Abstract
Sarcopenia may increase non-alcoholic fatty liver disease (NAFLD) risk, but prevalence likely varies with different diagnostic criteria. This study examined the prevalence of sarcopenia and its defining components in adults with and without NAFLD and whether it varied by the method of muscle mass assessment [bioelectrical impedance (BIA) versus dual-energy X-ray absorptiometry (DXA)] and adjustment (height2 versus BMI). Adults (n = 7266) in the UK Biobank study (45–79 years) with and without NAFLD diagnosed by MRI, were included. Sarcopenia was defined by the 2018 European Working Group on Sarcopenia in Older People definition, with low appendicular skeletal muscle mass (ASM) assessed by BIA and DXA and adjusted for height2 or BMI. Overall, 21% of participants had NAFLD and the sex-specific prevalence of low muscle strength (3.6–7.2%) and sarcopenia (0.1–1.4%) did not differ by NAFLD status. However, NAFLD was associated with 74% (males) and 370% (females) higher prevalence of low ASM when adjusted for BMI but an 82% (males) to 89% (females) lower prevalence when adjusted for height2 (all P < 0.05). The prevalence of impaired physical function was 40% (males, P = 0.08) to 123% (females, P < 0.001) higher in NAFLD. In middle-aged and older adults, NAFLD was not associated with a higher prevalence of low muscle strength or sarcopenia but was associated with an increased risk of impaired physical function and low muscle mass when adjusted for BMI. These findings support the use of adiposity-based adjustments when assessing low muscle mass and the assessment of physical function in NAFLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Non-alcoholic fatty liver disease (NAFLD) is now estimated to affect approximately 30% of the adult population [1] with the growing burden of NAFLD strongly related to modifiable lifestyle factors such as poor dietary habits and physical inactivity [2]. Low skeletal muscle mass, a key component of the disease sarcopenia (defined as low muscle mass, strength and function) has emerged as an independent risk factor for NAFLD and its severity, with some evidence that low muscle mass is associated with a 30% increased risk of NAFLD [3]. While muscle loss and NAFLD share several common underlying risk factors including systemic inflammation and insulin resistance in their pathophysiology and progression [4], there are mixed findings from the limited studies available with regard to the prevalence of low muscle mass in adults with NAFLD.
The prevalence of low muscle mass in NAFLD adults has reported to range from 0 to 63% [5,6,7,8,9]. This heterogeneity is likely due to differences in participant demographics, the method of assessment for muscle mass [dual-energy X-ray absorptiometry (DXA) or bioelectrical impedance analysis (BIA)], the method of muscle mass adjustment to account for differences in body size (e.g. height2, BMI or weight) and/or the cut-off values used to define low muscle mass [10, 11]. For example, a study in 156 older adults with NAFLD, in which 72% were obese, reported a significantly higher prevalence of low appendicular skeletal muscle mass (ASM) when adjusted for BMI compared to height2 (26% vs 13.5%) [6]. This is likely explained by previous research showing that adiposity can mask the prevalence of low muscle mass as higher BMI has been associated with greater absolute but lower relative muscle mass [12, 13]. Thus, in obesity-related metabolic disorders such as NAFLD it may be more relevant to use adiposity-adjusted definitions and cut-offs for defining low muscle mass and the prevalence of sarcopenia.
Current operational definitions of sarcopenia have evolved to incorporate low muscle mass in combination with low muscle strength and impaired physical function, with the 2018 European Working Group of Sarcopenia in Older People (EWGSOP2) definition being the most widely utilised [10]. Of the available studies assessing two or more components of sarcopenia in adults with NAFLD, the prevalence has ranged from 0.5 to 38.6% but these studies have used different definitions, cut-off points, and adjustment methods which makes comparison challenging [12, 14, 15]. To our knowledge, only two studies have assessed the prevalence of sarcopenia in those with NAFLD (age 26–73 years) using EWGSOP2, reporting a prevalence ranging from 0.0 to 1.6% [9, 16]. Since NAFLD has a higher likelihood of obesity [2], low muscle mass and sarcopenia prevalence may be underestimated given the EWGSOP2 definition recommends adjustment of muscle mass for height2. Therefore, the primary aim of this study was to estimate the prevalence of sarcopenia and its defining components (low muscle strength, low muscle mass or impaired physical function) in middle-aged and older adults with NAFLD compared to those without NAFLD. Secondary aims were to determine whether the prevalence differs according to methods of muscle mass adjustment (height2 versus BMI) and methods of assessment (BIA versus DXA), and to evaluate the level of agreement between these adjustment methods and assessments.
