Abstract
Purpose
Tacrolimus has a narrow therapeutic window. Measuring trough level (C0) as surrogate for drug exposure (AUC) in renal transplant recipients has limitations. Therefore, limited sampling strategies (LSS’s) have been developed. For the newer modified release, once-daily formulation (Tac QD) LSS’s are based on either linear regression analysis (LRA) or population pharmacokinetics with maximum a posteriori Bayesian (MAPB) estimation. The predictive performances of both methods were compared, also to LSS’s as described in literature.
Methods
LSS’s (maximally three sampling time points) were developed for Tac QD from full 24-h sampling by LRA in 27 Caucasian, stable renal transplant recipients. Performance for accuracy (mean absolute prediction error < 10%) and precision (root mean squared error < 15%) was quantified also after MAPB estimation in two independent groups (early and late post-transplant, n = 12 each).
Results
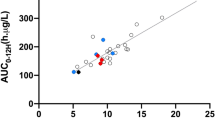
LRA determined a single 8 hours post-dose measurement (C8) to fulfil predefined criteria for accuracy (MAPE 3.41%) and precision (RMSE 4.28%). The best LSS contained C2, C8 and C12 for the stable (MAPE 2.42%, RMSE 3.1%) and the early post-transplant group (MAPE 2.46%, RMSE 3.14%). LRA did not include C0 for any LSS, unless it was forced into the model. MAPB estimation showed similar performance.
Conclusions
In renal transplant patients, sampling in the elimination phase (C8) accurately predicted Tac QD exposure, contrary to C0. The 3-point sampling C2, C8 and C12 had the best performance and is also valid early post-transplant. These LSS’s were similarly predictive with MAPB estimation. Dried blood spot could facilitate late sampling in clinical practice.


Similar content being viewed by others
References
Staatz CE, Tett SE (2015) Clinical pharmacokinetics of once-daily tacrolimus in solid-organ transplant patients. Clin Pharmacokinet 54(10):993–1025
Wallemacq P, Armstrong VW, Brunet M, Haufroid V, Holt DW, Johnston A, Kuypers D, le Meur Y, Marquet P, Oellerich M, Thervet E, Toenshoff B, Undre N, Weber LT, Westley IS, Mourad M (2009) Opportunities to optimize tacrolimus therapy in solid organ transplantation: report of the European consensus conference. Ther Drug Monit 31(2):139–152
Mahalati K, Kahan BD (2000) Pharmacological surrogates of allograft outcome. Ann Transplant 5(2):14–23
Undre NA, van Hooff J, Christiaans M, Vanrenterghem Y, Donck J, Heeman U, Kohnle M, Zanker B, Land W, Morales JM, Andrés A, Schäfer A, Stevenson P (1999) Low systemic exposure to tacrolimus correlates with acute rejection. Transplant Proc 31(1–2):296–298
Pisitkun T, Eiam-Ong S, Chusil S, Praditpornsilpa K, Pansin P, Tungsanga K (2002) The roles of C4 and AUC0-4 in monitoring of tacrolimus in stable kidney transplant patients. Transplant Proc 34(8):3173–3175
Stolk LM, Van Duijnhoven EM, Christiaans MH, van Hooff JP (2002) Trough levels of tacrolimus. Ther Drug Monit 24(4):573 author reply 573-4
Wong KM, Shek CC, Chau KF, Li CS (2000) Abbreviated tacrolimus area-under-the-curve monitoring for renal transplant recipients. Am J Kidney Dis 35(4):660–666
Op den Buijsch RA, van de Plas A, Stolk LM, Christiaans MH, van Hooff JP, Undre NA et al (2007) Evaluation of limited sampling strategies for tacrolimus. Eur J Clin Pharmacol 63(11):1039–1044
Alloway R, Steinberg S, Khalil K, Gourishankar S, Miller J, Norman D, Hariharan S, Pirsch J, Matas A, Zaltzman J, Wisemandle K, Fitzsimmons W, First MR (2005) Conversion of stable kidney transplant recipients from a twice daily Prograf-based regimen to a once daily modified release tacrolimus-based regimen. Transplant Proc 37(2):867–870
Advagraf: EPAR - Scientific Discussion: European Medicines Agency; 2007
