Abstract
Background
Port-a-catheter insertion and removal are common procedures performed for children with chronic disease or cancer. Although its removal is usually straightforward, some difficulties during the procedure can be encountered. Several methods have been described in the literature to handle those cases where lines have become stuck.
Aim
To describe our simple technique in dealing with stuck port-a-catheters during removal. We will additionally report the incidence and factors associated with this complication.
Methods
A retrospective chart review study was performed between January 2009 and December 2019. Of a collective 2040 ports that were removed during the research interval, cases of difficult port removal were collected and reviewed. In 42 cases, catheter removal difficulty is encountered, and a second incision at the venous access site is performed. Failure of this procedure in removing the stuck catheter is then followed by catheter stenting and removal over a guide wire.
Results
Difficult removal of port-a-catheters was experienced in 42 cases (2%). The mean age at removal for those cases was 6.6 years. Most of the port-a-cath removals were done after treatment completion (74%). Ports had been left in situ for a mean duration of 44 months. The stepladder technique with wire stenting of the catheter was successful in 37 cases (88%), while the rest were only partially removed (distal part). The retained part was extracted using an angiographic technique. No short- or long-term complications were encountered in any of those 42 patients.
Conclusions
Stepladder with wire stenting of catheters approach deals with difficult line removals. Our technique is, therefore, simple, feasible, and effective.
Level of evidence
IV.
Similar content being viewed by others
Background
Implanted central venous catheters (infuse port catheters) are widely used in pediatric patients with malignancy or chronic diseases with long-term venous access needs. Indications for port-a-catheter removal include treatment completion, documented line sepsis, catheter fracture, blockage, or thrombosis. Port catheter removal is usually a simple procedure; however, retrieval of stuck, usually long-standing catheters, can be challenging [1,2,3], and the incidence of a stuck catheter has been reported with wide variation. The incidence range reported is 0.3 to 2.2% in various studies [4, 5]. Nonetheless, we believe that there is a lack of reporting, and data are scarce in general regarding this common procedure.
The pathogenesis behind the “stuck” catheter is related to forming a peri-catheter sleeve of fibrin sheath. Experimental studies on postmortem animals performed during the 14 days after catheter insertion confirmed the presence of foci of local intimal injury, endothelial denudation, and adherent thrombi [6, 7]. Several reports claim that long duration of use (> 20 months) and hematological disorders are the main predisposing factors associated with the difficult removal of the port-a-catheters [1, 4, 8]. In hematological patients, there was no clear pathogenesis for stuck catheters found in the literature to explain such predisposition. Catheters in these children are kept for a long time with multiple insertions because of the need for prolonged treatment such as chemotherapy. Also, catheter damage, fibrosis, and adhesion have been reported when the catheter is compressed between the clavicle and first rib and chronic friction (the pinch-off syndrome) [9].
Removal of a stuck catheter can be difficult, and forceful pulling of a stuck catheter alone without any safer technique of removal can lead to catheter breakage with consequent retention or migration of the broken fragment; even more, a catastrophic event may occur secondary to bleeding and rupture of the vessel wall [5, 10]. Some have reported that medium-term follow-up for children with retained catheter fragments has been unremarkable; however, those children are at risk of thrombosis, infectious complications, myocardial perforation, endocarditis, arrhythmias, and catheter migration to pulmonary vasculature with a potential risk of pulmonary embolism [1, 4, 8, 11].
Different techniques for dealing with stuck catheters have been described. Endoluminal balloon dilatation, the Hong technique, is the most used [12]. Huang et al. reported their experience with one patient utilizing a guide wire to separate the catheter from the vessel wall, recognized as a “push-in” force technique [13]. A migrated catheter can be retrieved by interventional radiology using an EN Snare device [3, 14]. The retained fragment is occasionally left in place or anchored to surrounding tissues to decrease migration risk [1, 15]. Migrated fragments may require a more invasive approach, including open sternotomy with pulmonary arteriotomy [16]. This study aims to describe our experience utilizing a relatively feasible and simple alternative technique for removing stuck port-a-catheters and reviewing the factors associated with such intraoperative difficulties.
