Abstract
Late-onset cardiovascular complications are serious concerns for pediatric cancer survivors (PCS) including those who are asymptomatic. We investigated whether cardiopulmonary exercise testing (CPET) can delineate the underlying pathophysiology of preclinical cardiovascular abnormalities in PCS. We examined CPET data via cycle ergometer in asymptomatic PCS with normal echocardiogram and age-matched controls. Peak and submaximal parameters were analyzed. Fifty-three PCS and 60 controls were studied. Peak oxygen consumption (VO2), peak work rate (WR), and ventilatory anaerobic threshold (VAT) were significantly lower in PCS than controls (1.86 ± 0.53 vs. 2.23 ± 0.61 L/min, 125 ± 45 vs. 154 ± 46 W, and 1.20 ± 0.35 vs. 1.42 ± 0.43 L/min, respectively; all p < 0.01), whereas peak heart rate (HR) and ventilatory efficiency (a slope of minute ventilation over CO2 production or ∆VE/∆VCO2) were comparable. Peak respiratory exchange ratio (RER) was significantly higher in PCS (p = 0.0006). Stroke volume (SV) reserve was decreased in PCS, indicated by simultaneous higher dependency on HR (higher ∆HR/∆WR) and lower peak oxygen pulse (OP). Twelve PCS with high peak RER (≥ 1.3) revealed lower pVO2 and VAT than the rest of PCS despite higher ventilatory efficiency (lower ∆VE/∆VCO2), suggesting fundamental deficiency in oxygen utilization in some PCS. Poor exercise performance in PCS may be mainly attributed to limited stroke volume reserve, but the underlying pathophysiology is multifactorial. Combined assessment of peak and submaximal CPET parameters provided critical information in delineating underlying exercise physiology of PCS.






Similar content being viewed by others
References
Robison LL, Hudson MM (2014) Survivors of childhood and adolescent cancer: life-long risks and responsibilities. Nat Rev Cancer 14:61–70
Chow EJ, Leger KJ, Bhatt NS, Mulrooney DA, Ross CJ, Aggarwal S, Bansal N, Ehrhardt MJ, Armenian SH, Scott JM, Hong B (2019) Paediatric cardio-oncology: epidemiology, screening, prevention, and treatment. Cardiovasc Res 115:922–934
Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, Friedman DL, Marina N, Hobbie W, Kadan-Lottick NS, Schwartz CL, Leisenring W, Robison LL, Childhood Cancer Survivor S (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355:1572–1582
Toro-Salazar OH, Gillan E, O’Loughlin MT, Burke GS, Ferranti J, Stainsby J, Liang B, Mazur W, Raman SV, Hor KN (2013) Occult cardiotoxicity in childhood cancer survivors exposed to anthracycline therapy. Circ Cardiovasc Imaging 6:873–880
Armenian SH, Hudson MM, Mulder RL, Chen MH, Constine LS, Dwyer M, Nathan PC, Tissing WJ, Shankar S, Sieswerda E, Skinner R, Steinberger J, van Dalen EC, van der Pal H, Wallace WH, Levitt G, Kremer LC, International Late Effects of Childhood Cancer Guideline Harmonization G (2015) Recommendations for cardiomyopathy surveillance for survivors of childhood cancer: a report from the International Late Effects of Childhood Cancer Guideline Harmonization Group. Lancet Oncol 16:e123-136
Kaneko S, Tham EB, Haykowsky MJ, Spavor M, Khoo NS, Mackie AS, Smallhorn JF, Thompson RB, Nelson MD (2016) Impaired left ventricular reserve in childhood cancer survivors treated with anthracycline therapy. Pediatr Blood Cancer 63:1086–1090
Powell AW, Nagarajan R, Mays WA, Chin C, Knilans TK, Knecht SK, Amos MA, Gerdes YM, Ryan TD (2018) Cardiopulmonary aerobic fitness assessment during maximal and submaximal exercise testing in pediatric oncology patients after chemotherapy. Am J Clin Oncol. https://doi.org/10.1097/COC.0000000000000422