Methods
Study Design
This study was a secondary analysis of cross-sectional data from the UK Biobank resource under application number 73818. The UK Biobank is a long-term prospective study following the health of over 500,000 adults living in the UK aged between 40 and 69 years, first recruited between 2006 and 2010 [17]. Participants were recruited via centrally coordinated identification and invitation from population-based registers (including the National Health Service). At baseline, health-related information (socio-demographics, lifestyle, family history, health, and medical history) was obtained through self-completed touch screen questionnaires. Anthropometry, body composition (assessed by BIA) and grip strength were also assessed, and biological samples taken [17]. In 2014 the UK Biobank imaging enhancement protocol was initiated incorporating abdominal MRI and full body DXA scans [17], with data from the first 10,012 participants who completed the imaging component included in this analysis. The UK Biobank study was approved by the Northwest Multicentre Research Ethics Committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Informed consent was given by all participants at the time of recruitment.
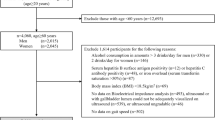
Participants
From a total of 502,488 participants enrolled in the UK Biobank study, 10,012 had available MRI liver imaging scans to quantify NAFLD. Of these, participants were excluded if they had missing MRI derived liver proton density fat fraction (PDFF) (n = 120) and/or unknown alcohol consumption (n = 75). Participants with excessive weekly alcohol consumption (n = 2297) (women > 112 g ethanol; men > 168 g ethanol), presence of other causes of liver disease (hepatitis B, hepatitis C, alcoholic liver disease or toxic liver diseases, n = 14), or missing data on the presence of one or more comorbidities (cancer, type 2 diabetes, cardiovascular disease, n = 29), were excluded. For investigation of sarcopenia, 221 participants were excluded due to missing data for one or more of the following variables: height, weight, grip strength, walking pace or fat free mass (FFM) assessed via BIA (Fig. 1). A subset of 3459 participants had a whole body DXA scan, and their demographic and health/medical characteristics were similar to the full cohort (n = 7266) that had a BIA assessment (Supplementary Table 1). For regression analysis, participants were further excluded if there were missing data for smoking status (n = 14) and/or physical activity (n = 1092), which were used as covariates.
Measures
Demographics and Health/Medical History
Information on demographic characteristics [age, sex, and ethnicity (white: British, White and Black Caribbean, Indian, Caribbean) or (non-white: mixed, Asian or Asian British, Black or Black British, Chinese, other ethnic group)] and history of diseases/illnesses (comorbidities) were collected via a touchscreen questionnaire. For the latter, participants were asked if they had ever been diagnosed by a doctor with the following: diabetes, vascular/heart problems (heart attack, angina, stroke, high blood pressure) or cancer. Information about smoking status (never, previous, current) and alcohol intake (frequency and average weekly intake of red wine, white wine, beer, cider, spirits, fortified wine, and other drinks) was also derived via the touchscreen questionnaire. The NHS alcohol unit’s definition was used to calculate the weekly number of alcohol units and intake (in grams) to assess excessive alcohol consumption [18].
Liver Imaging and NAFLD Diagnosis
Liver images via MRI were acquired at the UK Biobank Imaging Centre. Hepatic fat was quantified via MRI (Siemens 1.5T MAGNETOM Area) derived PDFF using a 6-min dual-echo Dixon vibe protocol [19]. As reported previously [20], a single transverse slice was captured, taken at the porta hepatitis. Liver images were analysed using LiverMultiScan™ Discover software (Perspectum Diagnostics) to obtain measures of liver fat % and MR echoes used to create PDFF maps using a three-point DIXON technique [21]. NAFLD was defined as > 5% liver fat in the absence of excessive alcohol consumption and presence of other causes of liver disease. MRI derived PDFF has been shown to correlate strongly with histopathological liver triglyceride content [22].
Definition of Sarcopenia
Sarcopenia was defined as probable sarcopenia [low muscle (grip) strength] and confirmed with the addition of low ASM for BIA and low appendicular lean mass (ALM) for DXA, with severe sarcopenia identified when impaired physical function was also present. The diagnostic criteria and cut-off points recommended by the EWGSOP2 guidelines were used for low grip strength and low ASM/ALM [10] as indicated below.
Muscle (Lean) Mass
Low ASM was estimated from FFM (sum of arms and legs) assessed by BIA using a Tanita BC418MA body composition analyser. Since BIA does not measure ASM, it was estimated using the following equation developed by Dodds et al. [23] using data from UK Biobank participants who had a total body DXA scan to evaluate appendicular lean mass: ASM (kg) = (0.958 × appendicular FFM (kg) − (0.166 × S) −0.308, with S being given the value 0 if female or 1 if male. In addition, a subset of UK Biobank participants had a total body DXA scan (GE-Lunar, Madison W1) performed by a trained radiographer which was used to assess total body and regional (arms, legs, and trunk) lean mass. Lean mass for the arms and legs was summed to calculate ALM (kg).
