Abstract
Aflatoxins (AFs), ochratoxin A (OTA), citrinin (CIT), fumonisin B1 (FB1), zearalenone (ZEN), and deoxynivalenol (DON) are mycotoxins that may contaminate diets, especially in low-income settings, with potentially severe health consequences. This study investigates the exposure of 439 pregnant women in rural Bangladesh to 35 mycotoxins and their corresponding health risks and links their exposure to certain foods and local stimulants. Overall, 447 first-morning urine samples were collected from pregnant women between July 2018 and November 2019. Mycotoxin biomarkers were quantified by DaS-HPLC–MS/MS. Urinary concentration of frequently occurring mycotoxins was used to estimate dietary mycotoxin exposure. Median regression analyses were performed to investigate the association between the consumption of certain foods and local stimulants, and urinary concentration of frequently occurring mycotoxins. Only in 17 of 447 urine samples (4%) were none of the investigated mycotoxins detected. Biomarkers for six major mycotoxins (AFs, CIT, DON, FB1, OTA, and ZEN) were detected in the urine samples. OTA (95%), CIT (61%), and DON (6%) were most frequently detected, with multiple mycotoxins co-occurring in 281/447 (63%) of urine samples. Under the lowest exposure scenario, dietary exposure to OTA, CIT, and DON was of public health concern in 95%, 16%, and 1% of the pregnant women, respectively. Consumption of specific foods and local stimulants—betel nut, betel leaf, and chewing tobacco—were associated with OTA, CIT, and DON urine levels. In conclusion, exposure to multiple mycotoxins during early pregnancy is widespread in this rural community and represents a potential health risk for mothers and their offspring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mycotoxins are natural toxins produced as secondary metabolites of micro-fungi under certain environmental and crop conditions; they are harmful to humans and animals even in low concentrations (Bennett and Klich 2003; Bhatnagar et al. 2002). Mycotoxins contaminate a substantial proportion of a variety of dietary staples and other food crops worldwide (Eskola et al. 2020). Due to their resistance to standard food processing and cooking practices, mycotoxins remain an important dietary contaminant, especially in low-income countries (IARC 2015), with potentially serious health consequences (Marin et al. 2013; Turner et al. 2012).
Human exposure to mycotoxins can either be assessed through environmental monitoring or biological monitoring (biomonitoring). Environmental monitoring involves directly measuring mycotoxin levels in food, feed, and/or air. However, representative mycotoxin contamination data from food are difficult to obtain due to the high degree of heterogeneity of food, the possible presence of modified forms of mycotoxins (Rychlik et al. 2014) and, in many regions, the challenges in sampling foods produced by subsistence farmers (IARC 2015). On the other hand, biomonitoring involves detecting mycotoxins, mycotoxin metabolites, and adducts (referred to as biomarkers) in tissues, body fluids, and excreta. Current state-of-the-art biomarker analysis methods enable relatively easy and objective detection and quantification of major mycotoxins from bio-samples (Escrivá et al. 2017; Ezekiel et al. 2022; Šarkanj et al. 2018). Examples of major mycotoxins investigated include aflatoxins (AFs), fumonisin B1 (FB1), ochratoxin A (OTA), citrinin (CIT), zearalenone (ZEN), and deoxynivalenol (DON) (Al-Jaal et al. 2019; Gerding et al. 2015, 2014; Schmidt et al. 2021a, 2021b; Solfrizzo et al. 2014; Warth et al. 2014). Biomonitoring of exposure biomarkers is also considered advantageous, as it provides information on the internal dose of exposure via all routes, including dietary intake and exposures via the respiratory tract and the skin (Degen 2011; Fromme et al. 2016). Moreover, biomonitoring is particularly valuable in low-income settings, such as Bangladesh, where regular food contamination surveillance is scarce or non-existent (Islam and Hoque 2013).
Human biomonitoring studies from several countries demonstrate widespread exposure to major mycotoxins during pregnancy (Abdulrazzaq et al. 2002; Chan-Hon-Tong et al. 2013; Groopman et al. 2014; Jonsyn et al. 1995; Lei et al. 2013). There is also evidence of transplacental transfer of mycotoxins such as AFs, OTA, CIT, DON, and ZEN to the developing fetus in humans and animals (Goyarts et al. 2007; Nielsen et al. 2011; Partanen et al. 2010; Reddy et al. 1982; Warth et al. 2019; Woo et al. 2012). This suggests a potentially harmful exposure during the critical first 1000 days of a child's life (Groopman et al. 2014; Ismail et al. 2021), with some evidence of adverse effects on newborn and child health (Andrews-Trevino et al. 2021, 2019; Kyei et al. 2020; Sherif et al. 2009).
Bangladesh has a tropical monsoon climate, characterized by seasonal variations in rainfall, high temperatures, and high humidity, conducive for mold contamination of food crops and subsequent mycotoxin production. An environmental monitoring study in the early 1990s assessed the extent of mycotoxin contamination of Bangladeshi food groups, including cereals, nuts, and pulses, in four districts (Chittagong, Dhaka, Rajshahi, and Khulna). In that study, varying contamination levels of major mycotoxins were detected in food samples, including AFs, FB1, DON, OTA, and ZEN (Dawlatana et al. 2002). Similarly, in a more recent market study, eight common Bangladeshi foods, including rice, wheat flour, lentils, groundnut, and spices, as well as betelnut were sampled from three cities: Dhaka, Chittagong, and Sirajganj, and analyzed for aflatoxin contamination. In that study, high levels of aflatoxins were detected in dates, groundnut, betelnut, and red chili powder (Roy et al. 2013). A very recent study reported the presence of aflatoxin M1 (AFM1) in dairy milk and milk products collected in four major divisions in Bangladesh (Sumon et al. 2021).
Consistent with these limited environmental monitoring studies, the results from biomonitoring studies in Bangladesh also suggest dietary exposure to mycotoxins for different population groups. For example, several biomonitoring studies analyzing urine samples from adults in rural and urban areas in the Rajshahi district reported the frequent occurrence of major mycotoxins such as AFM1, OTA, CIT, ZEN, and DON (Ali et al. 2015b, 2016a, b, d, 2017; Ali and Degen 2019). Studies analyzing urine samples from pregnant women in Dhaka district also reported the frequent occurrence of AFM1, OTA, CIT, and DON (Ali et al. 2015a, 2016c, 2017). Two other recent studies that analyzed urine samples from young children in Rajshahi and Dhaka districts also report a frequent occurrence of AFM1, DON, OTA, and CIT (Ali and Degen 2020; Ali et al. 2020). Furthermore, a recent study indicated the presence of AFM1 in about half of breast milk samples in Sylhet division (Islam et al. 2021).
Most biomonitoring studies have focused on characterizing individual mycotoxin occurrences rather than characterizing concurrent exposures to multiple mycotoxins. However, with molds requiring similar toxin production conditions and different mold species contaminating a food sample, concurrent exposure to multiple mycotoxins is likely to occur in reality (Frisvad et al. 2011; Turner et al. 2012; Vidal et al. 2018). Consequently, to improve the understanding of the mechanisms behind the association between maternal exposures to mycotoxins and adverse pregnancy outcomes in a population, there is a need to determine and describe the extent of simultaneous exposure of pregnant women to different mycotoxins.