Florman S, Alloway R, Kalayoglu M, Lake K, Bak T, Klein A, Klintmalm G, Busque S, Brandenhagen D, Lake J, Wisemandle K, Fitzsimmons W, First MR (2005) Conversion of stable liver transplant recipients from a twice-daily Prograf-based regimen to a once-daily modified release tacrolimus-based regimen. Transplant Proc 37(2):1211–1213
Marquet P, Bedu A, Monchaud C, Saint-Marcoux F, Rerolle JP, Etienne I et al (2018) Pharmacokinetic therapeutic drug monitoring of Advagraf in more than 500 adult renal transplant patients, using an expert system online. Ther Drug Monit 40(3):285–291
Benkali K, Rostaing L, Premaud A, Woillard JB, Saint-Marcoux F, Urien S et al (2010) Population pharmacokinetics and Bayesian estimation of tacrolimus exposure in renal transplant recipients on a new once-daily formulation. Clin Pharmacokinet 49(10):683–692
Saint-Marcoux F, Debord J, Undre N, Rousseau A, Marquet P (2010) Pharmacokinetic modeling and development of Bayesian estimators in kidney transplant patients receiving the tacrolimus once-daily formulation. Ther Drug Monit 32(2):129–135
Woillard JB, de Winter BC, Kamar N, Marquet P, Rostaing L, Rousseau A (2011) Population pharmacokinetic model and Bayesian estimator for two tacrolimus formulations--twice daily Prograf and once daily Advagraf. Br J Clin Pharmacol 71(3):391–402
Niioka T, Miura M, Kagaya H, Saito M, Numakura K, Habuchi T, Satoh S (2013) A limited sampling strategy to estimate the area under the concentration-time curve of tacrolimus modified-release once-daily preparation in renal transplant recipients. Ther Drug Monit 35(2):228–232
van Hooff JP, Alloway RR, Trunecka P, Mourad M (2011) Four-year experience with tacrolimus once-daily prolonged release in patients from phase II conversion and de novo kidney, liver, and heart studies. Clin Transpl 25(1):E1–E12
Stifft F, Undre N, van Hooff JP, Christiaans MH (2016) Effect of breakfast on the exposure of the once-daily Tacrolimus formulation in stable kidney transplant recipients. Ther Drug Monit 38(4):456–462
Van Hooff J, Van der Walt I, Kallmeyer J, Miller D, Dawood S, Moosa MR et al (2012) Pharmacokinetics in stable kidney transplant recipients after conversion from twice-daily to once-daily tacrolimus formulations. Ther Drug Monit 34(1):46–52
Wlodarczyk Z, Squifflet JP, Ostrowski M, Rigotti P, Stefoni S, Citterio F, Vanrenterghem Y, Krämer BK, Abramowicz D, Oppenheimer F, Pietruck F, Russ G, Karpf C, Undre N (2009) Pharmacokinetics for once- versus twice-daily tacrolimus formulations in de novo kidney transplantation: a randomized, open-label trial. Am J Transplant 9(11):2505–2513
Touw DJ, Vinks AA, Neef C (1997) Pharmacokinetic modelling of intravenous tobramycin in adolescent and adult patients with cystic fibrosis using the nonparametric expectation maximization (NPEM) algorithm. Pharm World Sci 19(3):142–151
Note for Guidance on the Investigation of Bioavailability and Bioequivalence (NfG on BA/ BE). London: European Medicines Agency; 2010
Fuchs A, Csajka C, Thoma Y, Buclin T, Widmer N (2013) Benchmarking therapeutic drug monitoring software: a review of available computer tools. Clin Pharmacokinet 52(1):9–22
Proost JH, Eleveld DJ (2006) Performance of an iterative two-stage bayesian technique for population pharmacokinetic analysis of rich data sets. Pharm Res 23(12):2748–2759
Xue L, Zhang H, Ma S, Rui JZ, Miao LY (2011) Population pharmacokinetics and pharmacogenetics of tacrolimus in healthy Chinese volunteers. Pharmacology. 88(5–6):288–294
D'Argenio DZ (1981) Optimal sampling times for pharmacokinetic experiments. J Pharmacokinet Biopharm 9(6):739–756
Sheiner LB, Beal SL (1981) Some suggestions for measuring predictive performance. J Pharmacokinet Biopharm 9(4):503–512
