chamberlain AJ, Venning VA, Wojnarowska F. Pachydermodactyly: a forme fruste of knuckle pads? Australas J Dermatol. 2003;44(2):140–3.
Sandobal C, Kuznietz A, Varizat A, Roverano S, Paira S. Pachydermodactyly: four additional cases. Clin Rheumatol. 2007;26(6):962–4.
Filippucci E, Cipolletta E, Mirza RM, et al. Ultrasound imaging in rheumatoid arthritis. Radiol Med. 2019;124(11):1087–100.
Dubash SR, De Marco G, Wakefield RJ, Tan AL, McGonagle D, Marzo-Ortega H. Ultrasound imaging in psoriatic arthritis: what have we learnt in the last five years? Front Med. 2020;7:487.
Dias JACM, Rosa RS, Perpétuo I, et al. Pachydermoperiostosis in an African patient caused by a Chinese/Japanese SLCO2A1 mutation-case report and review of literature. Semin Arthritis Rheum. 2014;43(4):566–9.
Christiansen SN, Østergaard M, Terslev L. Ultrasonography in gout: utility in diagnosis and monitoring. Clin Exp Rheumatol. 2018;36 Suppl 114(5):61–7.
Campbell EA, Wilbert CD. Foreign body imaging. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
Lopez-Ben R, Dehghanpisheh K, Chatham WW, Lee DH, Oakes J, Alarcón GS. Ultrasound appearance of knuckle pads. Skeletal Radiol. 2006;35(11):823–7.
Pacheco-Tena C, Londoño JD, Cazarín-Barrientos J, et al. Development of a radiographic index to assess the tarsal involvement in patients with spondyloarthropathies. Ann Rheum Dis. 2002;61(4):330–4.
Snoj Ž, Wu CH, Taljanovic MS, Dumić-Čule I, Drakonaki EE, Klauser AS. Ultrasound elastography in musculoskeletal radiology: past, present, and future. Semin Musculoskelet Radiol. 2020;24(2):156–66.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent
Informed consent was obtained from the subject described in this report.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Novais, C.M., Soares-de-Almeida, L., Garcia, J. et al. Pachydermodactyly: the role of ultrasonography, superb microvascular imaging, and elastography in diagnosis. Skeletal Radiol 51, 435–439 (2022). https://doi.org/10.1007/s00256-021-03887-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03887-5