De Caro E, Smeraldi A, Trocchio G, Calevo M, Hanau G, Pongiglione G (2011) Subclinical cardiac dysfunction and exercise performance in childhood cancer survivors. Pediatr Blood Cancer 56:122–126
Miller AM, Lopez-Mitnik G, Somarriba G, Lipsitz SR, Hinkle AS, Constine LS, Lipshultz SE, Miller TL (2013) Exercise capacity in long-term survivors of pediatric cancer: an analysis from the Cardiac Risk Factors in Childhood Cancer Survivors Study. Pediatr Blood Cancer 60:663–668
Baba R, Nagashima M, Goto M, Nagano Y, Yokota M, Tauchi N, Nishibata K (1996) Oxygen uptake efficiency slope: a new index of cardiorespiratory functional reserve derived from the relation between oxygen uptake and minute ventilation during incremental exercise. J Am Coll Cardiol 28:1567–1572
Lipshultz SE, Lipsitz SR, Sallan SE, Dalton VM, Mone SM, Gelber RD, Colan SD (2005) Chronic progressive cardiac dysfunction years after doxorubicin therapy for childhood acute lymphoblastic leukemia. J Clin Oncol 23:2629–2636
Chen MH, Colan SD, Diller L (2011) Cardiovascular disease: cause of morbidity and mortality in adult survivors of childhood cancers. Circ Res 108:619–628
Slieker MG, Fackoury C, Slorach C, Hui W, Friedberg MK, Fan CS, Manlhiot C, Dillenburg R, Kantor P, Mital S, Liu P, Nathan PC, Mertens L (2019) Echocardiographic assessment of cardiac function in pediatric survivors of anthracycline-treated childhood cancer. Circ Cardiovasc Imaging 12:e008869
Mulrooney DA, Hyun G, Ness KK, Ehrhardt MJ, Yasui Y, Duprez D, Howell RM, Leisenring WM, Constine LS, Tonorezos E, Gibson TM, Robison LL, Oeffinger KC, Hudson MM, Armstrong GT (2020) Major cardiac events for adult survivors of childhood cancer diagnosed between 1970 and 1999: report from the Childhood Cancer Survivor Study cohort. BMJ 368:l6794
Tilemann LM, Heckmann MB, Katus HA, Lehmann LH, Muller OJ (2018) Cardio-oncology: conflicting priorities of anticancer treatment and cardiovascular outcome. Clin Res Cardiol 107:271–280
Akam-Venkata J, Franco VI, Lipshultz SE (2016) Late cardiotoxicity: issues for childhood cancer survivors. Curr Treat Options Cardiovasc Med 18:47
Armstrong GT, Joshi VM, Ness KK, Marwick TH, Zhang N, Srivastava D, Griffin BP, Grimm RA, Thomas J, Phelan D, Collier P, Krull KR, Mulrooney DA, Green DM, Hudson MM, Robison LL, Plana JC (2015) Comprehensive echocardiographic detection of treatment-related cardiac dysfunction in adult survivors of childhood cancer: results from the St. Jude Lifetime Cohort Study. J Am Coll Cardiol 65:2511–2522
Sato T, Harada K, Tamura M, Watanabe A, Ishii M, Takada G (2001) Cardiorespiratory exercise capacity and its relation to a new Doppler index in children previously treated with anthracycline. J Am Soc Echocardiogr 14:256–263
Hauser M, Gibson BS, Wilson N (2001) Diagnosis of anthracycline-induced late cardiomyopathy by exercise-spiroergometry and stress-echocardiography. Eur J Pediatr 160:607–610
Christiansen JR, Kanellopoulos A, Lund MB, Massey R, Dalen H, Kiserud CE, Ruud E, Aakhus S (2015) Impaired exercise capacity and left ventricular function in long-term adult survivors of childhood acute lymphoblastic leukemia. Pediatr Blood Cancer 62:1437–1443
Guimaraes-Filho FV, Tan DM, Braga JC, Rodrigues A, Waib PH, Matsubara BB (2012) Ventricular systolic reserve in asymptomatic children previously treated with low doses of anthracyclines: a longitudinal, prospective exercise echocardiography study. Pediatr Blood Cancer 59:548–552
Cifra B, Chen CK, Fan CS, Slorach C, Manlhiot C, McCrindle BW, Dragulescu A, Redington AN, Friedberg MK, Nathan PC, Mertens L (2018) Dynamic myocardial response to exercise in childhood cancer survivors treated with anthracyclines. J Am Soc Echocardiogr 31:933–942