Methodology
Patients and methods
A retrospective chart review was performed, including all children who had their port-a-catheters removed from January 2009 to December 2019. Demographic and clinical data were reviewed. Potential risk factors from the literature were sought. Descriptive data were generated.
Method of removal of stuck central lines
The steps of our simple technique named stepladder wire stenting of catheter approach start with the classic way of removing the catheter through a small incision at the port site, incision of the fibrous capsule over the port, followed by an attempt to retrieve the catheter. When resistance is found, a second 3-mm incision over the skin below the clavicle at the catheter entry site is made where the catheter is identified in the subcutaneous tissue and delivered with surrounding fibrous sheath out of the incision. Then sheath is opened without any venotomy, so no bleeding was encountered.
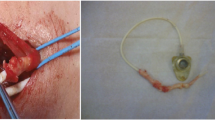
If the catheter is still stuck, it is cut, and proximal control of the retained catheter in the vein is achieved with a stitch or hemostat, and then a guide wire is inserted into the catheter and advanced beyond the tip of the catheter by 1–2 cm under C-arm fluoroscopic guidance (Fig. 1). A clamp was applied over the catheter and the inserted guide wire. The catheter is then retrieved along with the guide wire with gentle pulling, with the latter acting as a stent. Finally, a chest film (CXR) is done to confirm no retained fragments after the procedure (Fig. 2); all the above steps of the procedure are highlighted in the video submitted with subtitles (Video). The degree of difficulty experienced is graded in Table 1 using a modified Wilson grading system [1].
Results
A total of 2040 port-a-catheters were removed between 2009 and 2019. Of these, 42 (2%) cases involved difficult line removal, which constituted the population reviewed. Therefore, we have included only grades 3 and 4 to ensure an accurate inclusion of such challenging cases. There were 24 males and 18 females with a mean age of 6.6 years at the extraction time. All ports were from Bard Access System (Salt Lake City, Utah) and Celsite®. The catheter size was 4.5 Fr in 44% of cases, and the rest were 6.6 Fr.
The port-a-catheters insertion indications were cancer in 26 patients (62%); 17 of them had acute lymphocytic leukemia (Fig. 3). Thirty-one patients (74%) had their port-a-catheters removed after completion of treatment, while other indications for removal included infection and line dysfunction (Fig. 4). The mean time for catheter stay was 44 months, while the most prolonged duration was 8 years for one patient suffering from fibromatosis requiring immunosuppression therapy.
The average operative time for removing stuck lines with the stenting technique was 22.5 min, while 53 min were usually required if the catheter had to be replaced after removal. Most patients had their lines in the left subclavian vein (78.6%). Other less commonly used sites included external and internal jugular veins (10.5%); the risk of being stuck at these sites is less. Bleeding was not encountered much as stuck catheters were approached through the subcutaneous tissue.
In 5 patients (12%), the same venous site had been utilized earlier for line insertion before the current port insertions. We have not looked at all in 1998 removals regarding the incidence of reinsertion on previously utilized sites; hence, we cannot draw any conclusion about such association.
The degree of difficulty experienced is graded in Table 1 using a modified Wilson grading system [1]. However, it is sometimes difficult with retrospective reviews to ascertain the difference between grade 1 and grade 2 based on operative notes since the degree of difficulty of removal can either be missing or inaccurate.
In 42 patients, the catheter was difficult to remove despite traction at the port site, and thus, the incision used previously to obtain venous access was reopened, and the catheter was retrieved with the assistance of a guidewire stenting. This stenting technique was successful in 37 cases (88%). However, in the remaining 5 cases, the catheter was broken; therefore, they were referred for interventional radiology, and the fragments were removed successfully on the same day (Table 2).
