Abstract
Background and aims
Despite the association between sarcopenia and non-alcoholic fatty liver disease (NAFLD), no study has evaluated the predictive role of NAFLD in sarcopenia. We investigated impact of NAFLD on the risk of low muscle mass (LMM) and low muscle strength (LMS) in a nationwide multicenter study.
Methods
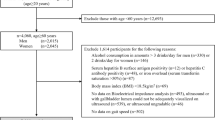
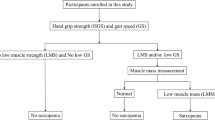
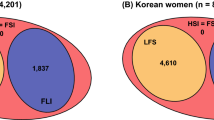
A total of 1595 community-dwelling people aged 70–84 years were followed for 2 years in the Korean Frailty and Aging Cohort Study. Muscle mass was estimated by dividing appendicular skeletal muscle mass (ASM) by body mass index (BMI). Muscle strength was measured as handgrip strength (HGS) divided by BMI. The sex-specific lowest quintiles of ASM/BMI and HGS/BMI of the study population were used as cutoffs for LMM and LMS, respectively. The risk of LMM and LMS were assessed according to hepatic steatosis index (HSI) and fatty liver index (FLI) quartiles.
Results
As HSI quartiles increased, the LMM risk increased gradually, after adjusting for age, sex, lifestyle factors, comorbidities, and several causative factors (insulin resistance, inflammation, and vitamin D) (Q4 vs. Q1 OR [95% CI] 3.46 [2.23–5.35]). The increased risk of LMS was even higher according to HSI quartiles (Q4 vs. Q1 5.81 [3.67–9.21]). Multivariate analyses based on FLI showed similar results. People with NAFLD (HSI > 36) were at higher risk of developing LMM and LMS compared to those without (1.65 [1.19–2.31] and 2.29 [1.61–3.26], respectively).
Conclusions
The presence of NAFLD may predict future risk of LMM and LMS, with greater impact on LMS than on LMM.
Graphic abstract



Similar content being viewed by others
Data availability
Access to anonymized data may be granted following review.
Abbreviations
- ALT:
-
Alanine aminotransferase
- ASM:
-
Appendicular skeletal muscle mass
- AST:
-
Aspartate aminotransferase
- BMI:
-
Body mass index
- DXA:
-
Dual-energy X-ray absorptiometry
- FLI:
-
Fatty liver index
- FNIH:
-
Foundation for the National Institutes of Health
- FPG:
-
Fasting plasma glucose
- GGT:
-
γ-Glutamyl transferase
- HbA1c:
-
Hemoglobin A1c
- HGS:
-
Handgrip strength
- HOMA-IR:
-
Homeostatic model assessment of insulin resistance
- hs-CRP:
-
High-sensitivity C-reactive protein
- HIS:
-
Hepatic steatosis index
- KFACS:
-
Korean Frailty and Aging Cohort Study
- KNHANES:
-
Korean National Health and Nutrition Examination Survey
- LMM:
-
Low muscle mass
- LMS:
-
Low muscle strength
- NAFLD:
-
Nonalcoholic fatty liver disease
- OR:
-
Odds ratio
- SBP:
-
Systolic blood pressure
- TG:
-
Triglycerides
- WC:
-
Waist circumference
References
Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10:686–690
Shafiee G, Keshtkar A, Soltani A, Ahadi Z, Larijani B, Heshmat R. Prevalence of sarcopenia in the world: a systematic review and meta- analysis of general population studies. J Diabetes Metab Disord. 2017;16:21
Roh E, Choi KM. Health consequences of sarcopenic obesity: a narrative review. Front Endocrinol (Lausanne). 2020;11:332
Kim D, Wijarnpreecha K, Sandhu KK, Cholankeril G, Ahmed A. Sarcopenia in nonalcoholic fatty liver disease and all-cause and cause-specific mortality in the United States. Liver Int. 2021;41(8):1832–1840
Hong HC, Hwang SY, Choi HY, Yoo HJ, Seo JA, Kim SG, et al. Relationship between sarcopenia and nonalcoholic fatty liver disease: the Korean Sarcopenic Obesity Study. Hepatology. 2014;59:1772–1778
Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, et al. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008–2011). J Hepatol. 2015;63:486–493
Kim G, Lee SE, Lee YB, Jun JE, Ahn J, Bae JC, et al. Relationship between relative skeletal muscle mass and nonalcoholic fatty liver disease: a 7-year longitudinal study. Hepatology. 2018;68:1755–1768
Lee MJ, Kim EH, Bae SJ, Kim GA, Park SW, Choe J, et al. Age-related decrease in skeletal muscle mass is an independent risk factor for incident nonalcoholic fatty liver disease: a 10-year retrospective cohort study. Gut Liver. 2019;13:67–76
Cruz-Jentoft AJ, Bahat G, Bauer J, Boirie Y, Bruyère O, Cederholm T, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing. 2019;48:601
Leong DP, Teo KK, Rangarajan S, Lopez-Jaramillo P, Avezum A Jr, Orlandini A, et al. Prognostic value of grip strength: findings from the Prospective Urban Rural Epidemiology (PURE) study. Lancet. 2015;386:266–273
Meng G, Wu H, Fang L, Li C, Yu F, Zhang Q, et al. Relationship between grip strength and newly diagnosed nonalcoholic fatty liver disease in a large-scale adult population. Sci Rep. 2016;6:33255
Kang S, Moon MK, Kim W, Koo BK. Association between muscle strength and advanced fibrosis in non-alcoholic fatty liver disease: a Korean nationwide survey. J Cachexia Sarcopenia Muscle. 2020;11:1232–1241
Gan D, Wang L, Jia M, Ru Y, Ma Y, Zheng W, et al. Low muscle mass and low muscle strength associate with nonalcoholic fatty liver disease. Clin Nutr. 2020;39:1124–1130