Ryerson AB, Border WL, Wasilewski-Masker K, Goodman M, Meacham L, Austin H, Mertens AC (2015) Assessing anthracycline-treated childhood cancer survivors with advanced stress echocardiography. Pediatr Blood Cancer 62:502–508
Ness KK, Plana JC, Joshi VM, Luepker RV, Durand JB, Green DM, Partin RE, Santucci AK, Howell RM, Srivastava DK, Hudson MM, Robison LL, Armstrong GT (2020) Exercise intolerance, mortality, and organ system impairment in adult survivors of childhood cancer. J Clin Oncol 38:29–42
Haykowsky MJ, Beaudry R, Brothers RM, Nelson MD, Sarma S, La Gerche A (2016) Pathophysiology of exercise intolerance in breast cancer survivors with preserved left ventricular ejection fraction. Clin Sci (Lond) 130:2239–2244
Mendonca GV, Pezarat-Correia P, Vaz JR, Silva L, Heffernan KS (2017) Impact of aging on endurance and neuromuscular physical performance: the role of vascular senescence. Sports Med 47:583–598
Abe J, Martin JF, Yeh ET (2016) The future of onco-cardiology: we are not just “Side Effect Hunters.” Circ Res 119:896–899
Johnson D, Perrault H, Fournier A, Leclerc JM, Bigras JL, Davignon A (1997) Cardiovascular responses to dynamic submaximal exercise in children previously treated with anthracycline. Am Heart J 133:169–173
Foulkes S, Costello BT, Howden EJ, Janssens K, Dillon H, Toro C, Claus P, Fraser SF, Daly RM, Elliott DA, Conyers R, La Gerche A (2020) Exercise cardiovascular magnetic resonance reveals reduced cardiac reserve in pediatric cancer survivors with impaired cardiopulmonary fitness. J Cardiovasc Magn Reson 22:64
Mezzani A, Corra U, Bosimini E, Giordano A, Giannuzzi P (2003) Contribution of peak respiratory exchange ratio to peak VO2 prognostic reliability in patients with chronic heart failure and severely reduced exercise capacity. Am Heart J 145:1102–1107
Ramos-Jimenez A, Hernandez-Torres RP, Torres-Duran PV, Romero-Gonzalez J, Mascher D, Posadas-Romero C, Juarez-Oropeza MA (2008) The respiratory exchange ratio is associated with fitness indicators both in trained and untrained men: a possible application for people with reduced exercise tolerance. Clin Med Circ Respirat Pulm Med 2:1–9
Rayar M, Webber CE, Nayiager T, Sala A, Barr RD (2013) Sarcopenia in children with acute lymphoblastic leukemia. J Pediatr Hematol Oncol 35:98–102
Scheede-Bergdahl C, Jagoe RT (2013) After the chemotherapy: potential mechanisms for chemotherapy-induced delayed skeletal muscle dysfunction in survivors of acute lymphoblastic leukaemia in childhood. Front Pharmacol 4:49
Gavin TP (2009) Basal and exercise-induced regulation of skeletal muscle capillarization. Exerc Sport Sci Rev 37:86–92
Jarvela LS, Niinikoski H, Lahteenmaki PM, Heinonen OJ, Kapanen J, Arola M, Kemppainen J (2010) Physical activity and fitness in adolescent and young adult long-term survivors of childhood acute lymphoblastic leukaemia. J Cancer Surviv 4:339–345
Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema JE, Sun X-G, Whipp BJ (2012) Measurements during integrative cardiopulmonary exercise testing. In: Wasserman K, Hansen JE, Sue DY, Stringer WW, Sietsema JE, Sun X-G, Whipp BJ (eds) Principles of exercise testing and interpretation. Wolters Kluwer, Lippincott Williams & Wilkins, Philadelphia, pp 71–106
Toyofuku M, Takaki H, Sugimachi M, Kawada T, Goto Y, Sunagawa K (2003) Reduced oxygen uptake increase to work rate increment (DeltaVO2/DeltaWR) is predictable by VO2 response to constant work rate exercise in patients with chronic heart failure. Eur J Appl Physiol 90:76–82
