Abstract
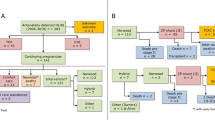
Predicting if a fetus with borderline left heart structures and coarctation of the aorta (CoA) will require single ventricle palliation (SVP) is challenging, partly due to the limitations of fetal echocardiography in defining valvar abnormalities. Fetal echocardiographic findings predictive of SVP, particularly in relation to the mitral valve (MV), are not well defined. We performed a retrospective review of fetuses with postnatally confirmed CoA from 2010 to 2020. Fetuses with complex congenital heart disease or unequivocal hypoplastic left heart syndrome were excluded. Data were compared between those who underwent biventricular repair (BVR) versus SVP, cardiac death or orthotopic heart transplant (OHT) to determine differences in fetal echocardiograms. Of 67 fetuses with 131 total echocardiograms, 62 (93%) underwent BVR and 5 (7%) experienced SVP, cardiac death or OHT. Fetuses with confirmed CoA who experienced SVP, cardiac death, or OHT, had fetal MV z-scores that were 2.03 lower, on average, than those who underwent BVR (z-score = − 3.98 vs. − 1.94, 95% CI − 2.93, − 1.13). The incidences of MV anomalies and left to right flow across the foramen ovale were higher in the SVP, cardiac death and OHT group. SVP, cardiac death or OHT in fetuses with confirmed CoA were associated with severe fetal MV hypoplasia, MV anomalies and left to right flow across the foramen ovale. These findings may help guide prenatal counseling about the likelihood of SVP, cardiac death or OHT in fetuses with CoA and borderline left heart structures.


Similar content being viewed by others
References
Buyens A, Gyselaers W, Coumans A et al (2012) Difficult prenatal diagnosis: fetal coarctation. Facts Views Vis ObGyn 4(4):230–236
Kaplinski M, Cohen MS (2015) Characterising adequacy or inadequacy of the borderline left ventricle: What tools can we use? Cardiol Young 25(8):1482–1488. https://doi.org/10.1017/S1047951115002267
Jantzen DW, Gelehrter SK, Yu S, Donohue JE, Fifer CG (2015) Echocardiographic factors discriminating biventricular versus univentricular approach in the foetus with borderline left ventricle. Cardiol Young 25(5):941–950. https://doi.org/10.1017/S1047951114001449
Weber RW, Ayala-Arnez R, Atiyah M et al (2013) Foetal echocardiographic assessment of borderline small left ventricles can predict the need for postnatal intervention. Cardiol Young 23(1):99–107. https://doi.org/10.1017/S1047951112000467
Haberer K, Fruitman D, Power A, Hornberger LK, Eckersley L (2021) Fetal echocardiographic predictors of biventricular circulation in hypoplastic left heart complex. Ultrasound Obstet Gynecol 58(3):405–410. https://doi.org/10.1002/uog.23558
Edwards LA, Arunamata A, Maskatia SA et al (2019) Fetal echocardiographic parameters and surgical outcomes in congenital left-sided cardiac lesions. Pediatr Cardiol 40(6):1304–1313. https://doi.org/10.1007/s00246-019-02155-7
Colquitt JL, Loar RW, Bolin EH, Ezon DS, Heinle JS, Morris SA (2022) Left heart hypoplasia in the fetus: echocardiographic predictors of outcome. Prenat Diagn 42(4):447–460. https://doi.org/10.1002/pd.6101
Viaux-Savelon S, Dommergues M, Rosenblum O et al (2012) Prenatal ultrasound screening: false positive soft markers may alter maternal representations and mother–infant interaction. PLoS ONE 7(1):e30935. https://doi.org/10.1371/journal.pone.0030935
Parameter(z). Accessed June 13, 2023. http://parameterz.blogspot.com/
R Workflow—13 Manipulation of Longitudinal Data. Accessed June 7, 2023. https://hbiostat.org/rflow/long.html#sec-long-interp
Toole BJ, Schlosser B, McCracken CE, Stauffer N, Border WL, Sachdeva R (2016) Importance of relationship between ductus and isthmus in fetal diagnosis of coarctation of aorta. Echocardiography 33(5):771–777. https://doi.org/10.1111/echo.13140
