Abstract
Background
Nerve injuries are a common occurrence among hand injuries, which at the time of the COVID-19 emergency, did not appear to have reduced their incidence. The treatment of these injuries is urgent, but the pandemic has led to a reduction in the availability of resources and a consequent reorganization of activities. Principles about Wide-Awake Local Anesthesia No Tourniquet (WALANT) in hand surgery expressed by LaLonde helped hand surgeons to adapt to this new condition by demonstrating a possible outpatient pathway for the treatment of hand traumatic conditions. In the present study, we bring our experience in nerve repair at time of COVID-19 emergency.
Methods
We retrospectively enrolled in this study all patients surgically treated for a peripheral nerve injury (PNI) during the COVID-19 emergency period from March 2020 to March 2022. Demographical, anamnestic, surgical, and postoperative data were recorded and analyzed. Persisting Tinel was set as the primary outcome, while hypoesthesia and other complications as secondary outcomes.
Results
Thirty-six patients have been enrolled. Despite some difference in group homogeneity in term of hypertension and multi-digital involvement, we registered no difference in term of outcomes (P > 0.05) between patient operated in surgical theater and in outpatient clinic and between the various techniques of nerve repair employed (P > 0.05).
Conclusions
Nerve repair on an outpatient facility is technically feasible and was found in this study to be safe and effective. Compared to hospitalization, the outpatient setting has a more “agile” organization and lower costs, making it preferable in selected cases.
Level of evidence: Level IV, Therapeutic.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
COVID-19 emergency has been a worldwide threatening condition who changed our life and habit. The impact of COVID-19 emergency in society and hospital organization is well known, consisting in the “re-”introduction of the concept of quarantine and the reorganization of activities with the suspension of all deferrable procedures [1]. At the peak of the pandemic, this even meant the suspension of all procedures related to the treatment of non-life-threatening conditions. In Italy, this phenomenon occurred especially in the most affected areas such as northern regions (e.g., Lombardy) [2, 3]. In this period, hand injuries and therefore conditions that require urgent treatment, such as peripheral nerve injuries (PNI) [4], did not seem to have reduced their incidence [5]. While the redirection of resources and activities towards the treatment of patients affected by SARS CoV-2 (severe acute respiratory syndrome) has led to a reduction in both economic and human resources dedicated to hand surgery, the need for the treatment of urgent injuries has remained. In Italy, this has led hand surgery units to reorganize their activities [2]. The principles associated with Wide-Awake Local Anesthesia No Tourniquet (WALANT) in hand surgery popularized by Don LaLonde [6] helped hand surgeons to cope with this new situation, opening the way to the outpatient pathway for the treatment of minor traumatic hand conditions. In the present study, we bring our experience in nerve repair at time of COVID-19 emergency and the consequent reorganization of the care pathway, with the aim to evaluate the safety and effectiveness of the outpatient treatment pathway compared to ordinary hospitalization and day surgery. The secondary purpose was to assess which nerve repair technique was the most beneficial.
Materials and methods
A retrospective review of all patients undergoing surgery during the emergency period of the COVID-19 pandemic (March 2020–March 2022) at “ASST-Settlaghi Circolo e Fondazione Macchi” hospital was performed. Patients with hand PNI who received surgical treatment were selected. The inclusion criteria were as follows: trauma to the hand involving a sensitive peripheral nerve such as common digital nerves, laterodigital nerves, and the superficial branch of the radial nerve. Patients with main nerve injury, such as median and ulnar nerves in the wrist or forearm, and complex or major hand trauma (including amputations) and patients who were clinically unstable at the time of injury were excluded from the study.
Demographic, anamnestic, and surgical data were recorded, such as the surgical course and neurorrhaphy technique, as well as outcomes and postoperative complications. For the analysis, patients were grouped according to the surgical pathway between those operated in outpatient clinical setting and those operated in a surgical theater.
The outpatient clinical setting included a surgical room in which usually small surgery is performed such as small skin or subcutaneous tumor excision. In this setting, sterile draping is limited to the area involved by the lesion. An 8/0 polyamide monofilament suture wire was used for the nerve repair. The surgery was performed under WALANT by two surgeons (one hand surgery–experienced specialist and a resident) under × 3.5 magnification loupes with external help of a nurse. The nerve was then directly repaired and occasionally wrapped with an external sheath of vein conduit or with fibrin glue.