Two techniques were used to adjust ASM and ALM for body size: (1) ASM/ALM adjusted for height (in metres squared); and (2) ASM/ALM adjusted for BMI. The following sex-specific cut-points were used for both the BIA and DXA measures to indicate low muscle mass: (1) Low ASM or ALM divided by height2; < 7.0 kg/m2 for males; < 5.5 kg/m2 for females; [10] and (2) low ASM or ALM divided by BMI; < 0.789 for males; < 0.512 for females [11].
Muscle (Grip) Strength
Low muscle strength was assessed via hand grip strength using a Jamar J00105 hydraulic hand dynamometer (Lafayette Instrument, USA). Participants were instructed to sit upright in a chair with elbows at 90° flexion with forearms placed on arm rests in the mid prone position. Hand grip strength was measured once for both the left and right arm using a 3-s maximum grip effort. The maximum value (in kg) for either arm was used as the result. Low muscle strength was defined as < 27 kg for males and < 16 kg for females [10].
Physical Function
Impaired physical function for the assessment of sarcopenia is typically based on an assessment of gait speed [10], but since the UK Biobank did not include a physical assessment of function, self-reported usual walking pace (1 unable to walk, 2 slow, 3 steady, or 4 brisk) was assessed via the touchscreen questionnaire and used as a surrogate estimate of physical function. As reported in previous studies using the UK Biobank data [23], impaired physical function was defined as unable to walk or walked at a slow pace.
Physical Activity
Physical activity was assessed via questions adapted from the validated short International Physical Activity Questionnaire (IPAQ) [24]. Questions encompassed the frequency, intensity and duration of walking and moderate and vigorous physical activity. Total physical activity expressed as MET min/week was determined by calculating the energy expended for the following activities: time spent in vigorous and moderate activity and walking. MET min/week = Walk (METs*min*days) + Moderate activity (METs*min*days) + Vigorous (METs*min*days [24].
Anthropometry
Height (in cm) was measured using a Seca stadiometer (Seca, Hamburg, Germany). Weight (in kg) was assessed using a Tanita BC418MA body composition analyser. Body mass index (BMI; kg/m2) was assessed from weight (kg) divided by height (m2).
Statistical Analysis
All analyses were performed using Stata Statistical software version 17.0. Descriptive statistics are presented as mean and SD or frequency counts and proportions (percentages). Independent t-tests (continuous variables) and chi-square tests (categorical variables) were used to compare baseline characteristics and the prevalence of low muscle strength, low ASM/ALM, and impaired physical function between participants with and without NAFLD. All results are presented for males and females separately. Generalised linear models, using a binomial family and log link function were used to estimate prevalence ratios with 95% confidence intervals for predicting low muscle strength (probable sarcopenia), low ASM/ALM, and impaired physical function, dependent upon the presence of NAFLD. Models were analysed unadjusted (model 1) and adjusted for age, physical activity, smoking status and number of comorbidities (model 2) and additionally adjusted for BMI (model 3). For low ASM/ALM outcomes, model 3 was not used, as ASM/ALM was already adjusted for height2 or BMI. Due to very small numbers of participants with confirmed and severe sarcopenia, no model was fitted for this exposure variable. Separate models were fitted for each individual exposure variable. The models included the exposure variable sex and their interaction, to estimate prevalence ratios for males and females separately as well as estimate sex differences in prevalence ratios. The Kappa test was used to evaluate the level of agreement between low ALM/ASM adjusting for height2 and BMI and sarcopenia using DXA and BIA. The strength of agreement (Kappa coefficients) was interpreted as < 0 no, 0–0.20 slight, 0.21–0.39 fair, 0.40–0.59 moderate, 0.61–0.80 substantial, and ≥ 0.81 almost perfect agreement [25]. Positive and negative predictive agreements were used to reflect the proportion of participants who were classified into low muscle mass or sarcopenia criteria (PPA%) or not having low muscle mass or sarcopenia (NPA%) [26]. Statistical significance was set at P < 0.05.
Results
Participant Characteristics
The characteristics of the participants by NAFLD status and sex are shown in Table 1. The mean ± SD age of participants was 62.7 ± 7.6 years with 54.9% female. Overall, 21.8% of the participants (n = 1582) had NAFLD, with a higher proportion in males compared to females (27.0% vs 17.5%). The mean PDFF for females and males with NAFLD was 11.3 ± 6.3% and 10.5 ± 10.1%, respectively. Participants with NAFLD were more likely to be obese (males 49% vs 13%; females 43% vs 10%, respectively) and have lower physical activity levels (all P < 0.001) and a higher prevalence of comorbidities.
