Abstract
Rationale
Sex-related differences in the clinical profiles of some insomnia medications have been previously reported.
Objective
To evaluate the clinical profile of suvorexant, a novel orexin receptor antagonist approved for treating insomnia at doses up to 20 mg, by sex subgroups.
Methods
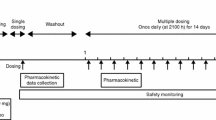
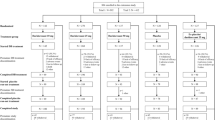
Efficacy analyses by sex were based on pooled data from two similar phase 3, randomized, double-blind, placebo-controlled, 3-month trials in elderly (≥65 years) and non-elderly (18–64 years) insomnia patients. Two age-adjusted (non-elderly/elderly) dose regimes of 40/30 and 20/15 mg were evaluated, with fewer patients assigned to 20/15 mg. Efficacy was assessed by patient-reported outcomes (N = 1264 women, 707 men) and by polysomnography endpoints in ~75% of patients. Safety analyses by sex (N = 1744 women, 1065 men) included pooled data from the two 3-month trials plus 3-month data from a safety trial of 40/30 mg.
Results
The sex subgroup efficacy analyses mirrored the improvements seen for suvorexant 40/30 and 20/15 mg over placebo on patient-reported outcomes and polysomnography sleep maintenance and onset endpoints in the primary analyses; 95% CIs excluded zero in favor of suvorexant for most endpoints in both sexes, and similar efficacy was observed between sexes (95% CIs overlapped). Suvorexant was well-tolerated in women and men, although women in all treatment groups (including placebo) reported more adverse events than men. The most frequent adverse event was somnolence (women: 11.1% for 40/30 mg, 8.5% for 20/15 mg, 2.3% for placebo; men: 10.1% for 40/30 mg, 3.4% for 20/15 mg, 4.2% for placebo).
Conclusion
Suvorexant was generally effective and well-tolerated in both women and men with insomnia.
ClinicalTrials.gov trial registration numbers: NCT01097616, NCT01097629, NCT01021813.

Similar content being viewed by others
References
American Psychiatric Association (2000) Diagnostic and statistical manual of mental disorders, 4th edn. American Psychiatric Association, Washington
Boivin DB, Shechter A, Boudreau P, Begum EA, Ng Ying-Kin NM (2016) Diurnal and circadian variation of sleep and alertness in men vs. naturally cycling women. Proc Natl Acad Sci U S A 113:10980–10985
Cosgrove KP, Mazure CM, Staley JK (2007) Evolving knowledge of sex differences in brain structure, function, and chemistry. Biol Psychiatry 62:847–855
Cox CD, Breslin MJ, Whitman DB, Schreier JD, McGaughey GB, Bogusky MJ, Roecker AJ, Mercer SP, Bednar RA, Lemaire W, Bruno JG, Reiss DR, Harrell CM, Murphy KL, Garson SL, Doran SM, Prueksaritanont T, Anderson WB, Tang C, Roller S, Cabalu TD, Cui D, Hartman GD, Young SD, Koblan KS, Winrow CJ, Renger JJ, Coleman PJ (2010) Discovery of the dual orexin receptor antagonist [(7R)-4-(5-chloro-1,3-benzoxazol-2-yl)-7-methyl-1,4-diazepan-1-yl][5-methyl-2-(2H −1,2,3-triazol-2-yl)phenyl]methanone (MK-4305) for the treatment of insomnia. J Med Chem 53:5320–5332
Dijk DJ, James LM, Peters S, Walsh JK, Deacon S (2010) Sex differences and the effect of gaboxadol and zolpidem on EEG power spectra in NREM and REM sleep. J Psychopharmacol 24:1613–1618
Farkas RH, Unger EF, Temple R (2013) Zolpidem and driving impairment—identifying persons at risk. N Engl J Med 369:689–691
Franconi F, Brunelleschi S, Steardo L, Cuomo V (2007) Gender differences in drug responses. Pharmacol Res 55:81–95
Gandhi M, Aweeka F, Greenblatt RM, Blaschke TF (2004) Sex differences in pharmacokinetics and pharmacodynamics. Annu Rev Pharmacol Toxicol 44:499–523
Herring WJ, Snyder E, Budd K, Hutzelmann J, Snavely D, Liu K, Lines C, Roth T, Michelson D (2012) Orexin receptor antagonism for treatment of insomnia: a randomized clinical trial of suvorexant. Neurology 79:2265–2274
Herring WJ, Connor KM, Ivgy-May N, Snyder E, Liu K, Snavely DB, Krystal AD, Walsh JK, Benca RM, Rosenberg R, Sangal RB, Budd K, Hutzelmann J, Leibensperger H, Froman S, Lines C, Roth T, Michelson D (2016) Suvorexant in patients with insomnia: results from two 3-month randomized controlled clinical trials. Biol Psychiatry 79:136–148
Jacobson R (2014) Psychotropic drugs affect men and women differently. Scientific American Mind July 1 2014. http://www.scientificamerican.com/article/psychotropic-drugs-affect-men-and-women-differently/ Accessed November 18, 2016.