Discussion
Most of the literature focuses on complications during line insertion or when the catheter is in situ, such as malfunction and infection. The complications encountered during central line removal in adults and pediatric populations are rarely discussed in the literature. We reported a 2% incidence of stuck lines, similar to previous reports [3,4,5]. The duration of catheter use for our patients was around 44 months; this supported the findings of Wilson, who reported statistically significant relations between those who had their port longer than 40 months and difficult line removal [1].
We observed a higher frequency of difficult catheter removal in acute lymphoblastic leukemia (ALL) patients (40%). Those findings are consistent with the previous report by Wilson, who had 76% of the stuck line with ALL [1]. Similarly, 2 of 3 patients in the Jones series also had lines placed for ALL. Thus, it may be possible that particular chemotherapeutic agents lead to this phenomenon [17]. Various methods for dealing with retained fragments have been described in the literature; Chen et al. described angiographic-assisted removal by an EN Snare device in their case series of four patients [8]. The technique described by Wilson and Jones included a second incision at the venous site followed by a venotomy if the catheter was still adherent and leaving a remnant in situ if it was not amenable for removal, while in our technique we just opened the fibrous sheath around the catheter without venotomy and getting distal catheter control for insertion of a guide wire. Once the guide wire beyond the tip of the catheter is confirmed by C-arm fluoroscopy followed by only gentle pulling of the catheter and guide wire as one piece, if there is a failure of this technique for retrieval, then the visible proximal catheter with the port is removed, and referring patient to interventional radiology for retrieval is recommended. We have never done venotomy in our cases as long as venotomy carries risks of major intraoperative bleeding and may be challenging to apply on our patients as the majority, 78.6%, had their line inserted in the subclavian vein. Furthermore, while leaving some remnant of the catheter showed good outcomes in the short term, there is still a risk of migration, infection, and thrombosis. This does not merely need further complex management, but it keeps parents of those patients with lifelong concerns [1, 17]. In addition, pulmonary hypertension secondary to the retention of a catheter fragment has been reported despite using anticoagulation, which ultimately leads to cor pulmonale and death [18].
Hong uses an endoluminal balloon angioplasty to expand the vein, which breaks the adhesions between the venous wall and the stuck catheter; he reported a single case done in an adult patient. Application of this might be difficult in small children with a risk of vein rupture due to small-sized and fragile veins [12]. Huang’s case report represents a similar technique to the one we are describing, where he inserted a guide wire to stent the catheter, and then he used a push in-pull out force to break the adhesions between the catheter and venous wall [13]. We used a pulling technique catheter and guide wire as one piece under fluoroscopic guidance.
We used a modified Wilson grading system to grade the difficulty with line removal on a scale of 0–4, while the patients with grades 3 and 4 were reviewed in detail for their characteristics.
No significant difference in duration in situ and age at insertion or removal was present among grades 3 and 4. Those findings were similar to that of Wilson [1].
All patients had a smooth recovery and were discharged on the same day. It is essential to follow up with those patients with CXR immediately after the procedure, if not done intraoperatively, to ensure no residual catheter was left in situ. The five patients whose catheters could not be removed with this technique were reported firmly adhering to the wall. All were discovered with CXR and were referred for angiographic removal performed on the same day without short-term or long-term complications.
Conclusion
This technique is easy, and feasible, and may eliminate the need for venotomy, sternotomy, or any other complex maneuvers to remove the stuck catheter. We recommend the stepladder wire stenting of catheter technique for all difficult removals of such lines to be complemented with the interventional procedures for unsuccessful ones.
Availability of data and materials
The data and material are available for review.
Abbreviations
- ALL:
-
Acute lymphoblastic leukemia
- CXR:
-
Chest X-ray
- Port-a-cath:
-
Infuse port catheters
References
Wilson GJP, van Noesel MM, Hop WCJ, van de Ven C. The catheter is stuck: complications experienced during removal of a totally implantable venous access device. A single-center. 2006.
Wall JL, Kierstead VL. Peripherally inserted central catheters: resistance to removal: a rare complication. J IntravenNurs. 1995;18(5):251–4.