Regarding the components of sarcopenia, the mean absolute ASM/ALM (by BIA and DXA) was 1.3–2.8 kg higher (all, P < 0.001) in both males and females with NAFLD. Similarly, mean ASM/ALM adjusted for height was higher (8.1–11.1%, all, P < 0.001) in males and females with NAFLD. In contrast, ASM/ALM adjusted for BMI was 4.1–11.1% lower (all, P < 0.001) in both males and females with NAFLD. While there was a trend (P = 0.062) for grip strength to be 0.5 kg lower in females with NAFLD, a significantly higher proportion of males and females with NAFLD reported a slow or steady compared to brisk walking pace indicative of impaired physical function (both P < 0.001; Table 1).
Prevalence of Sarcopenia and Its Components
The sex-specific estimated prevalence of low muscle strength, mass (ASM/ALM) and impaired physical function in those with and without NAFLD and their prevalence ratios according to NAFLD are reported in Table 2. Similar results were observed in the subset of participants with both DXA and BIA scans (Supplementary Table 2).
Low Muscle Strength (Probable Sarcopenia)
The estimated prevalence of low muscle strength was not statistically different for those with and without NAFLD ranging from 3.6 to 7.2%, and there was no significant sex interaction (P = 0.066) for the prevalence ratio (Table 2).
Low Muscle Mass
Using BIA, the estimated prevalence of low muscle mass (ASM) adjusting for height2 was greater in non-NAFLD than NAFLD females (2.4% vs 0.6%) and males (9.5% vs 1.2%), with an estimated 92–89% (both P < 0.05 for model 2) lower prevalence in males and females with NAFLD, respectively. In contrast, the prevalence of low muscle mass (ASM) adjusted for BMI was higher in both females (2.2% vs 0.4%) and males (4.4% vs 2.5%) with NAFLD, with an associated 74% and 370% (both P < 0.05 to < 0.01 for model 2) higher prevalence in males and females, respectively, with no significant sex interaction (P = 0.068). Using DXA, similar significant findings between NALFD and non-NAFLD males and females were observed for the prevalence of low muscle mass (ALM) after adjusting for height2 and BMI. However, the overall prevalence of low muscle mass for both NAFLD and non-NAFLD participants was 1.1 to 6.5-fold higher based on DXA compared to BIA (Table 2).
Impaired Physical Function
The estimated prevalence of impaired physical function was 2-3-fold greater in both females and males with NAFLD, with the prevalence ratio (model 2) being 40% (P = 0.09) higher in males and 123% (P < 0.001) higher in females with NAFLD compared without NAFLD, with no significant sex interaction (P = 0.083) (Table 2).
Sarcopenia and Severe Sarcopenia
Regardless of NAFLD status, the overall prevalence of confirmed sarcopenia was low for both females (0.14–0.43%) (Fig. 2) and males (0.11–0.67%) in this study when ASM was measured by BIA (Fig. 3). Similar findings (albeit slightly higher prevalence’s) were observed when ALM was assessed by DXA (females 0.29–1.20%; males 0.72–1.44%). The overall prevalence of severe sarcopenia (inclusive of impaired function) ranged from 0% to 0.58%, regardless of sex or the method of assessment or adjustment.
Prevalence of low muscle strength (probable sarcopenia), sarcopenia, and severe sarcopenia in females with and without NAFLD according to BIA (panel a) and DXA (panel b) with figures presenting proportions for each group (NAFLD and non-NAFLD). BIA, bioelectrical impedance analysis; DXA, dual-energy X-ray absorptiometry; NAFLD, non-alcoholic fatty liver disease. a Low ASM/ALM adjusted for height2, b Low ASM/ALM adjusted for BMI
Prevalence of low muscle strength (probable sarcopenia), sarcopenia, and severe sarcopenia in males with and without NAFLD according to BIA (panel a) and DXA (panel b) with figures presenting proportions for each group (NAFLD and non- NAFLD). BIA, bioelectrical impedance analysis; DXA, dual-energy X-ray absorptiometry; NAFLD, non-alcoholic fatty liver disease. a Low ASM/ALM adjusted for height2, b Low ASM/ALM adjusted for BMI
Agreement Between the Body Composition Methods of Assessment and Adjustment
Overall, the level of agreement for low muscle mass and sarcopenia based on the method of adjustment (height2 versus BMI) using either BIA or DXA was poor (Kappa, 0.00–0.08; PPA%, 0.0–12.0%) (Table 3). In contrast, agreement for low muscle mass and sarcopenia according to the method of assessment (BIA versus DXA) whether adjusted for height2 or BMI was moderate (Kappa, 0.38–0.58). The NPA% was high for all criteria.
