Abstract
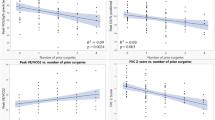
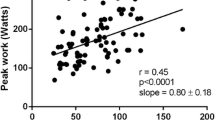
Two standard surgical palliative options for neonates born with pulmonary atresia and intact ventricular septum (PA/IVS) include uni-or biventricular repair. Whenever feasible, the biventricular repair is considered to have better exercise capacity (XC) and outcomes. However, there is a paucity of data comparing objective XC between these two surgical techniques. Our aim was to compare XC, including longitudinal changes in patients with PA/IVS following uni-biventricular repair. We performed a single-center retrospective study of survivors with repaired PA/IVS who underwent comprehensive treadmill cardiopulmonary exercise testing. Initial and latest exercise parameters were compared for longitudinal analysis. Demographic and exercise parameters were collated. Peak oxygen uptake (VO2 in ml/kg/min), an indicator of maximal aerobic capacity, peak heart rate, and other measures of spirometry performed at the same time were collected. Recorded parameters included, (a) Percentage of predicted VO2 (% VO2) normalized for age, weight, height, and gender, (b) % oxygen (O2) pulse, (c) anaerobic threshold (AT), (d) Chronotropic index (CI), (e) % Breathing reserve, (f) Forced vital capacity (FVC), (g) % Forced Expiratory volume in 1 s (FEV1), (h) Maximum voluntary ventilation (MVV), and (i) VE/VCO2. Appropriate statistical tests were performed, and a p value < 0.05 was considered significant. A total of 35 patients (43% male, 57% univentricular repair) were included, with a mean (SD) age of 20.1(7.5) years. Patients with univentricular palliation demonstrated significantly impaired peak heart rate, chronotropic index (0.50 ± 0.2 vs. 0.90 ± 0.1, p = 0.02), VE/VCO2 (35.4 ± 5.0 vs. 30.2 ± 2.8, p = 0.001), and %FVC (78.3 ± 8.3 vs. 88.6 ± 15.1, p = 0.02). There was a trend towards reduction in % VO2 in the Fontan patients though it was statistically similar between the groups (68.4 ± 21.4 vs. 81.2 ± 18.9, p = 0.07). Longitudinal data were available for 11 patients in each group, and there was no longitudinal decline in their exercise parameters over similar intermediate follow-up duration [6.8 (UV) vs. 5.3 (BV) years]. We conclude that young survivors with PA/IVS with prior univentricular palliation demonstrated an objective impairment in their chronotropic parameters compared with the biventricular repair. However, this did not translate into a significant difference in their exercise capacity. There was no longitudinal decline in exercise capacity or other parameters over intermediate follow-up.
Similar content being viewed by others
Abbreviations
- ACE:
-
Angiotensin-converting enzyme
- AV:
-
Atrioventricular
- BMI:
-
Body mass index
- BP:
-
Blood pressure
- BV:
-
Biventricular
- CHD:
-
Congenital heart disease
- CI:
-
Chronotropic index
- CO2 :
-
Carbon dioxide
- EKG:
-
Electrocardiogram
- FEV1:
-
Forced expiratory volume in 1 s
- FVC:
-
Forced vital capacity
- HR:
-
Heart rate
- IRB:
-
Institutional review board
- LV:
-
Left ventricle
- METS:
-
Metabolic equivalents
- MV:
-
Minute ventilation
- MVV:
-
Maximum voluntary ventilation
- O2 :
-
Oxygen
- PA:
-
Pulmonary artery
- PA/IVS:
-
Pulmonary atresia/intact ventricular septum
- PFT:
-
Pulmonary function test
- RV:
-
Right ventricle
- RVOT:
-
Right ventricular outflow tract
- SD:
-
Standard deviation
- SpO2 :
-
Oxygen saturation
- TOF:
-
Tetralogy of fallot
- UV:
-
Univentricular
- VAT:
-
Ventilatory anaerobic threshold
- VCO2 :
-
Carbon dioxide elimination
- VE:
-
Pulmonary ventilation
- VO2 :
-
Peak oxygen uptake
- XC:
-
Exercise capacity
References
Nykanen DG (2013) Pulmonary atresia and intact ventricular septum. In: Moss and Adams’ heart disease in infants, children, and adolescents: including the fetus and young adult, 8th edn. Lippincott Williams & Wilkins, Philadelphia, pp 939–959