Bland JM, Altman DG (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1(8476):307–310
de Jonge H, Vanhove T, de Loor H, Verbeke K, Kuypers DR (2015) Progressive decline in tacrolimus clearance after renal transplantation is partially explained by decreasing CYP3A4 activity and increasing haematocrit. Br J Clin Pharmacol 80(3):548–559
Stifft F, van Kuijk SMJ, Bekers O, Christiaans MHL (2018) Increase in tacrolimus exposure after steroid tapering is influenced by CYP3A5 and pregnane X receptor genetic polymorphisms in renal transplant recipients. Nephrol Dial Transplant 33(9):1668–1675
Scholten EM, Cremers SC, Schoemaker RC, Rowshani AT, van Kan EJ, den Hartigh J, Paul LC, de Fijter JW (2005) AUC-guided dosing of tacrolimus prevents progressive systemic overexposure in renal transplant recipients. Kidney Int 67(6):2440–2447
Hoogtanders K, van der Heijden J, Christiaans M, Edelbroek P, van Hooff JP, Stolk LM (2007) Therapeutic drug monitoring of tacrolimus with the dried blood spot method. J Pharm Biomed Anal 44(3):658–664
Hoogtanders K, van der Heijden J, Christiaans M, van de Plas A, van Hooff J, Stolk L (2007) Dried blood spot measurement of tacrolimus is promising for patient monitoring. Transplantation. 83(2):237–238
Acknowledgements
We would like to thank Dr. Nas Undre from Astellas Pharma for kindly providing us the raw data of the pharmacokinetic trial as published by Saint Marcoux et al. [14]. Dr. Undre nor Astellas was otherwise involved in our study. We would also like to thank our trial nurse, Mrs. Monique Mullens, and the nurse practitioners Mr. John Dackus and Mr. Philip Ulrichts for taking the blood samples during the trials that involved patients from our centre.
Author information
Authors and Affiliations
Contributions
FS collected and analysed the data, provided intellectual content of critical importance to the work, drafted and revised the manuscript. FV collected and analysed the data, provided intellectual content of critical importance to the work, drafted and revised the manuscript. CN conceived the study, provided intellectual content of critical importance to the work, revised and approved the version to be published. SvK provided intellectual content of critical importance to the work, revised and approved the version to be published. MC conceived the study, provided intellectual content of critical importance to the work, revised and approved the version to be published. Both authors FS and FV contributed equally to this manuscript.
Corresponding author
Ethics declarations
Ethical approval
All main studies cited above were conducted in accordance with the Declaration of Helsinki. The protocols had been reviewed by the Ethics Committee at each study centre and each patient had given written informed consent prior to enrolment into the study. The main studies were conducted between 2003 and 2004 [19, 20], i.e. before the cut-off date for registration of new and ongoing clinical trials and, thus, were not registered in a public trials registry. Collection, storage, and use of patient data were performed in agreement with FEDERA (Federation of Dutch University Medical Centers) Code of Conduct (www.nfu.nl).
Conflict of interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Stifft, F., Vandermeer, F., Neef, C. et al. A limited sampling strategy to estimate exposure of once-daily modified release tacrolimus in renal transplant recipients using linear regression analysis and comparison with Bayesian population pharmacokinetics in different cohorts. Eur J Clin Pharmacol 76, 685–693 (2020). https://doi.org/10.1007/s00228-019-02814-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02814-x