Discussion
The main finding from this study was that the overall prevalence of sarcopenia, defined as low muscle strength and mass, was very low (0.1–1.4%) and not different between middle-aged and older adults with or without NAFLD, regardless of the assessment (DXA versus BIA) or adjustment method for muscle mass (height2 versus BMI). Regarding the individual components of sarcopenia, the prevalence of low muscle strength was similar between NAFLD and non-NAFLD males and females (range 3.6–7.2%), but the prevalence of low muscle mass when adjusting for BMI versus height2 was different and in opposite directions, which was confirmed by the low agreement (Kappa 0.01–0.04) between the two adjustment methods (height2 versus BMI). Finally, for impaired physical function the risk (prevalence ratio) was 40 and 123% higher in males and females with NAFLD, respectively. Collectively, these findings suggest that in this select sample of UK middle-aged and older adults with NAFLD, muscle strength is not compromised compared to those without NAFLD, but they have low muscle mass when accounting for their increased adiposity, and impaired physical function.
The overall low prevalence of sarcopenia in our study in those with (and without) NAFLD is likely attributable to the demographic characteristics of the UK Biobank cohort. The mean age of participants in our study was 62.7 years (range 45–79) with 36% being under 60 years of age. Previous research in community dwelling middle-aged and older adults using the EWGSOP2 criteria to diagnose sarcopenia have reported the prevalence to range from 0.4 to 8.6% [27, 28] increasing to 8.1–20.0% in those > 70 years [29,30,31]. Despite evidence that the presence of chronic disease [32], including NAFLD [3], is associated with an increased risk of sarcopenia, we found no apparent difference between those with and without NAFLD, despite those with NAFLD having a higher prevalence of obesity and co-morbidities. The main reason for the lack of any differences in sarcopenia prevalence in our study is because muscle strength (the initial component of the sarcopenia definition) was not compromised in those with NAFLD. Previous studies examining the effects of NAFLD on muscle strength have reported mixed findings [16, 33] which may be related in part, to differences in the age of participants across studies and/or the potential confounding effects of body size (obesity). Indeed, there is some evidence that muscle (grip) strength is compromised in those with NAFLD when adjusted for BMI or weight [14, 33,34,35]. Although the current EWGSOP2 definition of sarcopenia does not recommend adjusting muscle strength for BMI or weight, when we adjusted absolute grip strength by BMI, we found it was 13.4% and 19.2% lower in males and females with NAFLD, respectively compared to those without NAFLD (data not shown). Based on these findings, further research is warranted to investigate whether normalising muscle strength for some measure of body size should be considered when evaluating the prevalence of low muscle strength, particularly in populations with increased adiposity, and what cut-offs should be used to define low muscle strength.
Another key finding was that the prevalence of low muscle mass in those with and without NAFLD was significantly different (and in the opposite direction) when adjusting for BMI versus height2, which is in concordance with the poor agreement (Kappa 0.01–0.04) we observed between the two adjustment methods. On average, those with NAFLD had significantly higher BMI and absolute (kg) muscle mass but when adjusted for BMI the prevalence ratio of low muscle mass was significantly higher in those with NAFLD; the opposite finding was observed when adjusted for height2. Previous studies have also reported a higher prevalence of low muscle mass when adjusting for BMI in those with NAFLD (8.7% vs 3.6%) [36] and no differences when adjusting for height2 [5]. This suggests that it is important to account for adiposity when evaluating the influence of NAFLD on muscle mass, especially in overweight and obese cohorts.
Another interesting observation from our study was that the overall prevalence of low muscle mass (and sarcopenia) was 1.1 to 6.5-fold higher when assessed by DXA compared to BIA, irrespective of NAFLD status or the method of adjustment. This is in alignment with the moderate agreement between DXA and BIA for quantifying low muscle mass in our cohort (Kappa 0.38–0.58, P < 0.001). These findings are likely explained by the fact that estimates of FFM and appendicular lean mass are typically overestimated by BIA, but this may also vary according to BMI [37, 38]. In our study, to estimate ASM from BIA we utilised a previously published equation developed from 4350 UK Biobank participants who had both a BIA and DXA scan, but the authors did not report on the level of agreement between DXA ALM and BIA estimated ASM in this study [23]. However, another study from the UK Biobank which validated BIA with DXA in 905 men and women reported that BIA overestimated ASM compared to DXA by 2.5% (women) and 1.9% (men) [39]. This confirms previous findings that BIA likely underestimates the prevalence of low muscle mass compared to DXA if using the same cut-off values [40, 41].
Poor physical function (a key component of sarcopenia) is associated with a range of adverse outcomes including falls, disability, and mortality [10]. Our findings indicated NAFLD was associated with a 40–123% increased prevalence ratio of impaired function (self-reported slow walking speed), after adjusting for several confounders including age, physical activity, smoking status, and the presence of chronic diseases, which was significantly higher in females only. However, when including BMI as a confounder the prevalence of impaired function was not significantly different between those with and without NAFLD. This suggests that adiposity was also likely a key factor contributing to impaired function in those with NAFLD, which is consistent with previous research reporting that obesity is associated with a higher risk of functional impairment [42]. To date, there are mixed findings from the few studies that have assessed whether NAFLD adversely influences physical performance, but most studies have reported no adverse effects on measures such as gait speed [5, 12]. Given the limited evidence available, further research is warranted to evaluate the impact of NAFLD on physical function.
