Abstract
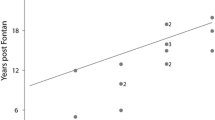
This investigation analyzed the rate of hepatic fibrosis progression in post-Fontan patients that underwent hepatic biopsy. The study cohort comprised post-Fontan patients that underwent cardiac catheterization and transvenous liver biopsy between March 2012 and September 2019. We identified 126 patients that met inclusion criteria. Of the 126, 27 (21%) had a lateral tunnel Fontan, and 99 (79%) had an extracardiac Fontan. For the 27 lateral tunnel Fontan patients, age at Fontan was 4 ± 2 years, and for the 99 extracardiac Fontan patients age at Fontan was 4 ± 2 years (p = 0.98). For the 27 lateral tunnel Fontan patients, the average total fibrosis score was 3.0 ± 1.5; and for the 99 extracardiac Fontan patients, the average total fibrosis was 2.7 ± 1.7 (p = 0.48). For the lateral tunnel Fontan patients, the average Fontan duration was 20 ± 6 years; and for the 99 extracardiac Fontan patients, the average Fontan duration was 11 ± 5 years (p < 0.001). For the 27 lateral tunnel Fontan patients, the average rate of fibrosis progression was 0.16 ± 0.10 total fibrosis score/year; and for the 99 extracardiac Fontan patients, the average rate of fibrosis progression was 0.30 ± 0.23 total fibrosis score/year (p < 0.001). In conclusion, our findings suggest that those with extracardiac Fontans have a faster rate of hepatic fibrosis progression than those with lateral tunnel Fontans. More extensive or multi-institutional studies will be needed to confirm these findings and define the clinical significance of discrepant rates of hepatic fibrosis in post-Fontan patients.
Similar content being viewed by others
References
Poynard BP, Opolon P (1997) Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet 349:825–832
Myers RP, Patel K, Pianko S, Poynard T, McHutchison JG (2003) The rate of fibrosis progression is an independent predictor of the response to antiviral therapy in chronic hepatitis C. J Viral Hepat 10:16–22
Sebagh M, Rifai K, Féray C, Yilmaz F, Falissard B, Roche B, Bismuth H, Samuel D, Reynès M (2003) All liver recipients benefit from the protocol 10-year liver biopsies. Hepatology 37:1293–1301
Hoefs JC, Shiffman ML, Goodman ZD, Kleiner DE, Dienstag JL, Stoddard AM, HALT-C Trial Group (2011) Rate of progression of hepatic fibrosis in patients with chronic hepatitis C: results from the HALT-C Trial. Gastroenterology 141(900):908
Howell J, Sawhney R, Angus P, Fink M, Jones R, Wang BZ, Visvanathan K, Crowley P, Gow P (2013) Identifying the superior measure of rapid fibrosis for predicting premature cirrhosis after liver transplantation for hepatitis C. Transpl Infect Dis 15:588–599
Rüeger S, Bochud PY, Dufour JF et al (2015) Impact of common risk factors of fibrosis progression in chronic hepatitis C. Gut 64:1605–1615
Sarkar M, Dodge JL, Greenblatt RM, Kuniholm MH, DeHovitz J, Plankey M, Kovacs A, French AL, Seaberg EC, Ofotokun I, Fischl M, Overton E, Kelly E, Bacchetti P, Peters MG, Women’s Interagency HIV Study (2017) Reproductive aging and hepatic fibrosis progression in human immunodeficiency virus/hepatitis C virus-coinfected women. Clin Infect Dis 65(1695):1702
Trout AT, Sheridan RM, Serai SD, Xanthakos SA, Su W, Zhang B, Wallihan DB (2018) Diagnostic performance of MR elastography for liver fibrosis in children and young adults with a spectrum of liver diseases. Radiology 287:824–832
Silvilairat S, Cabalka AK, Cetta F, Grogan M, Hagler DJ, O'Leary PW (2008) Protein-losing enteropathy after the Fontan operation: associations and predictors of clinical outcome. Congenit Heart Dis 3:262–268
Daniels CJ, Bradley EA, Landzberg MJ, Aboulhosn J, Beekman RH 3rd, Book W, Gurvitz M, John A, John B, Marelli A, Marino BS, Minich LL, Poterucha JJ, Rand EB, Veldtman GR (2017) Fontan-associated liver disease: proceedings from the American College of Cardiology Stakeholders Meeting, October 1 to 2, 2015, Washington DC. J Am Coll Cardiol 70:3173–3194
Schwartz MC, Sullivan LM, Glatz AC, Rand E, Russo P, Goldberg DJ, Rome JJ, Cohen MS (2013) Portal and sinusoidal fibrosis are common on liver biopsy after Fontan surgery. Pediatr Cardiol 34:135–142
Evans WN, Winn BJ, Yumiaco NS, Galindo A, Rothman A, Acherman RJ, Restrepo H (2014) Transvenous hepatic biopsy in stable Fontan patients undergoing cardiac catheterization. Pediatr Cardiol 35:1273–1278
Poterucha JT, Johnson JN, Qureshi MY et al (2015) Magnetic resonance elastography: a novel technique for the detection of hepatic fibrosis and hepatocellular carcinoma after the Fontan operation. Mayo Clin Proc 90:882–894