Mallampalli MP, Carter CL (2014) Exploring sex and gender differences in sleep health: a Society for Women's Health Research report. J Women's Health (Larchmt) 23:553–562
Michelson D, Snyder E, Paradis E, Chengan-Liu M, Snavely DB, Hutzelmann J, Walsh JK, Krystal AD, Benca RM, Cohn M, Lines C, Roth T, Herring WJ (2014) Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 13:461–471
Mieda M, Sakurai T (2013) Orexin (hypocretin) receptor agonists and antagonists for treatment of sleep disorders. Rationale for development and current status. CNS Drugs 27:83–90
Mong JA, Baker FC, Mahoney MM, Paul KN, Schwartz MD, Semba K, Silver R (2011) Sleep, rhythms, and the endocrine brain: influence of sex and gonadal hormones. J Neurosci 31:16107–16116
Nowakowski S, Meers J, Heimbach E (2013) Sleep and women's health. Sleep Med Res 4:1–22
Roth T, Lines C, Vandormael K, Ceesay P, Anderson D, Snavely D (2010) Effect of gaboxadol on patient-reported measures of sleep and waking function in patients with primary insomnia: results from two randomized, controlled, 3-month studies. J Clin Sleep Med 6:30–39
Roehrs T, Roth T (2012) Insomnia pharmacotherapy. Neurotherapeutics 9:728–738
Sun H, Kennedy WP, Wilbraham D, Lewis N, Calder N, Li X, Ma J, Yee KL, Ermlich S, Mangin E, Lines C, Rosen L, Chodakewitz J, Murphy GM (2013) Effects of suvorexant, an orexin receptor antagonist, on sleep parameters as measured by polysomnography in healthy men. Sleep 36:259–267
Svetnik V, Snyder ES, Ma J, Tao P, Lines C, Herring WJ (2017) EEG spectral analysis of NREM sleep in a large sample of patients with insomnia and good sleepers: effects of age, sex and part of the night. J Sleep Res 26:92–104
Winrow CJ, Gotter AL, Cox CD, Doran SM, Tannenbaum PL, Breslin MJ, Garson SL, Fox SV, Harrell CM, Stevens J, Reiss DR, Cui D, Coleman PJ, Renger JJ (2011) Promotion of sleep by suvorexant-a novel dual orexin receptor antagonist. J Neurogenet 25:52–61
Winrow CJ, Renger JJ (2014) Discovery and development of orexin receptor antagonists as therapeutics for insomnia. Br J Pharmacol 171:283–293
Zhang B, Wing YK (2006) Sex differences in insomnia: a meta-analysis. Sleep 29:85–93
Zopf Y, Rabe C, Neubert A, Gassmann KG, Rascher W, Hahn EG, Brune K, Dormann H (2008) Women encounter ADRs more often than do men. Eur J Clin Pharmacol 64:999–1004
Acknowledgements
These studies were funded by Merck & Co., Inc., Kenilworth, NJ, USA. Mingqui Wu, formerly from Merck & Co., Inc., contributed to the statistical analysis. Sheila Erespe from Merck & Co., Inc. assisted with the submission.