Dyamenahalli U, McCrindle BW, McDonald C et al (2004) Pulmonary atresia with intact ventricular septum: management of, and outcomes for, a cohort of 210 consecutive patients. Cardiol Young 14:299–308. https://doi.org/10.1017/S1047951104003087
Inuzuka R, Diller GP, Borgia F et al (2012) Comprehensive use of cardiopulmonary exercise testing identifies adults with congenital heart disease at increased mortality risk in the medium term. Circulation 125:250–259. https://doi.org/10.1161/CIRCULATIONAHA.111.058719
Diller GP, Dimopoulos K, Okonko D et al (2005) Exercise intolerance in adult congenital heart disease: comparative severity, correlates, and prognostic implication. Circulation 112:828–835. https://doi.org/10.1161/CIRCULATIONAHA.104.529800
Goldberg DJ, Avitabile CM, McBride MG, Paridon SM (2013) Exercise capacity in the Fontan circulation. Cardiol Young 23:824–830. https://doi.org/10.1017/S1047951113001649
Sanghavi DM, Flanagan M, Powell AJ et al (2006) Determinants of exercise function following univentricular versus biventricular repair for pulmonary atresia/intact ventricular septum. Am J Cardiol 97:1638–1643. https://doi.org/10.1016/j.amjcard.2005.12.057
Romeih S, Groenink M, Roest AAW et al (2012) Exercise capacity and cardiac reserve in children and adolescents with corrected pulmonary atresia with intact ventricular septum after univentricular palliation and biventricular repair. J Thorac Cardiovasc Surg 143:569–575. https://doi.org/10.1016/j.jtcvs.2011.08.012
Ekman-Joelsson BM, Gustafsson PM, Sunnegårdh J (2009) Exercise performance after surgery for pulmonary atresia and intact ventricular septum. Pediatr Cardiol 30:752–762. https://doi.org/10.1007/s00246-009-9423-4
Karamlou T, Poynter JA, Walters HL et al (2013) Long-term functional health status and exercise test variables for patients with pulmonary atresia with intact ventricular septum: a congenital Heart surgeons Society study. J Thorac Cardiovasc Surg 145:1018-1027.e3. https://doi.org/10.1016/j.jtcvs.2012.11.092
Fletcher GF, Ades PA, Kligfield P et al (2013) Exercise standards for testing and training: a scientific statement from the American heart association. Circulation 128:873–934. https://doi.org/10.1161/CIR.0b013e31829b5b44
Wilkoff BL, Miller RE (1992) Exercise testing for chronotropic assessment. Cardiol Clin 10(4):705–17
Powell AW, Veldtman G (2020) Heart rate responses during exercise by dominant ventricle in pediatric and young adult patients with a Fontan circulation. Can J Cardiol 36:1508–1515. https://doi.org/10.1016/j.cjca.2019.10.042
Ohuchi H, Arakaki Y, Yagihara T, Kamiya T (1997) Cardiorespiratory responses to exercise after repair of the univentricular heart. Int J Cardiol 58:17–30. https://doi.org/10.1016/S0167-5273(96)02848-3
Gewillig MH, Lundström UR, Bull C et al (1990) Exercise responses in patients with congenital heart disease after Fontan repair: patterns and determinants of performance. J Am Coll Cardiol 15:1424–1432. https://doi.org/10.1016/S0735-1097(10)80034-8
Claessen G, La Gerche A, Van De Bruaene A et al (2019) Heart rate reserve in Fontan patients: chronotropic incompetence or hemodynamic limitation? J Am Heart Assoc 8:1–10. https://doi.org/10.1161/JAHA.119.012008
Alonso-Gonzalez R, Borgia F, Diller GP et al (2013) Abnormal lung function in adults with congenital heart disease: prevalence, relation to cardiac anatomy, and association with survival. Circulation 127:882–890. https://doi.org/10.1161/CIRCULATIONAHA.112.126755
Ginde S, Bartz PJ, Hill GD et al (2013) Restrictive lung disease is an independent predictor of exercise intolerance in the adult with congenital heart disease. Congenit Heart Dis 8:246–254. https://doi.org/10.1111/chd.12010
Fredriksen PM, Therrien J, Veldtman G et al (2001) Lung function and aerobic capacity in adult patients following modified Fontan procedure. Heart 85:295–299. https://doi.org/10.1136/heart.85.3.295