Kailin JA, Santos AB, Yilmaz Furtun B, Sexson Tejtel SK, Lantin-Hermoso R (2017) Isolated coarctation of the aorta in the fetus: a diagnostic challenge. Echocardiography 34(12):1768–1775. https://doi.org/10.1111/echo.13578
Quartermain MD, Cohen MS, Dominguez TE, Tian Z, Donaghue DD, Rychik J (2009) Left ventricle to right ventricle size discrepancy in the fetus: the presence of critical congenital heart disease can be reliably predicted. J Am Soc Echocardiogr 22(11):1296–1301. https://doi.org/10.1016/j.echo.2009.08.008
Jowett V, Aparicio P, Santhakumaran S, Seale A, Jicinska H, Gardiner HM (2012) Sonographic predictors of surgery in fetal coarctation of the aorta: sonographic predictors of fetal CoA. Ultrasound Obstet Gynecol 40(1):47–54. https://doi.org/10.1002/uog.11161
Fricke K, Liuba P, Weismann CG (2021) Fetal echocardiographic dimension indices: important predictors of postnatal coarctation. Pediatr Cardiol 42(3):517–525. https://doi.org/10.1007/s00246-020-02509-6
Conte S, Lacour-Gayet F, Serraf A et al (1995) Surgical management of neonatal coarctation. J Thorac Cardiovasc Surg 109(4):663–675. https://doi.org/10.1016/S0022-5223(95)70347-0
Feinstein JA, Benson DW, Dubin AM et al (2012) Hypoplastic left heart syndrome. J Am Coll Cardiol 59(11):S1–S42. https://doi.org/10.1016/j.jacc.2011.09.022
Sharland GK, Chita SK, Fagg NL et al (1991) Left ventricular dysfunction in the fetus: relation to aortic valve anomalies and endocardial fibroelastosis. Heart 66(6):419–424. https://doi.org/10.1136/hrt.66.6.419
McCaffrey FM, Sherman FS (1997) Prenatal diagnosis of severe aortic stenosis. Pediatr Cardiol 18(4):276–281. https://doi.org/10.1007/s002469900174
Axt-Fliedner R, Kreiselmaier P, Schwarze A, Krapp M, Gembruch U (2006) Development of hypoplastic left heart syndrome after diagnosis of aortic stenosis in the first trimester by early echocardiography. Ultrasound Obstet Gynecol 28(1):106–109. https://doi.org/10.1002/uog.2824
Allan LD, Sharland G, Tynan MJ (1989) The natural history of the hypoplastic left heart syndrome. Int J Cardiol 25(3):341–343. https://doi.org/10.1016/0167-5273(89)90226-X
Walsh MJ, Verghese GR, Ferguson ME et al (2017) Counseling practices for fetal hypoplastic left heart syndrome. Pediatr Cardiol 38(5):946–958. https://doi.org/10.1007/s00246-017-1601-1
Luo JL, Zhao BW, Pan M et al (2020) z-scores of early diastolic blood flow widths of mitral and tricuspid valves in normal fetuses and fetuses with dilated coronary sinus. J Matern Fetal Neonatal Med 33(9):1579–1586. https://doi.org/10.1080/14767058.2018.1523894
Gu X, Zhu H, Zhang Y et al (2019) Quantile score: a new reference system for quantitative fetal echocardiography based on a large multicenter study. J Am Soc Echocardiogr 32(2):296-302.e5. https://doi.org/10.1016/j.echo.2018.09.012
Acknowledgements
Daniel L. Saurers RDCS.
Funding
Supported in part by the Vanderbilt CTSA Grant UL1TR002243 from NCATS/NIH.
Author information
Authors and Affiliations
Contributions
A.F. and S.K. wrote the main manuscript and prepared all figures. A.K. and J.S. provided substantial contributions to the conception and design of the work. A.K. and J.S. also revised the work critically for important intellectual content. All authors reviewed the final manuscript to be published. D.S. is acknowledged for assistance in data collection.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose or other conflicts of interest to declare that are relevant to the content of this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Foy, A.J., Soslow, J.H., Kavanaugh-McHugh, A.L. et al. Mitral Valve Abnormalities Associated with Single-Ventricle Palliation, Cardiac Death or Transplant in Fetuses with Postnatally Confirmed Coarctation of the Aorta. Pediatr Cardiol (2023). https://doi.org/10.1007/s00246-023-03335-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03335-2