Our study was conducted amongst a cohort of pregnant women in rural Habiganj district, Sylhet division, Bangladesh, where no previous environmental or biomonitoring studies for mycotoxins have been reported. The study aims to: (i) describe the occurrence and types of mycotoxin exposure of pregnant women in rural Bangladesh, (ii) estimate the probable daily intake (PDI) levels of frequently occurring mycotoxins and estimate dietary exposure of public health concern, and (iii) explore possible associations between the consumption of common Bangladeshi foods and stimulants and urinary concentrations of frequently detected mycotoxins.
Materials and methods
Study population and design
The Food and Agricultural Approaches to Reducing Malnutrition (FAARM) cluster-randomized controlled trial was conducted in two sub-districts of Habiganj district in Bangladesh’s Sylhet division (ClinicalTrials.gov ID: NCT02505711). FAARM included 2700 young married women, with self-reported age below 30 years, in 96 settlements (geographic clusters) who reported an interest in gardening and had access to at least 40 m2 of land. Settlements were randomized into 48 intervention and 48 control clusters. The FAARM trial evaluates the impact of a homestead food production program, implemented by the international non-governmental organization Helen Keller International, on undernutrition in young children. Further information on the FAARM trial design is available in the study protocol (Wendt et al. 2019).
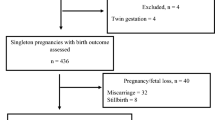
As an add-on to the FAARM trial, we conducted a prospective cohort study: Maternal Exposure to Mycotoxins and Adverse Pregnancy Outcomes (MEMAPO). MEMAPO enrolled a subsample of pregnant FAARM women—recruited early in pregnancy, of which 439 were followed up until the end of pregnancy—to investigate the role of maternal exposure to mycotoxins for the development of specific adverse pregnancy outcomes.
Urine sample collection and processing
We obtained 447 urine samples from 439 pregnant women (8 women with two pregnancies) who consented to participate in the MEMAPO study. About 10 ml of first-morning urine sample was collected into a sterile disposable container from each study participant before consuming food and water that day. The urine samples were collected between July 2018 and November 2019. They were transported to the project field laboratory in a cold box, aliquoted into 2 ml safe-seal tubes, and stored at – 20 °C on the same day of urine pick-up. All samples were subsequently sent to Germany on dry ice (transport time < 24 h) and stored at – 70 °C at Heidelberg University. Samples were later transported on dry ice to Münster University, Germany (transport time < 6 h) and stored at – 80 °C until biomarker analysis.
Background characteristics of study participants
Data on descriptive characteristics, such as a woman’s religion, her highest level of education, and her height, were extracted from the FAARM baseline and endline surveys conducted in 2014 and 2019, respectively. Using the FAARM endline survey's asset module, the household’s relative position within the 2014 Demographic and Health Survey (DHS) national wealth quintiles was calculated using the Equity Tool (NIPORT et al. 2016; Metrics for Management 2016). Data on other quantitative descriptive characteristics, such as gestational age in weeks and current weight, were extracted from the FAARM routine surveillance round at the time when the woman was enrolled in MEMAPO. The woman’s age at pregnancy enrollment was computed from her age at the FAARM baseline survey.
Food consumption data
FAARM’s routine surveillance system collects information on women’s dietary diversity, using a 21-food group questionnaire which can be collapsed into ten food groups according to recommended guidelines (FAO and FHI 360 2016). Briefly, women are asked about the food they consumed the previous 24-h day through an open recall followed by list-based probes. When women reported consuming a food item, they were then asked if they had consumed more or less than a spoonful to assess whether they had consumed at least 15 g of the food item throughout the day. Responses are aggregated into food groups, including starches (e.g., grains and white roots or tubers), pulses, nuts and seeds, dairy, flesh foods (e.g., meat, poultry, and game), fish, organ meats, eggs, dark green leafy vegetables, vitamin A-rich fruits and vegetables, other fruits, other vegetables, and sugary foods (sugar, honey, juice, chocolates, etc.). In the FAARM surveys, women were also asked about their intake of common local stimulants such as betelnut, betel leaf (locally called Paan), and chewing tobacco (locally called Jorda) in the past month.
Urine analysis
Urine creatinine and urine density analysis
Standard routine urine analyses were performed in the accredited central laboratory of Heidelberg University Hospital. Routine urine status parameters including specific gravity were assessed via multi-parameter urine test strips (#10,634,643, Siemens Healthcare GmbH, Erlangen, Germany) on a Siemens CLINITEK Novus® analyzer according to the manufacturer’s instructions. Urine creatinine concentrations were quantified on a Siemens ADVIA XPT chemistry analyzer (Siemens kit #03,039,070).
Mycotoxin analysis in spot urine
Mycotoxin biomarkers in urine were quantified by a validated “dilute and shoot” method using high-performance liquid chromatography–tandem mass spectrometry detection (DaS-HPLC–MS/MS), according to Gerding et al. (2014). This method was extended to include 12 additional analytes, so that urine samples were screened for 35 biomarkers in a chromatographic run time of 13 min. Instrumental limits of all analytes in urine were determined in a range of 0.01 to 30 ng/ml for the limit of detection (LOD) and 0.03 to 100 ng/ml for the limit of quantification (LOQ) (Table 1).
Statistical analysis
Management of left censoring and descriptive analysis
Left-censored urine mycotoxin data, i.e., concentrations below the LOD and LOQ of the analytical method, were imputed using the substitution methods as recommended in the European Food Safety Authority (EFSA) guidelines (EFSA 2010). Following EFSA guidelines, three substitution scenarios were estimated, lower bound (LB), middle bound (MB), and upper bound (UB). Specifically, results below LOD were substituted with the value of zero, LOD/2, and LOD under LB, MB, and UB scenarios, respectively. Likewise, results below LOQ were substituted with the value of LOD, LOQ/2, and LOQ under LB, MB, and UB scenarios, respectively. To adjust for inter-individual variation in urine volume, urine mycotoxin concentrations were corrected for urine density and urine creatinine before dietary exposure estimation. Descriptive statistics, including mean urine concentration of mycotoxins, standard deviation, and concentration range, were thus calculated for all substitution scenarios, corrected for urine density and creatinine concentration (Supplementary Table S1). Although urine density-corrected concentrations are preferred (Carrieri et al. 2001; Suwazono et al. 2005), both an adjustment for density and for creatinine are presented for easy comparison with previous studies using either method. For density correction, the formula provided by Smith et al. (2012) was adopted:
where C(cor) is the adjusted concentration in ng/ml, C(obs) is the observed unadjusted concentration in ng/ml, 1.0104 is the average urine density in our dataset (n = 447), and ρ is the specific density in each urine sample.
Estimation of dietary mycotoxin exposure
Dietary exposure assessments were performed by estimating probable daily intake (PDI) for the frequently occurring mycotoxins (OTA, CIT, DON, and AFM1) in this population. For DON and CIT, where both parent compounds and metabolites were detected, exposure assessment calculations were performed on total DON (DON + DON-15GlcA + DON-3GlcA) and total CIT (CIT + Dihydrocitrinone (HO-CIT)) by converting metabolites using their molar mass. The urinary mycotoxin concentrations were used to calculate a probable daily intake (PDI) in ng/kg body weight (bw) for each individual using this formula (Solfrizzo et al. 2014):
where C is the mycotoxin concentration, adjusted for urine density or creatinine, W is the individual's body weight (kg), E is the excretion rate (%) of the mycotoxin, and V is the daily urine excretion volume (ml). A mean daily urine output during pregnancy of 2000 ml was used based on literature (Mikhail and Anyaegbunam 1995). The urinary excretion rate of DON used for the calculation was 68% (Warth et al. 2013), a value used in previous studies in Bangladesh (Ali et al. 2015a, 2016b; Gerding et al. 2015). For CIT, an excretion rate of 40.2% was used (Degen et al. 2018), while an excretion rate of 1.5% was used for AFM1 (Zhu et al. 1987). An excretion rate of 2.6% was adopted for OTA, based on a recent pig study (Gambacorta et al. 2019). This value is close to what was estimated from a human kinetic study (Degen 2015; Studer-Rohr et al. 2000). PDIs for the mean population mycotoxin concentrations were calculated for the LB, MB, and UB substitution scenarios.
