Abstract
Purpose
To investigate the pharmacokinetic changes of linezolid in patients with hepatic impairment and to explore a method to predict linezolid exposure.
Methods
Patients with hepatic impairment who received linezolid were recruited. A population pharmacokinetic model (PPK) was then built using NONMEM software. And based on the final model, virtual patients with rich concentration values was constructed through Monte Carlo simulations (MCS), which were used to build machine learning (ML) models to predict linezolid exposure levels. Finally, we investigated the risk factors for thrombocytopenia in patients included.
Results
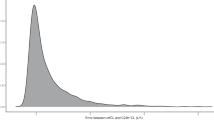
A PPK model with population typical values of 3.83 L/h and 34.1 L for clearance and volume of distribution was established, and the severe hepatic impairment was identified as a significant covariate of clearance. Then, we built a series of ML models to predict the area under 0 -24 h concentration-time curve (AUC0-24) of linezolid based on virtual patients from MCS. The results showed that the Xgboost models showed the best predictive performance and were superior to the methods for estimating linezolid AUC0-24 based on though concentration or daily dose. Finally, we found that baseline platelet count, linezolid AUC0-24, and combination with fluoroquinolones were independent risk factors for thrombocytopenia, and based on this, we proposed a method for calculating the toxicity threshold of linezolid.
Conclusion
In this study, we successfully constructed a PPK model for patients with hepatic impairment and used ML algorithm to estimate linezolid AUC0-24 based on limited data. Finally, we provided a method to determine the toxicity threshold of linezolid.




Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
References
Livermore DM (2003) Linezolid in vitro: mechanism and antibacterial spectrum. J Antimicrob Chemother 51(Suppl 2):ii9-16. https://doi.org/10.1093/jac/dkg249
Clemett D, Markham A (2000) Linezolid. Drugs 59(4):815–827; discussion 828. https://doi.org/10.2165/00003495-200059040-00007
Moellering RC (2003) Linezolid: the first oxazolidinone antimicrobial. Ann Intern Med 138(2):135–142. https://doi.org/10.7326/0003-4819-138-2-200301210-00015
Yang L, Wu T, Li J, Li J (2018) Bacterial infections in acute-on-chronic liver failure. Semin Liver Dis 38(2):121–133. https://doi.org/10.1055/s-0038-1657751
Wynalda MA, Hauer MJ, Wienkers LC (2000) Oxidation of the novel oxazolidinone antibiotic linezolid in human liver microsomes. Drug Metab Dispos 28(9):1014–1017
Luque S, Muñoz-Bermudez R, Echeverría-Esnal D, Sorli L, Campillo N, Martínez-Casanova J, González-Colominas E, Álvarez-Lerma F, Horcajada JP, Grau S, Roberts JA (2019) Linezolid dosing in patients with liver cirrhosis: standard dosing risk toxicity. Ther Drug Monit 41(6):732–739. https://doi.org/10.1097/ftd.0000000000000665
Liao R, Dong Y, Chen L, Wang T, Li H, Dong H (2023) A standard dose of linezolid puts patients with hepatic impairment at risk of overexposure. Eur J Clin Pharmacol 79(1):149–157. https://doi.org/10.1007/s00228-022-03427-7
Sasaki T, Takane H, Ogawa K, Isagawa S, Hirota T, Higuchi S, Horii T, Otsubo K, Ieiri I (2011) Population pharmacokinetic and pharmacodynamic analysis of linezolid and a hematologic side effect, thrombocytopenia. Japanese patients Antimicrob Agents Chemother 55(5):1867–1873. https://doi.org/10.1128/aac.01185-10
Rayner CR, Forrest A, Meagher AK, Birmingham MC, Schentag JJ (2003) Clinical pharmacodynamics of linezolid in seriously ill patients treated in a compassionate use programme. Clin Pharmacokinet 42(15):1411–1423. https://doi.org/10.2165/00003088-200342150-00007
Pea F, Furlanut M, Cojutti P, Cristini F, Zamparini E, Franceschi L, Viale P (2010) Therapeutic drug monitoring of linezolid: a retrospective monocentric analysis. Antimicrob Agents Chemother 54(11):4605–4610. https://doi.org/10.1128/aac.00177-10
Töpper C, Steinbach CL, Dorn C, Kratzer A, Wicha SG, Schleibinger M, Liebchen U, Kees F, Salzberger B, Kees MG (2016) Variable linezolid exposure in intensive care unit patients-possible role of drug-drug interactions. Ther Drug Monit 38(5):573–578. https://doi.org/10.1097/ftd.0000000000000324