A key strength of this study was the assessment of sarcopenia using all three components in a relatively large Western population of middle-aged and older adults with and without NAFLD. Other strengths include the assessment of body composition by BIA and DXA and the assessment of liver fat by MRI liver imaging, which is considered the gold standard to quantify NAFLD [43]. There are however several limitations. First, the UK Biobank cohort has been reported to represent ‘healthy volunteer’ selection bias [44]. Second, this study included a subset of participants from the larger UK Biobank sample (> 500,000) and those that had imaging data collected in 2014 (~ 10,000) which could limit generalisability, but the characteristics of the participants in our study versus the whole cohort was comparable (proportion female 54.9% vs 54.4%; weight 75.9 kg vs 78.1 kg, BMI 26.6 kg/m2 vs 27.4 kg/m2; proportion white 93.7% vs 94.6%; diabetes diagnosis 5.6% vs 5.3%). Third, the overall low prevalence of sarcopenia of participants in this study limits our ability to draw definitive conclusions regarding the influence of NALFD on the risk of sarcopenia. Fourth, DXA was only available in a subset (47%) of participants. Fifth, the estimate of ASM from BIA based on the equation developed by Dodds et al. [23] likely overestimates appendicular muscle mass, which may introduce a systematic error (bias) for this measure. Sixth, although we adjusted for several relevant covariates, there may be other potential confounders not considered that could influence the findings (e.g. diet, certain medications). Dietary data for the 2014 time point was not available and therefore could not be considered in the analysis. Finally, physical function was self-reported and did not include relevant objective measures such as the 4-m walking (gait) speed test.
In summary, this study indicates that adults aged 45–79 years with NAFLD do not have an increased likelihood sarcopenia, regardless of the method of body composition assessment (DXA versus BIA) or adjustment (height2 versus BMI). This was likely due to absolute hand grip (muscle) strength not being compromised in those with NAFLD. However, NAFLD was associated with an increased risk for low muscle mass when adjusting for adiposity (BMI), but not for height2, and impaired physical function. These findings support the use of adiposity-based adjustments when assessing the risk for low muscle mass in adults with NAFLD. In view of the close association between NAFLD and adiposity, and the recent proposed consensus definition and recommendations related to sarcopenic obesity, future work investigating the prevalence and impact of sarcopenic obesity in this cohort is warranted [45]. Additionally, further research assessing physical function in NAFLD is needed to determine whether it should be considered as part of routine screening or assessment for this population given that impairment is strongly linked to many adverse health outcomes.
Change history
05 June 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00223-024-01235-y
References
Liu J, Tian Y, Fu X, Mu C, Yao M, Ni Y, Liu Y et al (2022) Estimating global prevalence, incidence, and outcomes of non-alcoholic fatty liver disease from 2000 to 2021: systematic review and meta-analysis. Chin Med J 135(14):1682-1691
Huang TD, Behary J, Zekry A (2019) Non-alcoholic fatty liver disease (NAFLD): a review of epidemiology, risk factors, diagnosis and management. Intern Med J 50(9):1038–1047
Cai C, Song X, Chen Y, Chen X, Yu C (2020) Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a systematic review and meta-analysis. Hepatol Int 14(1):115–126
Kim JA, Choi KM (2019) Sarcopenia and fatty liver disease. Hepatol Int 13(6):674–687
Alferink LJM, Trajanoska K, Erler NS, Schoufour JD, de Knegt RJ, Ikram MA, Janssen HLA et al (2019) Nonalcoholic fatty liver disease in the Rotterdam Study: about muscle mass, sarcopenia, fat mass, and fat distribution. J Bone Miner Res 34(7):1254–1263
Seko Y, Mizuno N, Okishio S, Takahashi A, Kataoka S, Okuda K, Furuta M et al (2019) Clinical and pathological features of sarcopenia-related indices in patients with non-alcoholic fatty liver disease. Hepatol Res 49(6):627–636
Koo BK, Kim D, Joo SK, Kim JH, Chang MS, Kim BG, Lee KL et al (2017) Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis. J Hepatol 66(1):123–131