Health risk characterization
Two different approaches were used for risk assessment of individual mycotoxins based on their toxicity profiles. Considering the carcinogenicity of OTA and AFB1, no level of exposure is considered safe. The Margin of Exposure (MOE) was thus calculated for these mycotoxins to help prioritize risk management actions. MOE was computed as a ratio of benchmark dose lower confidence limit (BMDL10) and women's exposure (estimated by PDI). The scientific committee of EFSA and the WHO consider a MOE of 10,000 or more to be of low concern for public health (EFSA 2013). BMDL10 values for aflatoxins of 0.4 µg/kg bw/day (EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain) et al. 2020b) and for OTA with neoplastic effects at 14.5 µg/kg bw/day (EFSA CONTAM Panel (EFSA Panel on Contaminants in the Food Chain) et al. 2020a) were used for MOE estimations. For the other mycotoxins, the estimated PDIs were compared with established health-based guidance values to calculate a hazard quotient (HQ), i.e., the proportion of the population who consume these mycotoxins above established tolerable daily intake (TDI) levels. The TDI values for CIT of 200 ng/kg bw/day and for DON of 1000 ng/kg bw/day were those derived by scientific committees, such as the Joint FAO/WHO Expert Committee on Food Additives (JECFA) and the EFSA (EFSA 2012, 2017; FAO/WHO 2011). When the HQ was less than one, the exposure was considered to be within safe limits.
Assessment of the relationship between food consumption and urinary mycotoxin concentrations
Shapiro–Wilk’s test was used to assess normality of the raw and log-transformed urine concentration data for OTA, DON, CIT. There was strong evidence (p-values < 0.001) that the data, except for the log-transformed OTA concentration (p = 0.14), deviated from a normal distribution. Furthermore, household characteristics such as wealth did not appear to be associated with urinary mycotoxin concentration in our data. Also, an a priori model with wealth did not improve model fit significantly. Thus, crude bivariable median regression analyses were performed to investigate the direction of association between mycotoxin biomarker concentrations (OTA, total DON, and total CIT) and the consumption of typical Bangladeshi foods, as consumed by the women around the time of enrollment and reported in Table 5, and stimulants, including betel nut and betel leaf. We used foods from 19 out of the 21 dietary diversity food groups, leaving out the groups of other fruits and other vegetables. All median regression models used bootstrapping over 1000 replications to produce robust estimates. Analyses were performed in Stata 14.2 (Stata Corporation, College Station, TX, USA).
Results
Description of the study population
Of the cohort of 439 women recruited for the MEMAPO study, 8 had two pregnancy events during the study period, resulting in 447 pregnancy observations. The background characteristics of the enrolled pregnant women are presented in Table 2. Three-quarters were Muslim, and one-quarter were Hindu. Almost 80% came from households belonging to the middle and upper wealth quintiles of the 2014 Bangladesh Demographic and Health Survey wealth index (NIPORT et al. 2016), while a tenth belonged to the wealthiest quintile and another tenth to the lower two wealth quintiles. On average, women had been married in their late teens and were in their late twenties at the time of enrollment into this study. Only 6% of women had completed secondary school or higher degrees, while 14% had no formal education. On average, the women weighed 47 kg and were enrolled at around 15 weeks of gestation.
Occurrence of mycotoxin biomarkers in urine
Out of the 35 different urinary mycotoxin biomarkers investigated, ten different biomarkers were detected, representing six major mycotoxins: AF, CIT, DON, FB1, OTA, and ZEN (Table 3). Only 17 urine samples (4%) were free from all the investigated mycotoxin biomarkers. About a third of the urine samples each contained one, two, and three detectable mycotoxin biomarkers (Fig. 1a). More than half (58%) of the urine samples had two different detectable mycotoxins, 5% had even three detectable mycotoxins, while a third had only one detectable mycotoxin (Fig. 1b). The occurrence and uncorrected concentration of the ten detected mycotoxin biomarkers, along with their limits of detection (LOD) and quantification (LOQ) of the method, are summarized in Table 3. OTA was the most frequently occurring mycotoxin detected in 95% of the samples, with 77% of the samples detected above the LOQ of the method. The urinary metabolite of OTA, ochratoxin α (OTα), was not detected in any sample.
Number of detected biomarkers and mycotoxins in urine samples of pregnant women in rural Bangladesh (n = 447). Only in 17 urine samples (4%) none of the investigated mycotoxins were detected. About a third of the urine samples contained one, a third two, and another third three detectable mycotoxin biomarkers. Only 2% contained more than three. (Figure 1a). This corresponds to two different mycotoxins detected in over half and three in 5% of the samples, while a third of samples contained one detectable mycotoxin. (Figure 1b). tCIT- total CIT (CIT+ HO-CIT); tDON- total DON (DON + DON-Glucuronides); tAF- total aflatoxins (AFM1+AFB2)
The next most frequently occurring mycotoxin was CIT and its metabolite HO-CIT, detected in 41% and 51% of the samples, respectively. DON and its DON-Glucuronide metabolites were detectable in 6% of samples, with no detection of de-epoxy-deoxynivalenol (DOM-1), another urinary metabolite of DON. Aflatoxins (AFB2 and AFM1) were detected in less than 2% of samples. The occurrence of different combinations of mycotoxins in the urine of pregnant women is shown in Fig. 2. Co-occurrence of OTA and CIT was the prevailing mycotoxin exposure, present amongst more than half of pregnant women (55%). About a third were exposed to OTA alone, while another 6% were exposed to CIT alone. The seven remaining detected mycotoxins always co-occurred jointly with the more frequently detected mycotoxins.
Mycotoxin combinations and their occurrence in urine samples of pregnant women in rural Bangladesh (n = 447). Biomarkers for six major mycotoxins (AFs, CIT, DON, FB1, OTA, and ZEN) were detected in the urine samples. Co-occurrence of multiple mycotoxins was detected in 281/447 (63%) of urine samples. Co-occurrence of OTA and CIT was the prevailing co-exposure (55%)
Dietary mycotoxin exposure and health risk assessment
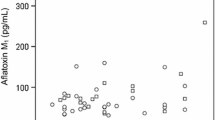
The probable daily intake (PDI) of the three most commonly detected mycotoxins, OTA, total CIT, and total DON calculated from urine mycotoxin concentration, corrected for urine density and creatinine, and estimated for LB, MB, and UB scenarios are presented in Table 4. The estimated mean dietary exposure to OTA in the study population ranged from 400 ng/kg bw under the LB scenario to 426 ng/kg bw under the UB scenario. The maximum estimated PDI for OTA was 3968 ng/kg bw and 8070 ng/kg bw when using density-adjusted and creatinine-adjusted data. Even under the LB scenario, the Margin of Exposure (MOE) values of OTA were lower than 1000 in nearly all samples (95%), indicating a high health concern for this mycotoxin (Fig. 3).