Callegari A, Neidenbach R, Milanesi O et al (2019) A restrictive ventilatory pattern is common in patients with univentricular heart after Fontan palliation and associated with a reduced exercise capacity and quality of life. Congenit Heart Dis 14:147–155. https://doi.org/10.1111/chd.12694
Opotowsky AR, Landzberg MJ, Earing MG et al (2014) Abnormal spirometry after the Fontan procedure is common and associated with impaired aerobic capacity. Am J Physiol 307:110–117. https://doi.org/10.1152/ajpheart.00184.2014
Matthews IL, Fredriksen PM, Bjørnstad PG et al (2006) Reduced pulmonary function in children with the Fontan circulation affects their exercise capacity. Cardiol Young 16:261–267. https://doi.org/10.1017/S1047951106000345
Udholm S, Aldweib N, Hjortdal VE, Veldtman GR (2018) Prognostic power of cardiopulmonary exercise testing in Fontan patients: a systematic review. Open Heart. https://doi.org/10.1136/openhrt-2018-000812
Atz AM, Zak V, Mahony L et al (2017) Longitudinal outcomes of patients with single ventricle after the Fontan procedure. J Am Coll Cardiol 69:2735–2744. https://doi.org/10.1016/j.jacc.2017.03.582
Kipps AK, Graham DA, Harrild DM et al (2011) Longitudinal exercise capacity of patients with repaired tetralogy of Fallot. Am J Cardiol 108:99–105. https://doi.org/10.1016/j.amjcard.2011.02.349
Eshuis G, Hock J, Sarvaas MDG et al (2021) Exercise capacity in patients with repaired Tetralogy of Fallot aged 6 to 63 years. Heart. https://doi.org/10.1136/heartjnl-2020-318928
Egbe A, Khan AR, Miranda WR et al (2018) Mechanism for temporal changes in exercise capacity after Fontan palliation: role of doppler echocardiography. Am Heart J 196:144–152. https://doi.org/10.1016/j.ahj.2017.10.010
Lévy M, Danel C, Tamisier D et al (2002) Histomorphometric analysis of pulmonary vessels in single ventricle for better selection of patients for the Fontan operation. J Thorac Cardiovasc Surg 123:263–270. https://doi.org/10.1067/mtc.2002.119697
Pushparajah K, Wong JK, Bellsham-Revell HR et al (2016) Magnetic resonance imaging catheter stress haemodynamics post-Fontan in hypoplastic left heart syndrome. Eur Heart J Cardiovasc Imaging 17:644–651. https://doi.org/10.1093/ehjci/jev178
Ono M, Vogt M, Cleuziou J et al (2016) Improved exercise performance in patients with tricuspid atresia after the Fontan-björk modification with pulsatile systolic pulmonary flow. Ann Thorac Surg 101:1012–1019. https://doi.org/10.1016/j.athoracsur.2015.09.085
Rhodes J, Garofano RP, Bowman FO et al (1990) Effect of right ventricular anatomy on the cardiopulmonary response to exercise: implications for the fontan procedure. Circulation 81:1811–1817. https://doi.org/10.1161/01.CIR.81.6.1811
Hickey EJ, Caldarone CA, Blackstone EH et al (2007) Critical left ventricular outflow tract obstruction: the disproportionate impact of biventricular repair in borderline cases. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2007.07.052
Author information
Authors and Affiliations
Contributions
Anusha Konduri: Acquisition of data, analysis and interpretation of data, drafting the manuscript Sanjeev Aggarwal: Conception and design of study, analysis and interpretation of data, drafting the manuscript Chenni Sriram: Analysis and interpretation of data, drafting the manuscript Deemah Mahadin: Analysis and interpretation of data, drafting the manuscript All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors do not have any conflict of interest, financial or otherwise, to disclose. No Grants were utilized.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Konduri, A., Sriram, C., Mahadin, D. et al. Exercise Capacity in Patients with Pulmonary Atresia with Intact Ventricular Septum: Does the Type of Surgical Repair Matter?. Pediatr Cardiol 44, 556–563 (2023). https://doi.org/10.1007/s00246-022-02943-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-022-02943-8