Abstract
Purpose
To compare image quality and interobserver agreement in evaluations of neuroforaminal stenosis between 1.5T cervical spine magnetic resonance imaging (MRI) with deep learning reconstruction (DLR) and 3T MRI without DLR.
Methods
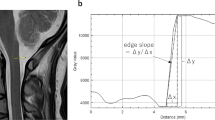
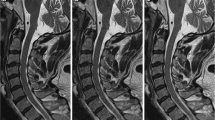
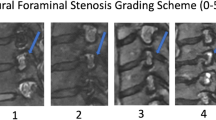
In this prospective study, 21 volunteers (mean age: 42.4 ± 11.9 years; 17 males) underwent cervical spine T2-weighted sagittal 1.5T and 3T MRI on the same day. The 1.5T and 3T MRI data were used to reconstruct images with (1.5T-DLR) and without (3T-nonDLR) DLR, respectively. Regions of interest were marked on the spinal cord to calculate non-uniformity (NU; standard deviation/signal intensity × 100), as an indicator of image noise. Two blinded radiologists evaluated the images in terms of the depiction of structures, artifacts, noise, overall image quality, and neuroforaminal stenosis. The NU value and the subjective image quality scores were compared between 1.5T-DLR and 3T-nonDLR using the Wilcoxon signed-rank test. Interobserver agreement in evaluations of neuroforaminal stenosis for 1.5T-DLR and 3T-nonDLR was evaluated using Cohen’s weighted kappa analysis.
Results
The NU value for 1.5T-DLR was 8.4, which was significantly better than that for 3T-nonDLR (10.3; p < 0.001). Subjective image scores were significantly better for 1.5T-DLR than 3T-nonDLR images (p < 0.037). Interobserver agreement (95% confidence intervals) in the evaluations of neuroforaminal stenosis was significantly superior for 1.5T-DLR (0.920 [0.916–0.924]) than 3T-nonDLR (0.894 [0.889–0.898]).
Conclusion
By using DLR, image quality and interobserver agreement in evaluations of neuroforaminal stenosis on 1.5T cervical spine MRI could be improved compared to 3T MRI without DLR.



Similar content being viewed by others
References
Brinjikji W, Luetmer PH, Comstock B et al (2015) Systematic literature review of imaging features of spinal degeneration in asymptomatic populations. AJNR Am J Neuroradiol 36(4):811–816
Theodore N (2020) Degenerative cervical spondylosis. N Engl J Med 383(2):159–168
Radhakrishnan K, Litchy WJ, O’Fallon WM, Kurland LT (1994) Epidemiology of cervical radiculopathy. A population-based study from Rochester, Minnesota, 1976 through 1990. Brain 117(Pt 2):325–335
Voorhies RM (2001) Cervical spondylosis: recognition, differential diagnosis, and management. Ochsner J 3(2):78–84
Korzan JR, Gorassini M, Emery D, Taher ZA, Beaulieu C (2002) In vivo magnetic resonance imaging of the human cervical spinal cord at 3 Tesla. J Magn Reson Imaging 16(1):21–27
Takahashi M, Uematsu H, Hatabu H (2003) MR imaging at high magnetic fields. Eur J Radiol 46(1):45–52
Grams AE, Gempt J, Forschler A (2010) Comparison of spinal anatomy between 3-Tesla MRI and CT-myelography under healthy and pathological conditions. Surg Radiol Anat 32(6):581–585
Meacock J, Schramm M, Selvanathan S et al (2021) Systematic review of radiological cervical foraminal grading systems. Neuroradiology 63(3):305–316
Park HJ, Kim SS, Lee SY et al (2013) A practical MRI grading system for cervical foraminal stenosis based on oblique sagittal images. Br J Radiol 86(1025):20120515
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521(7553):436–444
Yasaka K, Abe O (2018) Deep learning and artificial intelligence in radiology: Current applications and future directions. PLoS Med 15(11):e1002707
Chartrand G, Cheng PM, Vorontsov E et al (2017) Deep learning: a primer for radiologists. Radiographics 37(7):2113–2131
Yasaka K, Akai H, Kunimatsu A, Kiryu S, Abe O (2018) Deep learning with convolutional neural network in radiology. Jpn J Radiol 36(4):257–272
Lakhani P, Sundaram B (2017) Deep learning at chest radiography: automated classification of pulmonary tuberculosis by using convolutional neural networks. Radiology 284(2):574–582