Peck-Radosavljevic M (2017) Thrombocytopenia in chronic liver disease. Liver Int 37(6):778–793. https://doi.org/10.1111/liv.13317
Kawasaki T, Takeshita A, Souda K, Kobayashi Y, Kikuyama M, Suzuki F, Kageyama F, Sasada Y, Shimizu E, Murohisa G, Koide S, Yoshimi T, Nakamura H, Ohno R (1999) Serum thrombopoietin levels in patients with chronic hepatitis and liver cirrhosis. Am J Gastroenterol 94(7):1918–1922. https://doi.org/10.1111/j.1572-0241.1999.01231.x
Zhang YM, Yu W, Zhou N, Li JZ, Xu LC, Xie ZY, Lu YF, Li LJ (2015) High frequency of thrombocytopenia in patients with acute-on-chronic liver failure treated with linezolid. Hepatobiliary Pancreat Dis Int 14(3):287–292. https://doi.org/10.1016/s1499-3872(15)60379-4
Ikuta S, Tanimura K, Yasui C, Aihara T, Yoshie H, Iida H, Beppu N, Kurimoto A, Yanagi H, Mitsunobu M, Yamanaka N (2011) Chronic liver disease increases the risk of linezolid-related thrombocytopenia in methicillin-resistant Staphylococcus aureus-infected patients after digestive surgery. J Infect Chemother 17(3):388–391. https://doi.org/10.1007/s10156-010-0188-8
Dou L, Meng D, Dong Y, Chen L, Han X, Fan D, Dong H (2020) Dosage regimen and toxicity risk assessment of linezolid in sepsis patients. Int J Infect Dis 96:105–111. https://doi.org/10.1016/j.ijid.2020.03.054
Li SC, Ye Q, Xu H, Zhang L, Wang Y (2019) Population pharmacokinetics and dosing optimization of linezolid in pediatric patients. Antimicrob Agents Chemother. https://doi.org/10.1128/aac.02387-18
Wang X, Wang Y, Yao F, Chen S, Hou Y, Zheng Z, Luo J, Qiu B, Li Z, Wang Y, Wu Z, Lan J, Chen C (2021) Pharmacokinetics of linezolid dose adjustment for creatinine clearance in critically ill patients: a multicenter, prospective, open-label, observational study. Drug Des Devel Ther 15:2129–2141. https://doi.org/10.2147/dddt.S303497
Matsumoto K, Shigemi A, Takeshita A, Watanabe E, Yokoyama Y, Ikawa K, Morikawa N, Takeda Y (2014) Analysis of thrombocytopenic effects and population pharmacokinetics of linezolid: a dosage strategy according to the trough concentration target and renal function in adult patients. Int J Antimicrob Agents 44(3):242–247. https://doi.org/10.1016/j.ijantimicag.2014.05.010
Srinivas NR, Syed M (2016) Applicability of a single time point strategy for the prediction of area under the concentration curve of linezolid in patients: superiority of Ctrough- over Cmax-derived linear regression models. Drugs R D 16(1):69–79. https://doi.org/10.1007/s40268-015-0117-5
Ota R, Yamashita F (2022) Application of machine learning techniques to the analysis and prediction of drug pharmacokinetics. J Control Release 352:961–969. https://doi.org/10.1016/j.jconrel.2022.11.014
Poweleit EA, Vinks AA, Mizuno T (2023) Artificial intelligence and machine learning approaches to facilitate therapeutic drug management and model-informed precision dosing. Ther Drug Monit 45(2):143–150. https://doi.org/10.1097/ftd.0000000000001078
Gill J, Moullet M, Martinsson A, Miljković F, Williamson B, Arends RH, Pilla Reddy V (2022) Comparing the applications of machine learning, PBPK, and population pharmacokinetic models in pharmacokinetic drug-drug interaction prediction. CPT Pharmacometrics Syst Pharmacol 11(12):1560–1568. https://doi.org/10.1002/psp4.12870
Woillard JB, Labriffe M, Prémaud A, Marquet P (2021) Estimation of drug exposure by machine learning based on simulations from published pharmacokinetic models: the example of tacrolimus. Pharmacol Res 167:105578. https://doi.org/10.1016/j.phrs.2021.105578
Bououda M, Uster DW, Sidorov E, Labriffe M, Marquet P, Wicha SG, Woillard JB (2022) A machine learning approach to predict interdose vancomycin exposure. Pharm Res 39(4):721–731. https://doi.org/10.1007/s11095-022-03252-8
Kok B, Abraldes JG (2019) Child-Pugh classification: time to abandon? Semin Liver Dis 39(1):96–103. https://doi.org/10.1055/s-0038-1676805
Cockcroft DW, Gault MH (1976) Prediction of creatinine clearance from serum creatinine. Nephron 16(1):31–41. https://doi.org/10.1159/000180580