Contributors
WJH was involved in study concept and design, interpretation of data, and drafting of manuscript. KMC, DBS, YZ, RMB, ADK, JKW, TR, and DM were involved in study concept and design and interpretation of data. JH was involved in study concept and design and acquisition of data. ES was involved in study concept and design, analysis and interpretation of data, and drafting of manuscript. DM-W was involved in interpretation of data. CL was involved in interpretation of data and drafting of manuscript. All authors reviewed and/or revised the manuscript for intellectual content and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The trials were conducted in accordance with principles of Good Clinical Practice and were approved by the appropriate institutional review boards and regulatory agencies for each site. Informed consent was obtained from all patients. The trials were registered at ClinicalTrials.gov (NCT01097616, NCT01097629, NCT01021813).
Conflict of interests
WJH, KMC, ES, DBS, YZ, JH, DM-W, CL, and DM are current or former employees of Merck Sharp & Dohme Corp., a subsidiary of Merck & Co., Inc., Kenilworth, NJ USA and own or owned stock/stock options in the Company.
RMB has served as a consultant to and receives research support from Merck & Co., Inc., and has served as a consultant to Janssen and Jazz over the past 2 years.
ADK has received grants/research support from NIH, Teva, Sunovion, Astellas, Abbott, Neosync, Brainsway, Janssen, ANS St. Jude, Novartis. He has served as a consultant to Abbott, Astellas, AstraZeneca, Attentiv, BMS, Teva, Eisai, Eli Lilly, GlaxoSmithKline, Jazz, Janssen, Merck, Neurocrine, Novartis, Otsuka, Lundbeck, Roche, Sanofi-Aventis, Somnus, Sunovion, Somaxon, Takeda, Transcept, Vantia.
JKW has received research support from the following in the past 2 years: Apnex, Merck & Co., Inc., Novo Nordisk, Respironics, Vanda, and has provided consulting services to Merck & Co., Inc., Somnus, Transcept, Vanda, Ventus, and Vivus.
TR has received grants/research support from Aventis, Cephalon, GlaxoSmithKline, Neurocrine, Pfizer, Sanofi, Schering-Plough, Sepracor, Somaxon, Syrex, Takeda, TransOral, Wyeth and Xenoport; has acted as a consultant for Abbott, Acadia, Acoglix, Actelion, Alchemers, Alza, Ancil, Arena, AstraZeneca, Aventis, AVER, BMS, BTG, Cephalon, Cypress, Dove, Elan, Eli Lilly, Evotec, Forest, GlaxoSmithKline, Hypnion, Impax, Intec, Intra-Cellular, Jazz, Johnson–Johnson, King, Lundbeck, McNeil, MediciNova, Merck & Co., Inc., Neurim, Neurocrine, Neurogen, Novartis, Orexo, Organon, Prestwick, Procter–Gamble, Pfizer, Purdue, Resteva, Roche, Sanofi, Schering-Plough, Sepracor, Servier, Shire, Somaxon, Syrex, Takeda, TransOral, Vanda, Vivometrics, Wyeth, Yamanuchi, and Xenoport; and has participated in speaking engagements supported by Cephalon, Sanofi, and Takeda.
Funding
The studies were funded by Merck & Co., Inc., Kenilworth, NJ, USA. A Scientific Advisory Committee comprised Merck and non-Merck investigators contributed to the development of the protocols, statistical analysis plans, analysis and interpretation of data, served as authors of the manuscript and was responsible for the decision to submit the manuscript for publication. The funding organization was involved in the design and conduct of the studies, the collection, management, analysis, interpretation of data, and preparation, review, and approval of the manuscript.
Rights and permissions
About this article
Cite this article
Herring, W., Connor, K.M., Snyder, E. et al. Clinical profile of suvorexant for the treatment of insomnia over 3 months in women and men: subgroup analysis of pooled phase-3 data. Psychopharmacology 234, 1703–1711 (2017). https://doi.org/10.1007/s00213-017-4573-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-017-4573-1