Margin of Exposure of pregnant women to dietary ochratoxin A under the lowest exposure scenario (n = 447). The Margin of Exposure (MOE) is calculated by dividing the benchmark dose lower confidence limit (BMDL10) for ochratoxin A (OTA; 14.5 µg/kg body weight/day) by the woman's exposure which is estimated by probable daily intake (PDI). The red line shows a MOE of 10,000. If the MOE is below 10,000, the exposure could be of health concern. Dietary exposure to OTA is below this line in 95% of pregnant women in our sample
The mean PDI of total CIT amongst the pregnant women using density-adjusted data ranged from 116 ng/kg bw (LB scenario) to 152 ng/kg bw (UB scenario). Compared to the established health guidance level of no concern for nephrotoxicity below 200 ng/kg bw (EFSA 2012), the exposure of 17% of the pregnant women under the MB scenario was of public health concern (Fig. 4). The proportion of pregnant women with an estimated mean dietary intake of CIT exceeding this health reference value ranged from 16% (LB scenario) to 19% (UB scenario). Using creatinine-adjusted data, the proportion of pregnant women with average intake above the health-based guidance value ranges between 25% (LB scenario) and 33% (UB scenario).
Hazard quotient of dietary exposure of pregnant women to citrinin (n = 447) under a moderate exposure scenario. The Hazard quotient (HQ) is calculated by dividing individual exposure, measured by probable daily intake (PDI) by the established tolerable daily intake (TDI) level for citrinin (CIT; 200 ng/kg body weight/day). The red line shows a HQ of 1. If the HQ is above 1, the exposure could be of health concern. The exposure of 17% of the pregnant women in our sample is of public health concern
The mean PDI of total DON exceeded the group tolerable daily intake (TDI) for DON (EFSA 2017; FAO/WHO 2011) of 1000 ng/kg bw in approximately 1% (n = 3, density-adjusted, and n = 2, creatinine-adjusted data) of the participants under the LB scenario. The proportion of women with PDIs exceeding the health-based guidance value increases to 4% (n = 20, density-adjusted data) and 24% (n = 107, creatinine-adjusted data) under the UB scenario. The maximum estimated individual PDI for total DON ranges from 4943 ng/kg bw (LB scenario) to 4992 ng/kg bw (UB scenario). The corresponding maximum intake of total DON using creatinine-adjusted data ranges from 5359 ng/kg bw (LB scenario) to 16,123 ng/kg bw (UB scenario). Thus, these maximum intake values range between more than 50% to twice the acute reference dose (ARfD) of 8000 ng/kg bw established by the EFSA.
Relationship between food consumption and mycotoxin concentration in urine
Out of the 447 individual pregnancy events, four women had missing information on their food consumption around the time of recruitment. Hence, 443 pregnancy events with food consumption were used in this analysis. The number of women who consumed the specific food groups along with results of median regression analyses evaluating the direction of crude associations between concentrations of OTA, total CIT, and total DON in urine under the MB scenario and the consumption of specific Bangladeshi foods, including local stimulants, are shown in Table 5. All women consumed starchy staples such as grains and white roots in similar amounts. Consequently, their effect on urinary mycotoxin concentration could not be analyzed. Foods that pregnant women commonly consumed in the previous day included spices and condiments (99%), oils and fats (99%), small fish (69%), sugary foods (66%), and hot beverages like tea (52%). Less commonly consumed foods by pregnant women included nuts and seeds (9%), beans and peas (31%), and dark green leafy vegetables (32%). The consumption of local stimulants (betel nut/leaf and many chewing tobacco) by pregnant women in the past month was high.
The regression models showed significant positive associations between urine OTA concentration and intake of more than 15 g of nuts (p < 0.0001) and the intake of the following local stimulants in the past month: betel leaf (Paan) (p = 0.03), betel nut and betel leaf (p = 0.04), and chewing tobacco(Jorda) (p = 0.01). There were also significant negative associations between urine OTA concentration and intake of more than 15 g of eggs (p = 0.03), large fish or seafood (p = 0.04), sugary foods (p = 0.01), and tea or coffee (p = 0.01). In the study region, tea is consumed much more frequently than coffee.
Apart from the intake of small animal protein, which was negatively associated with total CIT concentration in urine (p = 0.02), none of the other food items was significantly associated with urinary CIT concentration. In contrast, intake of any of the following local stimulants was associated with an increase in urinary CIT levels: betel leaf (Paan) (p = 0.001), betel nut (p = 0.03), Paan and betel nut (p = 0.01), and chewing tobacco (Jorda) (p = 0.02).
Likewise, of all food items, only the intake of vitamin A-rich vegetables appeared to increase total DON levels in urine (p = 0.04) significantly, while intake of betel nut (p = 0.04) and chewing tobacco (p < 0.0001) were associated with a significant increase in total DON levels.
Discussion
The finding that only 17 of 447 urine samples (4%) were free from all investigated mycotoxin biomarkers (Table 2) clearly indicates a widespread exposure of pregnant women in this rural community of Bangladesh to mycotoxins. We detected similar mycotoxins as other biomonitoring studies conducted among pregnant women in the Dhaka district (Ali et al. 2015a, 2016c, 2017). However, this is the first study that determines concurrent multiple mycotoxin exposure among pregnant women in Bangladesh. The results establish that concurrent exposure to multiple mycotoxins (63% of samples) represents this population's prevailing exposure pattern (Figs. 1 and 2). This finding is not surprising considering that different mold species may contaminate a given food sample and that molds require similar conditions for toxin production (Frisvad et al. 2006).
OTA and CIT are the most frequently occurring mycotoxins in this population. A previous biomonitoring study among urban and rural residents in the Rajshahi district of Bangladesh revealed an equally high occurrence of both OTA and CIT biomarkers (> 60%) (Ali et al. 2016a). These are two major hazardous mycotoxins produced mainly by certain Aspergillus and Penicillium species, frequently contaminating foods and feed under poor post-harvest handling and storage conditions (Alshannaq and Yu 2017; Frisvad et al. 2006). Poor transportation practices, improper drying, improper shelling, poor curing techniques, bare floor storage, and very humid storage conditions are some of the post-harvest and storage conditions that facilitate storage mold contamination and mycotoxin production (Codex Alimentarius 2016). In Bangladesh, rice harvested in one season is usually stored and consumed until a new harvest becomes available.
The results on multi-mycotoxin biomarker analysis indicate a relatively low exposure of the study population to DON (6%), FB1 (< 1%), and ZEN (< 1%), toxins produced mainly by Fusarium species which contaminate crops such as maize, wheat, and barley in the field (Alshannaq and Yu 2017; Frisvad et al. 2006). However, it must be considered that the limited sensitivity of the analytical method resulted in an overall low number of detects. Repeated cultivation, late planting, poor field hygiene, heavy planting density, and poor water management are some of the pre-harvest or field conditions that may favor mycotoxin contamination (Codex Alimentarius 2016). In a previous biomonitoring survey among 54 pregnant women in the Dhaka district of Bangladesh, no DOM-1 was detected either. At the same time, 52% of the samples were positive for DON (Ali et al. 2015a), which can be explained by the better sensitivity of the immunoaffinity column (IAC)-based single analyte method used by Ali et al. 2015a. Apart from that, the difference in DON occurrence levels may be partly related to different levels of food contamination and food habits in the two study areas. Although DON has previously been detected at moderate levels in maize samples in Bangladesh (Dawlatana et al. 2002), maize is not an important staple in the study area. In general, the low occurrence rates for DON and other trichothecenes in Bangladesh, compared to studies elsewhere (Ali et al. 2016b; Gerding et al. 2015; Warensjö Lemming et al. 2020), are in good agreement with the Bangladeshi nutritional habits of low wheat and maize consumption. Due to the low occurrence of DON in Bangladesh, the applied management of left-censored data according to EFSA might lead to an overestimation of DON exposure, especially in the UB scenario.