Patients undergoing surgery in the operating room were treated under axillary plexus anesthesia with a tourniquet. Patient were then admitted in ward for postoperative observation. Patients undergoing the outpatient pathway were instead discharged immediately from the hospital after operation was concluded. The surgical technique, instruments, and optical magnification used were the same in both types of pathway.
Oral antibiotic therapy with amoxicillin and clavulanic acid was administered from the time of injury until 5 days postoperatively in all patients, in line with the hospital protocol for penetrating trauma injuries. Also, patients were divided into three groups according to the surgical technique used for nerve repair: direct nerve suture (DNS), direct nerve suture reinforced by a sleeve of fibrin glue (FGS), direct nerve suture with vein wrapping (VW).
Presence of the Tinel sign at 3–6 months at the site of the trauma, indicating a development of neuroma, was set as the primary outcome. Residual hypoesthesia and postoperative complications such as infection, wound dehiscence, and stiffness were considered as secondary outcomes. Hypoesthesia was defined by a static 2-point discrimination test on the fingertips above 8 mm.
Statistical analysis was performed with SPSS® Statistics version 23.0 (IBM SPSS Statistics for Windows; IBM Corp., Armonk, NY, USA) and parametric and non-parametric test such as the chi-square, Fisher, and Mann–Whitney tests with a confidence interval set at 95% (significative P value < 0.05). The study was conducted in accordance with the Declaration of Helsinki, with patients’ consensus obtained during the follow-up.
Results
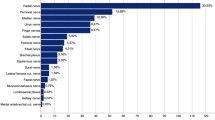
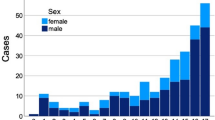
During the considered period, a total of 36 patients have been retrospectively identified and enrolled in the present study. The demographic, anamnestic, and operative characteristics of the population are described in Table 1.
According to surgical pathway, the patients were divided into two groups; among them, 18 underwent surgery in an operative theater (regular hospitalization or day surgery), and the others underwent surgery on an outpatient facility. In Table 2 are compared the characteristics and the outcomes of the two groups. Both groups appear to be uniform, except for hypertension (6 vs 1, P = 0.035) and multi-digital trauma (more than one finger involved) (9 vs 2, P = 0.011), which were statistically different. No statistically significant difference was found between the two groups in terms of outcome (P > 0.05). Among the general complications (8 patients), there were no cases of infection; stiffness was the only complication recorded, with the exception of one case treated on an outpatient basis that developed a retractile scar.
Moreover, to evaluate the difference between the surgical technique used for nerve repair, patients were sorted in three groups: DNS (18), FGS (7), VW (11). The groups were similar except for the timing of trauma repair that was delayed in patients in which a vein wrapping was performed (1.72 vs 2.29 vs 5.91, P = 0.008). Once again, no difference was found between the outcomes considered (P > 0.05) (Table 3).
In our study, the time between trauma and repair (Δ-tTR) was found not to be associated to higher complications (P = 0.125), hypoesthesia (P = 0.655), and development of Tinel (P = 0.196).
Discussion
COVID-19 emergency has been a worldwide catastrophe in terms of economy and lives. In Italy, in order to face the overwhelming amount of patients with COVID-19 infection, hospitals underwent to a structural reorganization. This included a conversion of all the surgical wards to internal medicine wards, a switch of all the activities of healthcare providers (medical, doctors, and nurses) to the treatment of SARS Cov-2 patients with reduction of resources for directing the treatment of other pathologies [3]. From the surgeon’s point of view, the consequence of this reorganization was a drastic reduction in the availability of operating theaters. On the other side, hand injuries did not decrease, nor did the number of patients with traumas requiring urgent surgical treatment [5] such as those with nerve injury.
As promoted by LaLonde and Phillips [6], the surgical treatment of small trauma of the hand can be safely accomplished in a “minor procedure room” without the necessity of a recovery room. This is feasible thanks to the WALANT anesthetic technique, which implies the use of a sort of tumescent technique around and in the site of the operative area with diluted adrenaline and anesthetic solution. The double benefits intrinsic of WALANT are the possibility of covering a large area (i.e., all the hand) and the effective control of bleeding [7].