Evans WN, Acherman RJ, Reardon LC, Galindo A, Rothman A, Ciccolo ML, Carrillo SA, Winn BJ, Yumiaco NS, Restrepo H (2016) An observation from liver biopsies two decades post-Fontan. Pediatr Cardiol 37:1119–1122
Evans WN, Acherman RJ, Ciccolo ML, Carrillo SA, Galindo A, Rothman A, Mayman GA, Adams EA, Reardon LC, Winn BJ, Yumiaco NS, Shimuizu L, Inanaga Y, Deleon RJ, Restrepo H (2018) A composite noninvasive index correlates with liver fibrosis scores in post-Fontan patients: preliminary findings. Congenit Heart Dis 13:38–45
Fidai A, Dallaire F, Alvarez N et al (2016) Risk factors and serological markers of liver cirrhosis after Fontan procedure. Heart Vessels 31:1514–1521
Goldberg DJ, Surrey LF, Glatz AC, Dodds K, O’Byrne ML, Lin HC, Fogel M, Rome JJ, Rand EB, Russo P, Rychik J (2017) Hepatic fibrosis sis universal following Fontan operation, and severity is associated with time from surgery: a liver biopsy and hemodynamic study. J Am Heart Assoc 6(5):e004809. https://doi.org/10.1161/JAHA.116.004809
de Leval MR, Kilner P, Gewillig M, Bull C (1988) Total cavopulmonary connection: a logical alternative to atriopulmonary connection for complex Fontan operations. Experimental studies and early clinical experience. J Thorac Cardiovasc Surg 96:682–695
Laschinger JC, Ringel RE, Brenner JI, McLaughlin JS (1992) Extracardiac total cavopulmonary connection. Ann Thorac Surg 54:371–373
Giannico S, Corno A, Marino B, Cicini MP, Gagliardi MG, Amodeo A, Picardo S, Marcelletti C (1992) Total extracardiac right heart bypass. Circulation 86(5 Suppl):II110–II117
Lardo AC, Webber SA, Friehs I, del Nido PJ, Cape EG (1999) Fluid dynamic comparison of intra-atrial and extracardiac total cavopulmonary connections. J Thorac Cardiovasc Surg 117:697–704
Hsia TY, Migliavacca F, Pittaccio S, Radaelli A, Dubini G, Pennati G, de Leval M (2004) Computational fluid dynamic study of flow optimization in realistic models of the total cavopulmonary connections. J Surg Res 116:305–313
Masters JC, Ketner M, Bleiweis MS, Mill M, Yoganathan A, Lucas CL (2004) The effect of incorporating vessel compliance in a computational model of blood flow in a total cavopulmonary connection (TCPC) with caval centerline offset. J Biomech Eng 126:709–713
Haggerty CM, Restrepo M, Tang E, de Zélicourt DA, Sundareswaran KS, Mirabella L, Bethel J, Whitehead KK, Fogel MA, Yoganathan AP (2014) Fontan hemodynamics from 100 patient-specific cardiac magnetic resonance studies: a computational fluid dynamics analysis. J Thorac Cardiovasc Surg 148:1481–1489
Bossers SS, Helbing WA, Duppen N, Kuipers IM, Schokking M, HazekampBogersTenHarkelTakken MGAJADT (2014) Exercise capacity in children after total cavopulmonary connection: lateral tunnel versus extracardiac conduit technique. J Thorac Cardiovasc Surg 148:1490–1497
Talwar S, Kumar MV, Sreenivas V, Gupta VP, Choudhary SK, Airan B (2018) Exercise performance after univentricular palliation. Ann Pediatr Cardiol 11:40–47
Bossers SS, Duppen N, Kapusta L, Maan AC, Duim AR, Bogers AJ, Hazekamp MG, van Iperen G, Helbing WA, Blom NA (2015) Comprehensive rhythm evaluation in a large contemporary Fontan population. Eur J Cardiothorac Surg 48(6):833–841
Januszewska K, Schuh A, Lehner A, Dalla-Pozza R, Malec E (2017) Lateral atrial tunnel Fontan operation predisposes to the junctional rhythm. Pediatr Cardiol 38:712–718
Zheng J, Li Z, Li Q, Li X (2018) Meta-analysis of Fontan procedure: Extracardiac conduit vs. intracardiac lateral tunnel. Herz 43:238–245
van den Bosch E, Bossers SSM, Bogers AJJC, Robbers-Visser D, van Dijk APJ, Roos-Hesselink JW, Breur HMPJ, Haas F, Kapusta L, Helbing WA (2019) Staged total cavopulmonary connection: serial comparison of intra-atrial lateral tunnel and extracardiac conduit taking account of current surgical adaptations. Interact Cardiovasc Thorac Surg 29:453–460
Rijnberg FM, Hazekamp MG, Wentzel JJ, de Koning PJH, Westenberg JJM, Jongbloed RM, Blom NA, Roest AAW (2018) Energetics of blood flow in cardiovascular disease: concept and clinical implications of adverse energetics in patients with a Fontan circulation. Circulation 137:2393–2407
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by WNE, RA, and HR. The first draft of the manuscript was written by WNE and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The author(s) declared no conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee from Sunrise Health Institutional Review Board, approval number 19-025, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Evans, W.N., Acherman, R.J., Mayman, G.A. et al. The Rate of Hepatic Fibrosis Progression in Patients Post-Fontan. Pediatr Cardiol 41, 905–909 (2020). https://doi.org/10.1007/s00246-020-02331-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-020-02331-0