In general, our mycotoxin occurrence results are consistent with the results of an earlier comparative study of urinary mycotoxin occurrence patterns (Gerding et al. 2015), which found that 83 of 95 (87%) samples from adult Bangladeshi volunteers were positive for mycotoxin biomarkers, compared to 80% of samples from Germany and 68% from Haiti. Overall, the urines from Bangladesh had high detection rates for OTA and CIT metabolites, while AFM1 and FB1 were only occasionally detected, and DON and its metabolites were absent from Bangladeshi samples. Apart from food habits, poor agricultural practices contribute to mold contamination of crops and subsequent mycotoxin production. Thus, the frequent high detection of OTA and CIT in this rural community likely indicates a lack of proper post-harvest and storage practices among households. Not surprisingly, a recent survey among the rural households, to which the pregnant women in our study belong, confirmed generally insufficient knowledge of the conditions that favor mold contamination of crops and the measures for prevention at all stages of crop production and storage (Kyei et al. 2021). This lack of knowledge likely contributed to contamination and the frequent detection of mycotoxins in the investigated urine samples.
Estimating the mean probable dietary intake from the concentrations of the most frequently occurring urinary mycotoxins among the pregnant women in our study, we found the values for OTA up to 25 times higher than the previous health-based guidance value of 17.1 ng/kg bw (EFSA 2006). However, in their recent opinion on OTA, the EFSA concluded that based on new data, it is inappropriate to establish a health-based guidance value, and a margin of exposure approach was applied (EFSA 2020). For this reason, MOE values were also calculated, and the vast majority of samples had MOE values far below 10,000 (Fig. 3), indicating a high health concern for the carcinogenic effects of OTA in this population. We also compared the mean estimated probable dietary intake for CIT under various substitution scenarios to the established health guidance level of no concern for nephrotoxicity (200 ng/kg bw) (EFSA 2012) and found that between a fifth and a third of the pregnant women had a dietary intake of CIT at levels of public health concern. Given experimental evidence of transplacental transfer of mycotoxins such as AF, OTA, CIT, DON, and ZEN to the developing fetus (Goyarts et al. 2007; Nielsen et al. 2011; Partanen et al. 2010; Reddy et al. 1982; Warth et al. 2019; Woo et al. 2012), exposure of pregnant women to these mycotoxins also represents a potential risk to maternal, fetal and child health, requiring further investigations to ascertain associations and mechanisms.
When examining possible dietary sources of the most frequently occurring mycotoxins using regression models, we found that intake of certain foods and local stimulants (betel nut, betel leaf, and chewing tobacco) was associated with urinary mycotoxin biomarker concentrations (Table 4). For example, intake of nuts and seeds (mainly groundnuts in our study area) and local stimulants was associated with higher urinary OTA concentration, while intake of eggs, large fish, or other seafood, but also of sugary foods and tea was associated with lower OTA concentrations. While associations point to certain foods/stimulants that may be contaminated, the proportion of women consuming such foods/stimulants determines whether that consumption can explain the detected mycotoxin occurrence in urine. For example, although we found that nut consumption was positively associated with urinary OTA levels, less than 10% of women consumed 15 g of nuts or seeds in the past day, which suggests this cannot be the primary dietary source. Local stimulant consumption was associated with higher urinary concentrations of OTA, CIT, and DON, and the majority of women took betel nut or leaf, and many women took chewing tobacco in the past month (Table 4), suggesting that these stimulants may be responsible for the high urinary concentrations identified in many pregnant women. Notably, OTA and CIT, the most frequently detected mycotoxins, have been reported in rice in Asia, the primary staple food in the sub-region (Ali et al. 2018; Reddy et al. 2009). However, as rice was consumed daily by all the women in our study, it was impossible to analyze its association with urinary mycotoxin concentrations.
A previous study in Bangladesh detected aflatoxin levels above US maximum regulatory levels in eight commonly ingested food commodities, including rice, lentils, wheat flour, dates, betelnut, and groundnut (Roy et al. 2013). AFM1 was, however, detected in only a few urine samples in our pregnant cohort, suggesting that very high aflatoxin exposure does not frequently occur in this community. Still, given that AFM1 has been detected in greater frequency in other studies in Bangladesh (Ali et al. 2017), this low occurrence may be a limitation of using a urine biomarker that only reflects acute exposures, although the LOD/LOQ obtained with the used 'dilute and shoot' approach is higher compared to other studies applying an additional sample cleanup step (Ali et al. 2017; Šarkanj et al. 2018). Consequently, to determine whether aflatoxin exposure is really low in our study population, measurement of aflatoxin B1-lysine adduct in blood samples will be carried out in a follow-up project. This long-term biomarker based on the formation of aflatoxin-B1-albumin allows for accurate and sensitive quantification of AFB1 uptake over the past two months.
The present study is unique due to the large study sample of pregnant women (n = 447) with paired data from the FAARM food consumption survey and the multiple urinary mycotoxin biomarker analysis. The applied method is based on a dilute and shoot approach, covering a broad spectrum of compounds but focusing on the previously detected highly relevant mycotoxins OTA and CIT / HO-CIT. For other analytes, a moderate sensitivity was accepted as no more sensitive methods with comparable efficiency were available at the time of sample analysis (Schmidt et al. 2021a). As a consequence, the LODs of some mycotoxins were comparably high, allowing only the detection of very high exposure scenarios but not the baseline level of mycotoxin uptake present in Bangladesh.
While urine is convenient for population-based biomonitoring studies due to the non-invasive sampling involved, the daily variation in urine composition and excretion rate among individuals adds some difficulties. We adjusted for inter-individual variations in urine volume by correcting urine mycotoxin concentrations for urine density and urine creatinine before dietary exposure estimation. Despite the inherent challenges in assessing diets accurately given misreporting and misclassification biases, we found evidence that reported intake of certain foods and stimulants was linked to urinary mycotoxin concentrations. However, our dietary assessment was not comprehensive. For example, spices were not covered in our dietary survey but are also a common source of high OTA contamination (Kabak and Dobson 2017). Sampling common foods and stimulants, as well as spices, from our study population for direct mycotoxin contamination analysis will be valuable in ascertaining the sources of dietary mycotoxin contamination in this population. Our study was conducted among pregnant women from rural households in Habiganj district who participated in the FAARM trial, and thus the conclusions cannot necessarily be generalized to other areas. However, our results were similar to those from previous biomonitoring studies in Bangladesh, suggesting that our study population is typical for rural settings in Bangladesh, and findings may, thus, also apply to similar settings.
Overall, the following conclusions can be drawn from our study:
-
Exposure to multiple mycotoxins during early pregnancy is widespread in this rural community and represents a potential health risk for mothers and babies.
-
OTA alone or in combination with citrinin, produced by post-harvest or storage molds, are ubiquitous food contaminants in this community.
-
FB1, ZEN, DON, and other trichothecenes, produced by pre-harvest or field molds, are less common contaminants of foods consumed by pregnant women in this community.
-
The local stimulants betel nut, betel leaf, and chewing tobacco may be possible sources of OTA, CIT, and DON exposure among pregnant women in this community.
Although mycotoxins cannot be completely eliminated from food or feed supplies, their levels can be substantially reduced by promoting good agricultural practices, safe food habits and proper storage. This is an important challenge for agricultural extension work. Future research should explore the role of concurrent exposure to multiple mycotoxins for the development of adverse health outcomes in mothers, newborns, and children.