In our center, the transition to outpatient management of certain types of hand injuries arose from the need to treat patients with non-deferrable conditions at a time when there was no availability of surgical rooms due to the COVID-19 pandemic emergency. In this context, all peripheral hand injuries that did not require a specific instrument (e.g., an optical microscope) were referred to outpatient management. For patients’ safety, the decision to submit them to the outpatient route was subject to their surgical risk, assessed on the basis of comorbidity (ASA score higher than 3), and COVID-19 positivity of the nasopharyngeal swab. In those cases, patients were referred directly to ordinary hospitalization, which only happened in one case.
The primary objective of our study was to evaluate the safety and efficacy of outpatient setting treatment in PNI of the hand. By comparing the two groups of patients (those operated in outpatient context vs those hospitalized) we found that there was no difference in terms of developing complication such as neuroma or infection, with the same efficacy of treatment. Our results regarding infection rate seems to be in line with those reported in literature [8, 9].
Although no cost-analysis was carried out in this study, another consideration is about the cost economic impact of the two pathways. For the same treatment efficacy and safety, outpatient management avoids and significantly reduces the costs associated with patients’ admission to the hospital, the amount of staff involved, and the occupation time of the operating theater. Therefore, for selected patients, we believe that for minor hand traumas, the outpatient setting should be preferable.
Secondly, the surgical technique used for nerve repair was analyzed. No significant difference in outcomes was found between epineural nerve suture, venous bandage, and epineural suture with fibrin glue sheath. The use of fibrin glue to reinforce nerve sutures may be not worth cost-effective. Vein wrapping serves the purpose of isolating and reinforcing the neurorrhaphy, but implies the harvest of a donor vein and increases the operative time. Although the groups in our cases differed in terms of delay in trauma treatment, we found no benefit in using venous or “glue” sleeves. This evidence, in accordance with the literature [10], suggests that classical neurorrhaphy seems to be the simplest and most convenient technique in cases of nerve injuries without significant gaps. Our results may have been influenced by a different timing in the treatment, thereby disadvantaging the VW group that was treated with a higher delay.
In the present study, oral antibiotic therapy has been administered to all patients for two reasons. Although our hospital is a trauma center, minor injuries of the hand are not always immediately evaluated by the hand surgeon, and the surgical assessment and thus accurate wound irrigation may be delayed. Secondly, in our area, these are often work-related injuries, occurring in manual workers in dirty conditions with tools such as saws, or alternatively from animal bites. While literature suggest that antibiotic therapy is not required in small hand trauma [11], this is not for this kind of wounds. For these reasons, in order to prevent the development of infections, in our institute, we prefer to administer a course of antibiotic therapy to all patients with penetrating hand trauma regardless of the surgical pathway.
The limitations of this study are as follows: the retrospective design, the low number of patients enrolled, and the difference in homogeneity found between the groups. Patients included are relatively few, since we wanted to analyze a very specific pattern of lesion such as PNI of the hand within a peculiar time frame. When comparing the surgical pathways (Table 1), a difference in both groups regarding the hypertension prevalence and multi-digital trauma (P < 0.05) was found. Hypertension was more prevalent in the hospitalized group. This could be a selection bias between the two groups, given that patients were admitted because they were more “fragile.” However, other comorbidities such as diabetes and the ASA score were comparable in both groups, refuting this hypothesis. Another objection could be the possible influence of hypertension in outcomes. Hypertension can contribute to neuropathy in diabetic patients [12, 13]; however, in literature, the association between hypertension and impairment of nerve recover after repair is not described. In our study, only one patient had a history of a combination of diabetes and hypertension, but did not develop any complications, Tinel or hypoesthesia. In this paper, multi-digital trauma was a selection bias, yet the outcomes were comparable. Involving more than one finger may increase the operating time, and this must be weighted with patient compliance when deciding whether an outpatient procedure is feasible. Further studies are needed to prevent the effect of biases encountered in this study regarding the homogeneity of the population, and to gain a better evaluation on the safety and efficacy of the outpatient surgical pathway.
Conclusions
Nerve repair on an outpatient setting is technically feasible and was found in this study to be safe and effective, with good functional results and complication incidence. This can be achieved by reproducing a sterile surgical field and taking care to maintain antisepsis during the procedure. Compared to hospitalization, the outpatient setting has a more “agile” organization and lower costs, making it preferable in selected cases. Patient safety is paramount and the selection must be weighed against operational risk and patient compliance.
Data Availability
The data used for this study are collected in a non-publicly accessible, password-protected excell database.