Lee HJ, Chang JS, Ahn JH, Kim MY, Park K-S, Ahn Y-S, Koh SB (2021) Association between low muscle mass and non-alcoholic fatty liver disease diagnosed using ultrasonography, magnetic resonance imaging derived proton density fat fraction, and comprehensive NAFLD score in Korea. J Prev Med Public Health 54(6):412–421
Almeida NS, Rocha R, de Souza CA, da Cruz ACS, Ribeiro BDR, Vieira LV, Daltro C et al (2022) Prevalence of sarcopenia using different methods in patients with non-alcoholic fatty liver disease. World J Hepatol 14(8):1643–1651
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, Cooper C et al (2019) Sarcopenia: revised European consensus on definition and diagnosis. Age Aging 48(1):16–31
Studenski SA, Peters KW, Alley DE, Cawthon PM, McLean RR, Harris TB, Ferrucci L et al (2014) The FNIH sarcopenia project: rationale, study description, conference recommendations, and final estimates. J Gerentol 69(5):547–558
Peng T-C, Wu L-W, Chen W-L, Liaw F-Y, Chang Y-W, Kao T-W (2019) Nonalcoholic fatty liver disease and sarcopenia in a Western population (NHANES III): the importance of sarcopenia definition. Clin Nutr 38(1):422–428
Meng NH, Li CI, Liu CS, Lin CH, Lin WY, Chang CK, Li TC et al (2015) Comparison of height-and weight-adjusted sarcopenia in a Taiwanese metropolitan older population. Geriatr Gerontol Int 15(1):45–53
Gan D, Wang L, Jia M, Ru Y, Ma Y, Zheng W, Zhao X et al (2020) Low muscle mass and low muscle strength associate with nonalcoholic fatty liver disease. Clin Nutr 39(4):1124–1130
Wang Y-M, Zhu K-F, Zhou W-J, Zhang Q, Deng D-F, Yang Y-C, Lu W-W et al (2021) Sarcopenia is associated with the presence of nonalcoholic fatty liver disease in Zhejiang Province, China: a cross-sectional observational study. BMC Geriatr 21(1):55
Linge J, Ekstedt M, Leinhard OD (2021) Adverse muscle composition is linked to poor functional performance and metabolic comorbidities in NAFLD. JHEP Rep 3(1):100197
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P et al (2015) UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12(3):e1001779
National Health Service: Alcohol Units—NHS; 2021. https://www.nhs.uk/live-well/alcohol-advice/calculating-alcohol-units/. Accessed 11 Nov 2022
Dixon WT (1984) Simple proton spectroscopic imaging. Radiology 153(1):189–194
Wilman HR, Kelly M, Garratt S, Matthews PM, Milanesi M, Herlihy A, Gyngell M et al (2017) Characterisation of liver fat in the UK Biobank cohort. PLoS ONE 12(2):e0172921
Glover GH (1991) Multipoint Dixon technique for water and fat proton and susceptibility imaging. J Magn Reson Imaging 1(5):521–530
Ahn SB, Jun DW, Kang B-K, Kim M, Chang M, Nam E (2018) Optimal cutoff value for assessing changes in intrahepatic fat amount by using the controlled attenuation parameter in a longitudinal setting. Medicine 97(50):e13636
Dodds RM, Granic A, Robinson SM, Sayer AA (2020) Sarcopenia, long-term conditions, and multimorbidity: findings from UK Biobank participants. J Cachexia Sarcopenia Muscle 11(1):62–68
Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, Pratt M et al (2003) International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 35(8):1381–1395
Viera AJ, Garrett JM (2005) Understanding interobserver agreement: the kappa statistic. Fam Med 37(5):360–363
Safari S, Baratloo A, Elfil M, Negida A (2015) Evidence based emergency medicine part 2: positive and negative predictive values of diagnostic tests. Emerg 3(3):87–88
Martone AM, Marzetti E, Salini S, Zazzara MB, Santoro L, Tosato M, Picca A et al (2020) Sarcopenia identified according to the EWGSOP2 definition in community-living people: prevalence and clinical features. J Am Med Dir Assoc 21(10):1470–1474
Dietzel R, Wiegmann S, Borucki D, Detzer C, Zeiner KN, Schaumburg D, Buehring B et al (2022) Prevalence of sarcopenia in patients with rheumatoid arthritis using the revised EWGSOP2 and the FNIH definition. RMD Open 8(2):e002600
Sobestiansky S, Michaelsson K, Cederholm T (2019) Sarcopenia prevalence and associations with mortality and hospitalisation by various sarcopenia definitions in 85–89 year old community-dwelling men: a report from the ULSAM study. BMC Geriatr 19(1):318
Su Y, Hirayama K, Han T-F, Izutsu M, Yuki M (2019) Sarcopenia prevalence and risk factors among Japanese community dwelling older adults living in a snow-covered city according to EWGSOP2. J Clin Med 8(3):291
Moreno-Gonzalez R, Corbella X, Mattace-Raso F, Tap L, Sieber C, Freiberger E, Kostka T et al (2020) Prevalence of sarcopenia in community-dwelling older adults using the updated EWGSOP2 definition according to kidney function and albuminuria. BMC Geriatr 20(1):327