Data availability statement
The data presented in this study are available upon reasonable request from the corresponding author. The data are not publicly available due to privacy restrictions.
References
Abdulrazzaq YM, Osman N, Ibrahim A (2002) Fetal exposure to aflatoxins in the United Arab Emirates. Ann Trop Paediatr 22(1):3–9
Ali N, Degen GH (2019) Biomonitoring of zearalenone and its main metabolites in urines of Bangladeshi adults. Food Chem Toxicol 130:276–283. https://doi.org/10.1016/j.fct.2019.05.036
Ali N, Degen GH (2020) Biological monitoring for ochratoxin A and citrinin and their metabolites in urine samples of infants and children in Bangladesh. Mycotoxin Res 36:409–417. https://doi.org/10.1007/s12550-020-00407-7
Ali N, Blaszkewicz M, Al Nahid A, Rahman M, Degen GH (2015a) Deoxynivalenol exposure assessment for pregnant women in Bangladesh. Toxins (basel) 7(10):3845–3857. https://doi.org/10.3390/toxins7103845
Ali N, Blaszkewicz M, Mohanto NC et al (2015b) First results on citrinin biomarkers in urines from rural and urban cohorts in Bangladesh. Mycotoxin Res 31:9–16. https://doi.org/10.1007/s12550-014-0217-z
Ali N, Blaszkewicz M, Alim A, Hossain K, Degen GH (2016a) Urinary biomarkers of ochratoxin A and citrinin exposure in two Bangladeshi cohorts: follow-up study on regional and seasonal influences. Arch Toxicol 90:2683–2697. https://doi.org/10.1007/s00204-015-1654-y
Ali N, Blaszkewicz M, Degen GH (2016b) Assessment of deoxynivalenol exposure among Bangladeshi and German adults by a biomarker-based approach. Toxicol Lett 258:20. https://doi.org/10.1016/j.toxlet.2016.06.006
Ali N, Blaszkewicz M, Manirujjaman M, Degen GH (2016c) Biomonitoring of concurrent exposure to ochratoxin A and citrinin in pregnant women in Bangladesh. Mycotoxin Res 32:163–172. https://doi.org/10.1007/s12550-016-0251-0
Ali N, Hossain K, Blaszkewicz M et al (2016d) Occurrence of aflatoxin M1 in urines from rural and urban adult cohorts in Bangladesh. Arch Toxicol 90(7):1749–1755. https://doi.org/10.1007/s00204-015-1601-y
Ali N, Blaszkewicz M, Hossain K, Degen GH (2017) Determination of aflatoxin M1 in urine samples indicates frequent dietary exposure to aflatoxin B1 in the Bangladeshi population. Int J Hyg Environ Health 220:271–281. https://doi.org/10.1016/j.ijheh.2016.11.002
Ali N, Hossain K, Degen GH (2018) Blood plasma biomarkers of citrinin and ochratoxin A exposure in young adults in Bangladesh. Mycotoxin Res 34:59–67. https://doi.org/10.1007/s12550-017-0299-5
Ali N, Manirujjaman M, Rana S, Degen GH (2020) Determination of aflatoxin M(1) and deoxynivalenol biomarkers in infants and children urines from Bangladesh. Arch Toxicol 94(11):3775–3786. https://doi.org/10.1007/s00204-020-02857-5
Codex Alimentarius (2016) Code of practice for the prevention and reduction of mycotoxin contamination in cereals CAC/RCP 51–2003. Codex alimentarius commission
Al-Jaal BA, Jaganjac M, Barcaru A (2019) Aflatoxin, fumonisin, ochratoxin, zearalenone and deoxynivalenol biomarkers in human biological fluids: a systematic literature review, 2001–2018. Food Chem Toxicol 129:211–228. https://doi.org/10.1016/j.fct.2019.04.047
Alshannaq A, Yu J-H (2017) Occurrence, Toxicity, and Analysis of Major Mycotoxins in Food. Int J Environ Res Public Health 14(6):632. https://doi.org/10.3390/ijerph14060632
Andrews-Trevino JY, Webb P, Shively G et al (2019) Relatively low maternal aflatoxin exposure is associated with small-for-gestational-age but not with other birth outcomes in a prospective birth cohort study of nepalese infants. J Nutr 149(10):1818–1825. https://doi.org/10.1093/jn/nxz122
Andrews-Trevino JY, Webb P, Shively G et al (2021) Aflatoxin exposure and child nutrition: measuring anthropometric and long-bone growth over time in Nepal. Am J Clin Nutr 113(4):874–883. https://doi.org/10.1093/ajcn/nqaa397
Bennett JW, Klich M (2003) Mycotoxins. Clin Microbiol Rev 16(3):497–516. https://doi.org/10.1128/CMR.16.3.497-516.2003
Bhatnagar D, Yu J, Ehrlich KC (2002) Toxins of filamentous fungi. Chem Immunol 81:167–206. https://doi.org/10.1159/000058867
Carrieri M, Trevisan A, Bartolucci GB (2001) Adjustment to concentration-dilution of spot urine samples: correlation between specific gravity and creatinine. Int Arch Occup Environ Health 74(1):63–67. https://doi.org/10.1007/s004200000190
Chan-Hon-Tong A, Charles MA, Forhan A, Heude B, Sirot V (2013) Exposure to food contaminants during pregnancy. Sci Total Environ 458:27–35. https://doi.org/10.1016/j.scitotenv.2013.03.100
Dawlatana M, Coker RD, Nagler MJ, Wild CP, Hassan MS, Blunden G (2002) The occurrence of mycotoxins in key commodities in Bangladesh: surveillance results from 1993 to 1995. J Nat Toxins 11(4):379–386
Degen GH (2011) Tools for investigating workplace-related risks from mycotoxin exposure. World Mycotoxin J 4:315–327. https://doi.org/10.3920/WMJ2011.1295
Degen GH (2015) Are we ready to estimate daily ochratoxin A intake based on urinary concentration? Environ Int 97:254–255. https://doi.org/10.1016/j.envint.2015.10.010
Degen GH, Ali N, Gundert-Remy U (2018) Preliminary data on citrinin kinetics in humans and their use to estimate citrinin exposure based on biomarkers. Toxicol Lett 282:43–48. https://doi.org/10.1016/j.toxlet.2017.10.006
EFSA (2006) Opinion of the scientific panel on contaminants in the food chain [CONTAM] related to ochratoxin A in food. EFSA J 365:1–56. https://doi.org/10.2903/j.efsa.2006.365
EFSA (2010) Management of left-censored data in dietary exposure assessment of chemical substances. EFSA J 8(3):1557. https://doi.org/10.2903/j.efsa.2010.1557
EFSA (2012) Scientific opinion on the risks for public and animal health related to the presence of citrinin in food and feed. EFSA J 10:2605
EFSA (2013) International frameworks dealing with human risk assessment of combined exposure to multiple chemicals. EFSA J 11(7):3313. https://doi.org/10.2903/j.efsa.2013.3313
EFSA (2017) Scientific opinion on the risks to human and animal health related to the presence of deoxynivalenol and its acetylated and modified forms in food and feed Deoxynivalenol, 3-acetyl-deoxynivalenol, 15-acetyl-deoxynivalenol. EFSA J 15:345. https://doi.org/10.2903/j.efsa.2017.4718
EFSA Contam Panel (EFSA Panel on Contaminants in the Food Chain), Schrenk D, Bodin L et al (2020a) Scientific opinion on the risk assessment of ochratoxin A in food. EFSA J 18(5):6133. https://doi.org/10.2903/j.efsa.2020.6113
EFSA Contam Panel (EFSA panel on contaminants in the food chain), Schrenk D, Bodin L et al (2020b) Scientific Opion on the risk assessment of aflatoxins in food. EFSA J 18(3):6040. https://doi.org/10.2903/j.efsa.2020.6040
