Abstract
Background
Magnetic resonance imaging (MRI) is used for neuroradiologic evaluation of patients with idiopathic growth hormone deficiency (IGHD).
Objectives
To compare pituitary height and morphology at MRI between patients with IGHD and controls.
Materials and methods
This retrospective study was conducted in pediatric patients, 3 years–15 years old, who had had brain MRI with non-contrast-enhanced midsagittal T1-weighted images. These images were measured for pituitary height and morphology of the pituitary gland including shape, stalk and posterior pituitary bright spot was evaluated.
Results
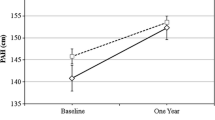
One hundred and nineteen patients were included, with 49 and 70 patients assigned to the study and control groups, respectively. Mean pituitary height was significantly less in the IGHD group than in the control group (3.81 mm±1.38 vs. 4.92 mm±1.13, retrospectively; P<0.001). Subgroup analysis revealed a significant difference in the pituitary height between groups in the prepubertal (8–10 years) and pubertal (11–13 years) periods (P=0.039 and P=0.006, respectively) and a trend toward significance in the postpubertal period (P=0.053). There was a significant difference in pituitary shape between IGHD and controls when combining grades III, IV and V (P=0.007). Other abnormal MRI findings of the pituitary stalk and posterior bright spot were significantly more often observed in the IGHD group (P<0.05).
Conclusion
Pituitary height was significantly smaller in patients with IGHD than in controls during prepuberty and puberty. Abnormal concave superior contour, hypoplastic stalk and absent/ectopic posterior bright spot were observed significantly more often among patients with IGHD.




Similar content being viewed by others
References
David W, Sara A (2016) Normal and aberrant growth in children. In: Shlomo M (ed) Williams textbook of endrocrinology, 13th edn. Elsevier Health Sciences, PA, p 965–1073
Alatzoglou KS, Dattani MT (2010) Genetic causes and treatment of isolated growth hormone deficiency—an update. Nat Rev Endocrinol 6:562–576
Kliegman S, Geme SS (2015) Nelson textbook of pediatrics. Elsevier Health Sciences, Philadelphia
Bozzola M, Adamsbaum C, Biscaldi I et al (1996) Role of magnetic resonance imaging in the diagnosis and prognosis of growth hormone deficiency. Clin Endocrinol 45:21–26
Zimmermann A, Schenk J-P, Grigorescu Sido P et al (2007) MRI findings and genotype analysis in patients with childhood onset growth hormone deficiency-correlation with severity of hypopituitarism. J Pediatr Endocrinol Metab 20:587–596
Hamilton J, Blaser S, Daneman D (1998) MR imaging in idiopathic growth hormone deficiency. AJNR Am J Neuroradiol 19:1609–1615
Elster A, Chen M, Williams D 3rd et al (1990) Pituitary gland: MR imaging of physiologic hypertrophy in adolescence. Radiology 174:681–685
Triulzi F, Scotti G, di Natale B et al (1994) Evidence of a congenital midline brain anomaly in pituitary dwarfs: a magnetic resonance imaging study in 101 patients. Pediatrics 93:409–416
Naderi F, Eslami SR, Mirak SA et al (2015) Effect of growth hormone deficiency on brain MRI findings among children with growth restrictions. J Pediatr Endocrinol Metab 28:117–123
Xue H, Xiu J, Huang Z et al (2014) Three-dimensional magnetic resonance volumetry of the pituitary gland is effective in detecting short stature in children. Exp Ther Med 8:551–556
Maghnie M, Ghirardello S, Genovese E (2004) Magnetic resonance imaging of the hypothalamuspituitary unit in children suspected of hypopituitarism: who, how and when to investigate. J Endocrinol Investig 27:496–509
Kornreich L, Horev G, Lazar L et al (1998) MR findings in growth hormone deficiency: correlation with severity of hypopituitarism. AJNR Am J Neuroradiol 19:1495–1499
Arslanoǧlu İ, Kutlu H, Işgüven P et al (2001) Diagnostic value of pituitary MRI in differentiation of children with normal growth hormone secretion, isolated growth hormone deficiency and multiple pituitary hormone deficiency. J Pediatr Endocrinol Metab 14:517–524
Lo FS, Chang LY, Yang MH et al (2004) Auxological, clinical and MRI findings in Taiwanese children with growth hormone deficiency. J Pediatr Endocrinol Metab 17:1519–1526
Chen S, Léger J, Garel C et al (1999) Growth hormone deficiency with ectopic neurohypophysis: anatomical variations and relationship between the visibility of the pituitary stalk asserted by magnetic resonance imaging and anterior pituitary function. J Clin Endocrinol Metab 84:2408–2413
Kandemir N, Yordam N, Cila A et al (2000) Magnetic resonance imaging in growth hormone deficiency: relationship between endocrine function and morphological findings. J Pediatr Endocrinol Metab 13:171–178
Liu M, Hu Y, Li G et al (2015) Low growth hormone levels in short-stature children with pituitary hyperplasia secondary to primary hypothyroidism. Int J Endocrinol 2015:283492. https://doi.org/10.1155/2015/283492
Takano K, Utsunomiya H, Ono H et al (1999) Normal development of the pituitary gland: assessment with three-dimensional MR volumetry. AJNR Am J Neuroradiol 20:312–315
Tsunoda A, Okuda O, Sato K (1997) MR height of the pituitary gland as a function of age and sex: especially physiological hypertrophy in adolescence and in climacterium. ANJR. Am J Neuroradiol 18:551–554
Acknowledgements
We gratefully acknowledge the Division of Pediatric Endocrinology, Department of Pediatrics, King Chulalongkorn Memorial Hospital for providing study data and Associate Professor Dr. Cameron Hurst for assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Rights and permissions
About this article
Cite this article
Dumrongpisutikul, N., Chuajak, A. & Lerdlum, S. Pituitary height at magnetic resonance imaging in pediatric isolated growth hormone deficiency. Pediatr Radiol 48, 694–700 (2018). https://doi.org/10.1007/s00247-018-4070-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4070-7