Tilg H, Moschen AR. Insulin resistance, inflammation, and non-alcoholic fatty liver disease. Trends Endocrinol Metab. 2008;19:371–379
Kim JA, Choi KM. Sarcopenia and fatty liver disease. Hepatol Int. 2019;13:674–687
Won CW, Lee S, Kim J, Chon D, Kim S, Kim C-O, et al. Korean frailty and aging cohort study (KFACS): cohort profile. BMJ Open. 2020;10:e035573
McLean RR, Shardell MD, Alley DE, Cawthon PM, Fragala MS, Harris TB, et al. Criteria for clinically relevant weakness and low lean mass and their longitudinal association with incident mobility impairment and mortality: the foundation for the National Institutes of Health (FNIH) sarcopenia project. J Gerontol A Biol Sci Med Sci. 2014;69:576–583
Moon JH, Kim KM, Kim JH, Moon JH, Choi SH, Lim S, et al. Predictive values of the new sarcopenia index by the Foundation for the National Institutes of Health Sarcopenia Project for mortality among older Korean adults. PLoS ONE. 2016;11:e0166344
Lee J-H, Kim D, Kim HJ, Lee C-H, Yang JI, Kim W, et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis. 2010;42:503–508
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol. 2006;6:33
Kotronen A, Peltonen M, Hakkarainen A, Sevastianova K, Bergholm R, Johansson LM, et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology. 2009;137:865–872
Harrison SA, Oliver D, Arnold HL, Gogia S, Neuschwander-Tetri BA. Development and validation of a simple NAFLD clinical scoring system for identifying patients without advanced disease. Gut. 2008;57:1441–1447
Kim KM, Jang HC, Lim S. Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia. Korean J Intern Med. 2016;31:643–650
Lim S, Kim JH, Yoon JW, Kang SM, Choi SH, Park YJ, et al. Sarcopenic obesity: prevalence and association with metabolic syndrome in the Korean Longitudinal Study on Health and Aging (KLoSHA). Diabetes Care. 2010;33:1652–1654
Kim TN, Park MS, Lee EJ, Chung HS, Yoo HJ, Kang HJ, et al. Comparisons of three different methods for defining sarcopenia: an aspect of cardiometabolic risk. Sci Rep. 2017;7:6491
Li D, Guo G, Xia L, Yang X, Zhang B, Liu F, et al. Relative handgrip strength is inversely associated with metabolic profile and metabolic disease in the general population in China. Front Physiol. 2018;9:59
Srikanthan P, Hevener AL, Karlamangla AS. Sarcopenia exacerbates obesity-associated insulin resistance and dysglycemia: findings from the National Health and Nutrition Examination Survey III. PLoS ONE. 2010;5:10805
Meex RCR, Watt MJ. Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance. Nat Rev Endocrinol. 2017;13:509–520
Mathews ST, Chellam N, Srinivas PR, Cintron VJ, Leon MA, Goustin AS, et al. Alpha2-HSG, a specific inhibitor of insulin receptor autophosphorylation, interacts with the insulin receptor. Mol Cell Endocrinol. 2000;164:87–98
Wu H-T, Ou H-Y, Hung H-C, Su Y-C, Lu F-H, Wu J-S, et al. A novel hepatokine, HFREP1, plays a crucial role in the development of insulin resistance and type 2 diabetes. Diabetologia. 2016;59:1732–1742
Valenti L, Bugianesi E, Pajvani U, Targher G. Nonalcoholic fatty liver disease: cause or consequence of type 2 diabetes? Liver Int. 2016;36:1563–1579
Acknowledgements
This study was supported by grant from the Korea Health Technology R&D Project through the Korean Health Industry Development Institute (KHIDI) funded by the Ministry of Health and Welfare of Korea (grant number: HI15C3153) and grant from the National Research Foundation of Korea (NRF) funded by the Ministry of Education of Korea (grant number: 2020R1I1A1A01070499) This work was also supported by Korea University Guro Hospital (Korea Research-Driven Hospital) and grant funded by Korea University Medicine (K2115701).
Author information
Authors and Affiliations
Contributions
ER, SYH, CWW and KMC participated in the design of the study. ER, JL, SJS, HJK, YSP, SL, BLC, HCJ, BJK, CWW and KMC contributed to data collection and quality control. SYH performed the statistical analysis. ER, HJY, SHB, CWW and KMC contributed to analysis and interpretation of data. ER, CWW and KMC wrote the paper. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
Eun Roh, Soon Young Hwang, Hye Jin Yoo, Sei Hyun Baik, Jin-Hee Lee, Sang Joon Son, Hyeon Ju Kim, Yong Soon Park, Sam-Gyu Lee, Be Long Cho, Hak Chul Jang, Bong Jo Kim, Miji Kim, Chang Won Won and Kyung Mook Choi have nothing to disclose.
Ethical approval
The study was performed according to the 1964 Declaration of Helsinki. The study protocol for the KFACS was approved by the Institutional Review Board of Korea University Guro Hospital (approval no. 2020GR0134).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roh, E., Hwang, S.Y., Yoo, H.J. et al. Impact of non-alcoholic fatty liver disease on the risk of sarcopenia: a nationwide multicenter prospective study. Hepatol Int 16, 545–554 (2022). https://doi.org/10.1007/s12072-021-10258-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-021-10258-8