Bawazir O. Management of stuck long. 2018. https://doi.org/10.24327/ijcar.2018.15678.2870.
Bautista F, Gomez-Chacon J, Costa E, et al. Retained intravascular fragments after removal of indwelling central venous catheters: a single institution experience. J Pediatr Surg. 2010;45:1491–5. https://doi.org/10.1016/j.jpedsurg.2010.02.001.
Aworanti O, Linnane N, Tareen F, Mortell A. Incidence and outcome of retained port-a-cath fragments during removal. Pediatr Surg Int. 2017;33(7):777-781. https://doi.org/10.1007/s00383-017-4103-6.
Xiang DZ, Verbeken EK, Van Lommel ETL, Stas M, De Wever I. Composition and formation of the sleeve enveloping a central venous catheter. J Vasc Surg. 1998;28:260–71.
Forauer AR, Theoharis C. Histological changes in the human vein wall adjacent to indwelling central venous catheters. J Vasc Intervent Radiol. 2003;14:1163–8.
Chan BKY, Rupasinghe SN, Hennessey I, et al. Retained central venous lines (CVLs) after attempted removal: an 11-year series and literature review. J Pediatr Surg. 2013;48:1887–91. https://doi.org/10.1016/j.jpedsurg.2013.01.050.
Andris DA, Krzywda EA, Schulte W, Ausman R, Quebbeman EJ. Pinch-off syndrome: a rare etiology for central venous catheter occlusion. JPEN J Parenter Enteral Nutr. 1994;18(6):531–3. https://doi.org/10.1177/0148607194018006531. PMID: 7602729.
Nakabayashi K, Nomura H, Isomura D, Sugiura R, Oka T. Successful retrieval of a dismembered central venous catheter stuck to the right pulmonary artery using a stepwise approach. Case Rep Cardiol. 2016;2016:6294263.
Lee D, Shaffer K. Wandering catheter through pulmonary vasculature. Radiology Case Reports. 2006;1:41.
Hong JH. A breakthrough technique for the removal of a hemodialysis catheter stuck in the central vein: endoluminal balloon dilatation of the stuck catheter. J Vasc Access. 2011;12(4):381–4.
Huang S-C, Tsai M-S, Lai H-S. A new technique to remove a ‘stuck’ totally implantable venous access catheter. J Pediatr Surg. 2009;44(7):1465–7.
Chen P-C, Chen C-J. Removal of retained port-a catheter in central lines in a pediatric population. Tzu Chi Med J. 2007;19(4):245–8.
Milbrandt K, Beaudry P, Anderson R, et al. A multi-institutional review of central venous line complications: retained intravascular fragments. J Pediatric Surg. 2009;44:972–6.
Peng CH, Tan PH, Chou AK, et al. Retention of broken central venous catheters in the pulmonary artery and inferior vena cava – a case report. Acta Anaesthesiol Sin. 1997;35(3):171–4.
Jones SA, Giacomantonio M. A complication associated with central line removal in the pediatric population: retained fixed catheter fragments. J Pediatric Surg. 2003;38:594–6.
Espiritu JD, Stolar CG. Pulmonary hypertension due to a retained totally implantable venous access device fragment. Chest. 2007;131:1574–6.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Each author in this research project has participated sufficiently in the work to take public responsibility for appropriate portions of the manuscript contents. The role of each author was assigned in the following categories: study conception and design, MA, MAA, ZA, and SA. Data acquisition, MA, MAA, and ZA. Analysis and data interpretation, MA, ZA, MAA, and SA. Drafting of the manuscript, MA and ZA. Critical revision, SA, MA, MAA, and ZA. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by our hospital’s IRB committee (RAC no. 2201133). It is a retrospective observational study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Video: Steps of procedure.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Awan, M.Y., Almatar, Z., AlShawa, M.A. et al. Difficult removal of implantable venous access system: stepladder approach with wire stenting of a catheter—single-center experience. Ann Pediatr Surg 19, 23 (2023). https://doi.org/10.1186/s43159-023-00254-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43159-023-00254-y