Takken T, Blank AC, Hulzebos EH, van Brussel M, Groen WG, Helders PJ (2009) Cardiopulmonary exercise testing in congenital heart disease: (contra)indications and interpretation. Neth Heart J 17:385–392
Cooper DM, Leu SY, Galassetti P, Radom-Aizik S (2014) Dynamic interactions of gas exchange, body mass, and progressive exercise in children. Med Sci Sports Exerc 46:877–886
Espinosa T, de Los MC, Harteveld LM, Kuipers IM, Rammeloo L, Hazekamp MG, Blom NA, Ten Harkel ADJ (2021) Prognostic value of maximal and submaximal exercise performance in Fontan patients < 15 years of age. Am J Cardiol 154:92–98
Dallaire F, Wald RM, Marelli A (2017) The role of cardiopulmonary exercise testing for decision making in patients with repaired Tetralogy of Fallot. Pediatr Cardiol 38:1097–1105
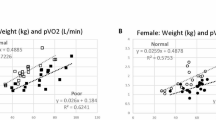
Kernizan D, Glass A, D’Aloisio G, Hossain J, Tsuda T (2022) A combined analysis of peak and submaximal exercise parameters in delineating underlying mechanisms of sex differences in healthy adolescents. Pediatr Cardiol. https://doi.org/10.1007/s00246-022-02832-0
Chicco AJ, Schneider CM, Hayward R (2006) Exercise training attenuates acute doxorubicin-induced cardiac dysfunction. J Cardiovasc Pharmacol 47:182–189
Kouzi SA, Uddin MN (2016) Aerobic exercise training as a potential cardioprotective strategy to attenuate doxorubicin-induced cardiotoxicity. J Pharm Pharm Sci 19:399–410
Acknowledgements
We thank the Nemours Summer Student Research Program offered by Nemours Children’s Health, Wilmington, DE (for A. G.). We also acknowledge DE-CTR ACCEL program for biostatistics support. The authors thank Ms. Theresa Michel for editing the manuscript text.
Funding
Authors received no external funding for this study.
Author information
Authors and Affiliations
Contributions
TT primarily conceptualized and designed the study and organized the research team. Material preparation, data collection, and analysis of cardiopulmonary exercise testing (CPET) were performed by TT, DK, AG, and GD’A. JH is a biostatistician who carefully analyzed the entire data and provided critical suggestions regarding statistics. JQ oversees the Oncology Survivorship Program, which provided the patients’ medical information regarding diagnosis and treatment of primary disease and their current clinical status. The first draft of the manuscript was written by TT, and all authors commented on the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
IRB Information
Nemours Office of Human Subject Protection (1438331).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
246_2022_2995_MOESM1_ESM.pptx
Supplementary file1 (PPTX 72 KB)—Supplemental Figure 1. Submaximal slope parameters. A A cardiopulmonary exercise test (CPET) worksheet of a 17-year-old male with acute lymphoblastic leukemia (ALL) who is now off-treatment. B A slope of work rate (WR) and oxygen consumption (VO2) (∆VO2/∆WR). C A slope of WR and heart rate (HR) (∆HR/∆WR). D A slope of HR and VO2* (∆VO2*/∆HR). E Oxygen uptake efficiency slope (OUES), where x-axis is log10[minute ventilation (VE)] and y-axis is VO2, and F A slope of minute ventilation (VE) and VCO2. There is an excellent correlation among these parameters during submaximal exercise phase.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tsuda, T., Kernizan, D., Glass, A. et al. Cardiopulmonary Exercise Testing Characterizes Silent Cardiovascular Abnormalities in Asymptomatic Pediatric Cancer Survivors. Pediatr Cardiol 44, 344–353 (2023). https://doi.org/10.1007/s00246-022-02995-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02995-w