Escrivá L, Font G, Manyes L, Berrada H (2017) Studies on the presence of mycotoxins in biological samples: an overview. Toxins 9(8):251
Eskola M, Kos G, Elliott CT, Hajšlová J, Mayar S, Krska R (2020) Worldwide contamination of food-crops with mycotoxins: Validity of the widely cited ‘FAO estimate’ of 25%. Crit Rev Food Sci Nutr 60(16):2773–2789. https://doi.org/10.1080/10408398.2019.1658570
Ezekiel CN, Abia WA, Braun D et al (2022) Mycotoxin exposure biomonitoring in breastfed and non-exclusively breastfed Nigerian children. Environm Int 158:106996
FAO, FHI 360 (2016) Minimum dietary diversity for women: a guide for measurement. Food and Agriculture Organization of the United Nations, Rome
FAO/WHO (2011) Safety evaluation of certain contaminants in food (deoxynivalenol). Prepared by the seventy-second meeting of the Joint FAO/WHO Expert committee in food additives (JECFA) WHO food additives series 63. Food and Agriculture Organization of the United Nations/World Health Organization, Geneva
Frisvad JC, Thrane U, Samson RA, Pitt JI (2006) Important mycotoxins and the fungi which produce them. Adv Exp Med Biol 571:3–31. https://doi.org/10.1007/0-387-28391-9_1
Frisvad JC, Larsen TO, Thrane U et al (2011) Fumonisin and ochratoxin production in industrial Aspergillus niger strains. PLoS ONE 6(8):e23496–e23496. https://doi.org/10.1371/journal.pone.0023496
Fromme H, Gareis M, Völkel W, Gottschalk C (2016) Overall internal exposure to mycotoxins and their occurrence in occupational and residential settings–An overview. Int J Hyg Environ Health 219(2):143–165. https://doi.org/10.1016/j.ijheh.2015.11.004
Gambacorta L, Olsen M, Solfrizzo M (2019) Pig Urinary concentration of mycotoxins and metabolites reflects regional differences mycotoxin intake and feed contaminations. Toxins (basel) 11(7):299–308. https://doi.org/10.3390/toxins11070378
Gerding J, Cramer B, Humpf HU (2014) Determination of mycotoxin exposure in Germany using an LC-MS/MS multibiomarker approach. Mol Nutr Food Res 58(12):2358–2368. https://doi.org/10.1002/mnfr.201400406
Gerding J, Ali N, Schwartzbord J et al (2015) A comparative study of the human urinary mycotoxin excretion patterns in Bangladesh, Germany, and Haiti using a rapid and sensitive LC-MS/MS approach. Mycotoxin Res 31:127–136. https://doi.org/10.1007/s12550-015-0223-9
Goyarts T, Dänicke S, Brüssow KP, Valenta H, Ueberschär KH, Tiemann U (2007) On the transfer of the fusarium toxins deoxynivalenol (DON) and zearalenone (ZON) from sows to their fetuses during days 35–70 of gestation. Toxicol Lett 171(1–2):38–49. https://doi.org/10.1016/j.toxlet.2007.04.003
Groopman JD, Egner PA, Schulze KJ et al (2014) Aflatoxin exposure during the first 1000 days of life in rural South Asia assessed by aflatoxin B(1)-lysine albumin biomarkers. Food Chem Toxicol 74:184–189
IARC (2015) In: Wild CP, Miller JD, Groopman JD (eds) Working Group Report No 9, Mycotoxin control in low- and middle-income countries. International Agency for Research on Cancer, Lyon (FR)
Islam GM, Hoque M (2013) Food safety regulation in Bangladesh, chemical hazard and some perception to overcome the dilemma. Int Food Res J 20:47–58
Islam F, Das Trisha A, Hafsa JM, Hasan A, Degen GH, Ali N (2021) Occurrence of aflatoxin M(1) in human breast milk in Bangladesh. Mycotoxin Res 37(3):241–248. https://doi.org/10.1007/s12550-021-00436-w
Ismail A, Naeem I, Gong YY et al (2021) Early life exposure to dietary aflatoxins, health impact and control perspectives: A review. Trends Food Sci Technol 112:212–224
Jonsyn FE, Maxwell SM, Hendrickse RG (1995) Human fetal exposure to ochratoxin A and Aflatoxins. Ann Trop Paediatr 15(1):3–9
Kabak B, Dobson AD (2017) Mycotoxins in spices and herbs-An update. Crit Rev Food Sci Nutr 57(1):18–34. https://doi.org/10.1080/10408398.2013.772891
Kyei NNA, Boakye D, Gabrysch S (2020) Maternal mycotoxin exposure and adverse pregnancy outcomes: a systematic review. Mycotoxin Res 36(2):243–255. https://doi.org/10.1007/s12550-019-00384-6
Kyei NNA, Waid JL, Ali N, Gabrysch S (2021) Awareness, experience, and knowledge of farming households in rural bangladesh regarding mold contamination of food crops: a cross-sectional study. Int J Environ Res Public Health 18(19):10335. https://doi.org/10.3390/ijerph181910335
Lei Y, Fang L, Akash MSH et al (2013) Estimation of urinary concentration of aflatoxin M1 in Chinese pregnant women. J Food Sci 78(11):T1835–T1838
Marin S, Ramos AJ, Cano-Sancho G, Sanchis V (2013) Mycotoxins: occurrence, toxicology, and exposure assessment. Food Chem Toxicol 60:218–237. https://doi.org/10.1016/j.fct.2013.07.047
Metrics for Management (2016) Bangladesh equity tool. https://www.equitytool.org/bangladesh
Mikhail MS, Anyaegbunam A (1995) Lower urinary tract dysfunction in pregnancy: a review. Obstet Gynecol Surv 50(9):675–683. https://doi.org/10.1097/00006254-199509000-00022
Nielsen JK, Vikström AC, Turner P, Knudsen LE (2011) Deoxynivalenol transport across the human placental barrier. Food Chem Toxicol 49(9):2046–2052. https://doi.org/10.1016/j.fct.2011.05.016
NIPORT, Mitra and Associates, ICF International (2016) Bangladesh demographic and health survey 2014. National Institute of Population Research and Training-NIPORT Bangladesh, Mitra and Associates, and ICF International., Dhaka, Bangladesh
Partanen HA, El-Nezami HS, Leppänen JM, Myllynen PK, Woodhouse HJ, Vähäkangas KH (2010) Aflatoxin B1 transfer and metabolism in human placenta. Toxicol Sci 113(1):216–225. https://doi.org/10.1093/toxsci/kfp257
Reddy RV, Hayes AW, Berndt WO (1982) Disposition and metabolism of [14C]Citrinin in pregnant rats. Toxicology 25(2–3):161–174. https://doi.org/10.1016/0300-483x(82)90027-0
Reddy KRN, Abbas HK, Abel CA, Shier WT, Oliveira CAF, Raghavender CR (2009) Mycotoxin contamination of commercially important agricultural commodities. Toxin Rev 28(2–3):154–168. https://doi.org/10.1080/15569540903092050
Roy M, Harris J, Afreen S et al (2013) Aflatoxin contamination in food commodities in Bangladesh. Food Addit Contam Part B Surveill 6(1):17–23. https://doi.org/10.1080/19393210.2012.720617
Rychlik M, Humpf HU, Marko D et al (2014) Proposal of a comprehensive definition of modified and other forms of mycotoxins including “masked” mycotoxins. Mycotoxin Res 30(4):197–205. https://doi.org/10.1007/s12550-014-0203-5
Šarkanj B, Ezekiel CN, Turner PC et al (2018) Ultra-sensitive, stable isotope assisted quantification of multiple urinary mycotoxin exposure biomarkers. Anal Chim Acta 1019:84–92. https://doi.org/10.1016/j.aca.2018.02.036