References
De Filippis G, Cavazzana L, Gimigliano A et al (2020) Covid-19 pandemic: a frontline hospital reorganization to cope with therapeutic and diagnostic emergency. Pharmacol Res 161:105160. https://doi.org/10.1016/J.PHRS.2020.105160
Toia F, Romeo M, Abate M et al (2021) Impact of COVID-19 on hand surgery in Italy: a comparison between the Northern and the Southern regions. Hand Surg Rehabil 40:139–144. https://doi.org/10.1016/J.HANSUR.2020.11.005
Cherubino M, Valdatta L (2020) Plastic surgery in coronavirus disease 2019 emergencies: report from Northern Italy. Plast Reconstr Surg - Glob Open. 13;8(5):e2913. https://doi.org/10.1097/GOX.0000000000002913
Campbell WW (2008) Evaluation and management of peripheral nerve injury. Clin Neurophysiol 119:1951–1965. https://doi.org/10.1016/J.CLINPH.2008.03.018
Saleh S, Faulkner H, Golledge K et al (2023) The impact of COVID-19 on hand trauma. Hand (N Y) 18:355. https://doi.org/10.1177/15589447211028918
Lalonde D (ed) (2015) Wide awake hand surgery, 1st edn. CRC Press
Prasetyono TOH, Biben JA (2014) One-per-mil tumescent technique for upper extremity surgeries: broadening the indication. J Hand Surg Am 39:3-12.e7. https://doi.org/10.1016/J.JHSA.2013.09.034
Oakes TC, Wong KC, Schank KJ et al (2022) Infection rate comparison during transition from hospital to office WALANT enabled by virtual reality. Plast Reconstr Surg - Glob Open 10:e4285. https://doi.org/10.1097/GOX.0000000000004285
Avoricani A, Dar QA, Levy KH et al (2022) WALANT hand and upper extremity procedures performed with minor field sterility are associated with low infection rates. Plast Surg 30:122–129. https://doi.org/10.1177/22925503211003840/ASSET/IMAGES/LARGE/10.1177_22925503211003840-FIG2.JPEG
Paprottka FJ, Wolf P, Harder Y et al (2013) Sensory recovery outcome after digital nerve repair in relation to different reconstructive techniques: meta-analysis and systematic review. Plast Surg Int 2013:1–17. https://doi.org/10.1155/2013/704589
Murphy GRF, Gardiner MD, Glass GE et al (2016) Meta-analysis of antibiotics for simple hand injuries requiring surgery. Br J Surg 103:487–492. https://doi.org/10.1002/BJS.10111
Ponirakis G, Petropoulos IN, Alam U et al (2019) Hypertension contributes to neuropathy in patients with type 1 diabetes. Am J Hypertens 32:796–803. https://doi.org/10.1093/AJH/HPZ058
Gregory JA, Jolivalt CG, Goor J et al (2012) Hypertension-induced peripheral neuropathy and the combined effects of hypertension and diabetes on nerve structure and function in rats. Acta Neuropathol 124:561–573. https://doi.org/10.1007/S00401-012-1012-6/FIGURES/6
Acknowledgements
The authors would like to give special thanks to Dr. Francesco Maria Locatelli, Dr. Danilo Di Giovanna, Dr. Ferruccio Paganini, Dr. Annachiara Tellarini, Dr. Veronica Fasoli, Dr. Francesco Buttarelli, Dr. Beatrice Corsini, Dr. Sara Matarazzo, Dr. Julien Teodori, Dr. Anna Brandolini, and Dr. Emanuele Mascherpa for their contribution and support in daily activities.
Funding
Open access funding provided by Università degli Studi dell'Insubria within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Dr. Andrea Minini, Dr. Tommaso Baroni, and Dr. Elisa Bascialla. The first draft of the manuscript was written by Dr. Leonardo Garutti and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This is an observational study; no ethical approval is required. This was confirmed by the local Ethical Committee of the hospital.
Patient consent
The study was conducted with the consent obtained from the patients during the follow-up visit.
Competing interests
Leonardo Garutti, Federico Tamborini, Alessandro Fagetti, Tommaso Baroni, Elisa Bascialla, Andrea Minini, Mario Cherubino, and Luigi Valdatta declare no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Garutti, L., Tamborini, F., Fagetti, A. et al. Sensitive peripheral nerve repair during COVID-19 emergency: does the outpatient surgical setting work as well as the operating theater?. Eur J Plast Surg 46, 1193–1197 (2023). https://doi.org/10.1007/s00238-023-02085-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-023-02085-x