Pacifico J, Geerlings MA, Reijnierse EM, Phassouliotis C, Lim WK, Maier AB (2020) Prevalence of sarcopenia as a comorbid disease: a systematic review and meta-analysis. Exp Gerentol 131(3):110801
Lee K (2018) Relationship between handgrip strength and nonalcoholic fatty liver disease: nationwide surveys. Metab Syndr Relat Disord 16(9):497–503
Meng G, Wu H, Fang L, Li C, Yu F, Zhang Q, Liu L et al (2016) Relationship between grip strength and newly diagnosed nonalcoholic fatty liver disease in a large-scale adult population. Sci Rep 6(1):1–7
Park SH, Kim DJ, Plank LD (2020) Association of grip strength with non-alcoholic fatty liver disease: investigation of the roles of insulin resistance and inflammation as mediators. Eur J Clin Nutr 74(10):1401–1409
Seo JY, Cho EJ, Kim MJ, Kwak M-S, Yang JI, Chung SJ, Yim JY et al (2022) The relationship between metabolic dysfunction-associated fatty liver disease and low muscle mass in an asymptomatic Korean population. J Cachexia Sarcopenia Muscle 13(6):2953–2960
Ballesteros-Pomar MD, González-Arnáiz E, Pintor-de-la Maza B, Barajas-Galindo D, Ariadel-Cobo D, González-Roza L, Cano-Rodríguez I (2022) Bioelectrical impedance analysis as an alternative to dual-energy x-ray absorptiometry in the assessment of fat mass and appendicular lean mass in patients with obesity. Nutrition 93:111442
Achamrah N, Colange G, Delay J, Rimbert A, Folope V, Petit A, Grigioni S et al (2018) Comparison of body composition assessment by DXA and BIA according to the body mass index: a retrospective study on 3655 measures. PLoS ONE 13(7):e0200465
Lee MM, Jebb SA, Oke J, Piernas C (2020) Reference values for skeletal muscle mass and fat mass measured by bioelectrical impedance in 390 565 UK adults. J Cachexia Sarcopenia Muscle 11(2):487–496
Lee SY, Ahn S, Kim YJ, Ji MJ, Kim KM, Choi SH, Jang HC et al (2018) Comparison between dual-energy X-ray absorptiometry and bioelectrical impedance analyses for accuracy in measuring whole body muscle mass and appendicular skeletal muscle mass. Nutrients 10(6):738
Wingo BC, Barry VG, Ellis AC, Gower BA (2018) Comparison of segmental body composition estimated by bioelectrical impedance analysis and dual-energy X-ray absorptiometry. Clin Nutr 28:141–147
Kalyani RR, Corriere M, Ferrucci L (2014) Age-related and disease-related muscle loss: the effect of diabetes, obesity, and other diseases. Lancet Diabetes Endocrinol 2(10):819–829
Kinner S, Reeder SB, Yokoo T (2016) Quantitative imaging biomarkers of NAFLD. Dig Dis Sci 61(5):1337–1347
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R et al (2017) Comparison of sociodemographic and health-related characteristics of UK biobank participants with those of the general population. Am J Epidemiol 186(9):1026–1034
Donini LM, Busetto L, Bischoff SC, Cederholm T, Ballesteros-Pomar MD, Batsis JA, Bauer JM et al (2022) Definition and diagnostic criteria for sarcopenic obesity: ESPEN and EASO consensus statement. Clin Nutr 41(4):990–1000
Acknowledgements
CLF was supported by a Deakin University Higher Degree by Research Scholarship. ESG was supported by a Deakin University, Faculty of Health Dean’s Postdoctoral Fellowship. The salary of DS was supported by a National Health and Medical Research Council Australia Investigator Grant. The authors thank the UK Biobank participants and research team. This research has been conducted using the UK Biobank resource under application number 73818.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
RMD reports honoraria for educational presentations from Abbott Nutrition and Fresenius Kabi. DS reports a clinical grant from Amgen Australia and honoraria from Abbott Nutrition, Amgen Australian and Pfizer. Christine L. Freer, Elena S. George, Sze-Yen Tan, Gavin Abbott declare no conflict of interest.
Human and Animal Rights
The UK Biobank study was approved by the Northwest Multicentre Research Ethics Committee and performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
Informed consent was given by all participants at the time of recruitment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of the article was revised: P values in Tables 1 and 2 have been corrected.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Freer, C.L., George, E.S., Tan, SY. et al. Prevalence of Sarcopenia and Its Defining Components in Non-alcoholic Fatty Liver Disease Varies According to the Method of Assessment and Adjustment: Findings from the UK Biobank. Calcif Tissue Int 114, 592–602 (2024). https://doi.org/10.1007/s00223-024-01212-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-024-01212-5