Yasaka K, Akai H, Abe O, Kiryu S (2018) Deep learning with convolutional neural network for differentiation of liver masses at dynamic contrast-enhanced CT: a preliminary study. Radiology 286(3):887–896
Kiryu S, Yasaka K, Akai H et al (2019) Deep learning to differentiate parkinsonian disorders separately using single midsagittal MR imaging: a proof of concept study. Eur Radiol 29(12):6891–6899
Yasaka K, Akai H, Kunimatsu A, Abe O, Kiryu S (2018) Liver fibrosis: deep convolutional neural network for staging by using gadoxetic acid-enhanced hepatobiliary phase MR images. Radiology 287(1):146–155
Yasaka K, Akai H, Kunimatsu A, Abe O, Kiryu S (2018) Deep learning for staging liver fibrosis on CT: a pilot study. Eur Radiol 28(11):4578–4585
Higaki T, Nakamura Y, Tatsugami F, Nakaura T, Awai K (2019) Improvement of image quality at CT and MRI using deep learning. Jpn J Radiol 37(1):73–80
Kidoh M, Shinoda K, Kitajima M et al (2020) Deep learning based noise reduction for brain MR imaging: tests on phantoms and healthy volunteers. Magn Reson Med Sci 19(3):195–206
Tajima T, Akai H, Sugawara H et al (2021) Breath-hold 3D magnetic resonance cholangiopancreatography at 1.5 T using a deep learning-based noise-reduction approach: Comparison with the conventional respiratory-triggered technique. Eur J Radiol 144:109994
Yasaka K, Akai H, Sugawara H et al (2021) Impact of deep learning reconstruction on intracranial 1.5 T magnetic resonance angiography. Jpn J Radiol 40(5):476–483
Kashiwagi N, Tanaka H, Yamashita Y et al (2021) Applicability of deep learning-based reconstruction trained by brain and knee 3T MRI to lumbar 1.5T MRI. Acta Radiol Open 10(6):20584601211023939
Ueda T, Ohno Y, Yamamoto K et al (2021) Compressed sensing and deep learning reconstruction for women’s pelvic MRI denoising: utility for improving image quality and examination time in routine clinical practice. Eur J Radiol 134:109430
Fruehwald-Pallamar J, Szomolanyi P, Fakhrai N et al (2012) Parallel imaging of the cervical spine at 3T: optimized trade-off between speed and image quality. AJNR Am J Neuroradiol 33(10):1867–1874
Noebauer-Huhmann IM, Glaser C, Dietrich O et al (2007) MR imaging of the cervical spine: assessment of image quality with parallel imaging compared to non-accelerated MR measurements. Eur Radiol 17(5):1147–1155
Engel G, Bender YY, Adams LC et al (2019) Evaluation of osseous cervical foraminal stenosis in spinal radiculopathy using susceptibility-weighted magnetic resonance imaging. Eur Radiol 29(4):1855–1862
Cohen J (1968) Weighted kappa: nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull 70(4):213–220
Yasaka K, Tanishima T, Ohtake Y et al (2022) Deep learning reconstruction for 1.5 T cervical spine MRI: effect on interobserver agreement in the evaluation of degenerative changes. Eur Radiol. https://doi.org/10.1007/s00330-022-08729-z
Shim E, Lee JW, Lee E et al (2019) Cervical spondylotic myelopathy: diagnostic performance of radiologists with varying levels of experience in comparing MR images acquired using field strengths of 1.5 and 3 Tesla. Acta Radiol 60(10):1314–1320
Funding
This study was financially supported by Canon Medical Systems Corporation. Any data and information included in this study was not controlled by Canon Medical Systems Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares a conflict of interest: Shigeru Kiryu got research grants from Canon Medical Systems Corporation.
Ethical approval
This prospective study was approved by our institutional review board (20-Nr-059).
Informed consent
Written informed consent was obtained from all study participants.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 12 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yasaka, K., Tanishima, T., Ohtake, Y. et al. Deep learning reconstruction for the evaluation of neuroforaminal stenosis using 1.5T cervical spine MRI: comparison with 3T MRI without deep learning reconstruction. Neuroradiology 64, 2077–2083 (2022). https://doi.org/10.1007/s00234-022-03024-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-03024-6