Schmidt J, Cramer B, Turner PC et al (2021a) Determination of urinary mycotoxin biomarkers using a sensitive online solid phase extraction-UHPLC-MS/MS method. Toxins (basel) 13(6):418. https://doi.org/10.3390/toxins13060418
Schmidt J, Lindemann V, Olsen M, Cramer B, Humpf HU (2021b) Dried urine spots as sampling technique for multi-mycotoxin analysis in human urine. Mycotoxin Res 37(2):129–140. https://doi.org/10.1007/s12550-021-00423-1
Sherif SO, Salama EE, Abdel-Wahhab MA (2009) Mycotoxins and child health: the need for health risk assessment. Int J Hyg Environ Health 212(4):347–368. https://doi.org/10.1016/j.ijheh.2008.08.002
Smith KW, Braun JM, Williams PL, Ehrlich S, Correia KF, Calafat AM, Ye X, Ford J, Keller M, Meeker JD, Hauser R (2012) Predictors and variability of urinary paraben concentrations in men and women including before and during pregnancy. Environ Health Perspect 120(11):1538–1543. https://doi.org/10.1289/ehp.1104614
Solfrizzo M, Gambacorta L, Visconti A (2014) Assessment of multi-mycotoxin exposure in southern Italy by urinary multi-biomarker determination. Toxins (basel) 6(2):523–538. https://doi.org/10.3390/toxins6020523
Studer-Rohr I, Schlatter J, Dietrich DR (2000) Kinetic parameters and intraindividual fluctuations of ochratoxin A plasma levels in humans. Arch Toxicol 74(9):499–510. https://doi.org/10.1007/s002040000157
Sumon AH, Islam F, Mohanto NC et al (2021) The Presence of Aflatoxin M1 in Milk and Milk Products in Bangladesh. Toxins (basel) 13(7):440. https://doi.org/10.3390/toxins13070440
Suwazono Y, Akesson A, Alfven T, Jarup L, Vahter M (2005) Creatinine versus specific gravity-adjusted urinary cadmium concentrations. Biomarkers 10:117–126. https://doi.org/10.1080/13547500500159001
Turner PC, Flannery B, Isitt C, Ali M, Pestka J (2012) The role of biomarkers in evaluating human health concerns from fungal contaminants in food. Nutr Res Rev 25(1):162–179
Vidal A, Mengelers M, Yang S, De Saeger S, De Boevre M (2018) Mycotoxin biomarkers of exposure: a comprehensive review. Compr Rev Food Sci Food Saf 17(5):1127–1155. https://doi.org/10.1111/1541-4337.12367
Warensjö Lemming E, Montano Montes A, Schmidt J et al (2020) Mycotoxins in blood and urine of Swedish adolescents—possible associations to food intake and other background characteristics. Mycotoxin Res 36(2):193–206. https://doi.org/10.1007/s12550-019-00381-9
Warth B, Sulyok M, Berthiller F, Schuhmacher R, Krska R (2013) New insights into the human metabolism of the Fusarium mycotoxins deoxynivalenol and zearalenone. Toxicol Lett 220(1):88–94. https://doi.org/10.1016/j.toxlet.2013.04.012
Warth B, Petchkongkaew A, Sulyok M, Krska R (2014) Utilising an LC-MS/MS-based multi-biomarker approach to assess mycotoxin exposure in the Bangkok metropolitan area and surrounding provinces. Food Addit Contamin Part A 31(12):2040–2046
Warth B, Preindl K, Manser P, Wick P, Marko D, Buerki-Thurnherr T (2019) Transfer and metabolism of the xenoestrogen zearalenone in human perfused placenta. Environ Health Perspect 127(10):107004. https://doi.org/10.1289/ehp4860
Wendt AS, Sparling TM, Waid JL, Mueller AA, Gabrysch S (2019) Food and agricultural approaches to reducing malnutrition (FAARM): protocol for a cluster-randomised controlled trial to evaluate the impact of a Homestead Food Production programme on undernutrition in rural Bangladesh. BMJ Open 9(7):e031037. https://doi.org/10.1136/bmjopen-2019-031037
Woo CS, Partanen H, Myllynen P, Vähäkangas K, El-Nezami H (2012) Fate of the teratogenic and carcinogenic ochratoxin A in human perfused placenta. Toxicol Lett 208(1):92–99. https://doi.org/10.1016/j.toxlet.2011.10.013
Zhu JQ, Zhang LS, Hu X et al (1987) Correlation of dietary aflatoxin B1 levels with excretion of aflatoxin M1 in human urine. Cancer Res 47(7):1848–1852
Acknowledgements
Nicholas Kyei thanks the GNPC Foundation Fellowships for scholarship support between 2017 and 2020 to undertake his Ph.D. studies in Heidelberg. Special thanks to Amanda Wendt and Jillian Waid for their help and advice during data collection and help with the food consumption data. Also grateful to Maik Brune for his assistance with urine creatinine and density analysis, and to Abdul Kader and Shafinaz Sobhan for Bangla–English translation and fieldwork support. Finally, we thank the women enrolled in the MEMAPO study for their valuable time and participation.
Funding
Open Access funding enabled and organized by Projekt DEAL. The German Ministry for Education and Research (BMBF) (grant number: 01ER1201) is the primary funder for the FAARM trial. Sabine Gabrysch received funding from a Recruiting Grant of Stiftung Charité. Nicholas Kyei completed this work as part of his doctoral thesis, supported by the Ghana National Petroleum Corporation (GNPC) Foundation Ph.D. Fellowship.
Author information
Authors and Affiliations
Contributions
NNA Kyei: Conceptualization, Methodology, Software, Formal analysis, Investigation, Resources, Data curation, Writing—Original Draft preparation, Visualization. S Gabrysch: Conceptualization, Methodology, Supervision, Writing—Review and Editing. B Cramer: Conceptualization, Methodology, Investigation, Validation, Data curation, Writing—Review and Editing. HU Humpf: Conceptualization, Methodology, Resources, Writing—Review and Editing, Supervision. GH Degen: Conceptualization, Writing—Review and Editing. N Ali: Conceptualization, Writing—Review and Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper. The funders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the result.
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki. The FAARM protocol was positively reviewed by ethics committees in Bangladesh and Germany, and written informed consent was obtained from all study participants before data collection (Wendt et al. 2019). The MEMAPO study was additionally reviewed by Heidelberg University in Germany and the Institute of Health Economics's institutional review board at the University of Dhaka, Bangladesh (Reference: FWA00026031). After clarifying the study objective and the voluntary nature of participation, written informed consent was obtained from all study participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kyei, N.N.A., Cramer, B., Humpf, HU. et al. Assessment of multiple mycotoxin exposure and its association with food consumption: a human biomonitoring study in a pregnant cohort in rural Bangladesh. Arch Toxicol 96, 2123–2138 (2022). https://doi.org/10.1007/s00204-022-03288-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-022-03288-0