Dong H, Wang X, Dong Y, Lei J, Li H, You H, Wang M, Xing J, Sun J, Zhu H (2011) Clinical pharmacokinetic/pharmacodynamic profile of linezolid in severely ill intensive care unit patients. Int J Antimicrob Agents 38(4):296–300. https://doi.org/10.1016/j.ijantimicag.2011.05.007
Zhang SH, Zhu ZY, Chen Z, Li Y, Zou Y, Yan M, Xu Y, Wang F, Liu MZ, Zhang M, Zhang BK (2020) Population pharmacokinetics and dosage optimization of linezolid in patients with liver dysfunction. Antimicrob Agents Chemother. https://doi.org/10.1128/aac.00133-20
Tikiso T, Fuhrmann V, König C, Jarczak D, Iwersen-Bergmann S, Kluge S, Wicha SG, Grensemann J (2023) Acute-on-chronic liver failure alters linezolid pharmacokinetics in critically ill patients with continuous hemodialysis: an observational study. Ann Intensive Care 13(1):83. https://doi.org/10.1186/s13613-023-01184-z
Lin B, Hu Y, Xu P, Xu T, Chen C, He L, Zhou M, Chen Z, Zhang C, Yu X, Fang L, Zhu J, Ji Y, Lin Q, Cao H, Dai Y, Lu X, Shi C, Li L, Wang C, Li X, Fang Q, Miao J, Zhu Z, Lin G, Zhan H, Lv S, Zhu Y, Cai X, Ying Y, Chen M, Xu Q, Zhang Y, Xu Y, Federico P, Jiang S, Dai H (2022) Expert consensus statement on therapeutic drug monitoring and individualization of linezolid. Front Public Health 10:967311. https://doi.org/10.3389/fpubh.2022.967311
Murray M (2016) CYP2J2 - regulation, function and polymorphism. Drug Metab Rev 48(3):351–368. https://doi.org/10.1080/03602532.2016.1188938
Bièche I, Narjoz C, Asselah T, Vacher S, Marcellin P, Lidereau R, Beaune P, de Waziers I (2007) Reverse transcriptase-PCR quantification of mRNA levels from cytochrome (CYP)1, CYP2 and CYP3 families in 22 different human tissues. Pharmacogenet Genomics 17(9):731–742. https://doi.org/10.1097/FPC.0b013e32810f2e58
Davey PG (1988) Pharmacokinetics in liver disease. J Antimicrob Chemother 21(1):1–5. https://doi.org/10.1093/jac/21.1.1
Verbeeck RK (2008) Pharmacokinetics and dosage adjustment in patients with hepatic dysfunction. Eur J Clin Pharmacol 64(12):1147–1161. https://doi.org/10.1007/s00228-008-0553-z
MacGowan AP (2003) Pharmacokinetic and pharmacodynamic profile of linezolid in healthy volunteers and patients with Gram-positive infections. J Antimicrob Chemother 51(Suppl 2):ii17-25. https://doi.org/10.1093/jac/dkg248
Danishuddin KV, Faheem M, Woo Lee K (2022) A decade of machine learning-based predictive models for human pharmacokinetics: advances and challenges. Drug Discov Today 27(2):529–537. https://doi.org/10.1016/j.drudis.2021.09.013
Dong HY, Xie J, Chen LH, Wang TT, Zhao YR, Dong YL (2014) Therapeutic drug monitoring and receiver operating characteristic curve prediction may reduce the development of linezolid-associated thrombocytopenia in critically ill patients. Eur J Clin Microbiol Infect Dis 33(6):1029–1035. https://doi.org/10.1007/s10096-013-2041-3
Cheah CY, De Keulenaer B, Leahy MF (2009) Fluoroquinolone-induced immune thrombocytopenia: a report and review. Intern Med J 39(9):619–623. https://doi.org/10.1111/j.1445-5994.2009.01996.x
Acknowledgements
We would like to thank authors and all the participants for their time and effort.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82173898) and the Institutional foundation of the first affiliated hospital of Xi’an Jiaotong University (No. 2019ZYTS-01).
Author information
Authors and Affiliations
Contributions
RL: conception, design, data collection, analysis of data, interpretation of results, drafting, and revision of manuscript. HY: conception, design, and major revision of manuscript, and funding acquisition. YL: conception, design, major revision of manuscript. LH: data collection, and revision of manuscript. XL, HL and TT: interpretation of results, and revision of manuscript. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of the First Affiliated Hospital of Xi’an Jiaotong University (Xi’an, China). The institutional review board (IRB) approval number was “[XJTU1AF2019LSK-163].”
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liao, R., Chen, L., Cheng, X. et al. Estimation of linezolid exposure in patients with hepatic impairment using machine learning based on a population pharmacokinetic model. Eur J Clin Pharmacol (2024). https://doi.org/10.1007/s00228-024-03698-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00228-024-03698-2