Abstract
Summary
Joint replacement surgery is common in older adults, leading to increasing periprosthetic fracture (PPFx) occurrence. We reviewed all PPFx seen over a 4-year period at an academic hospital. Clinical osteoporosis could be diagnosed based on existing data in 104 (67%) at the time of PPFx. Periprosthetic fractures are generally osteoporosis-related.
Purpose
Periprosthetic fractures (PPFx) cause morbidity, mortality, and cost. This study’s purpose was to describe osteoporosis-related data available at the time of PPFx.
Methods
The electronic medical record (EMR) of PPFx patients seen over 4 years in a university orthopedic practice were reviewed. Demographic data and osteoporosis relevant parameters were collected. Prior DXA studies were reviewed, and L1 Hounsfield unit (HU) measurements were performed on CT scans obtained within 2 years before PPFx. Clinical osteoporosis was defined as prior diagnosis, prescribed osteoporosis treatment, T-score ≤ − 2.5, HU ≤ 100, or prior fracture.
Results
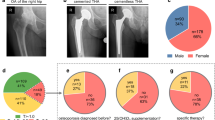
Records of 156 PPFx patients (115 F/41 M), mean (SD) age 75.4 (11.9), were reviewed. Almost all 153/156 (98%) of these fractures were femoral. Falls caused 139 (89%); 12 (8%) were spontaneous. Mean time post-arthroplasty was 7.9 (6.3) years. Prior fragility fracture(s) occurred in 72 (46%); 14 were PPFx. Osteoporosis was previously diagnosed in 45 (29%) and medications prescribed in 41 (26%). Prior to PPFx, DXA data were available in 62, mean (SD) lowest T-score was − 1.9 (0.9) and was ≤ − 2.5 in 19. CT data were available in 46; mean (SD) L1 HU was 79.0 (29.4) and was ≤ 100 in 35. Based on existing data, clinical osteoporosis could have been diagnosed in 104 (67%) at the time of PPFx.
Conclusion
Periprosthetic fractures are osteoporosis-related. They occur in older adults, often female, and result from falls; BMD, when assessed, is low. Data available at the time of PPFx often allows osteoporosis diagnosis; this should prompt evaluation and pharmacologic treatment consideration.


Similar content being viewed by others
References
Maradit Kremers H, Larson DR, Crowson CS, Kremers WK, Washington RE, Steiner CA, Jiranek WA, Berry DJ (2015) Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am Vol 97:1386–1397
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am Vol 89:780–785
Schwartz AM, Farley KX, Guild GN, Bradbury TL Jr (2020) Projections and epidemiology of revision hip and knee arthroplasty in the United States to 2030. J Arthroplasty 35:S79-s85
Bernatz JT, Brooks AE, Squire MW, Illgen RI 2nd, Binkley NC, Anderson PA (2019) Osteoporosis is common and undertreated prior to total joint arthroplasty. J Arthroplasty 34:1347–1353
Kadri A, Binkley N, Hare KJ, Anderson PA (2020) Bone health optimization in orthopaedic surgery. J Bone Joint Surg 102:574–581
Bernatz JT, Krueger DC, Squire MW, Illgen RL 2nd, Binkley NC, Anderson PA (2019) Unrecognized osteoporosis is common in patients with a well-functioning total knee arthroplasty. J Arthroplasty 34:2347–2350
Prince JM, Bernatz JT, Binkley N, Abdel MP, Anderson PA (2019) Changes in femoral bone mineral density after total knee arthroplasty: a systematic review and meta-analysis. Arch Osteoporos 14:23
Meyer JS, Freitag T, Reichel H, Bieger R (2019) Periprosthetic bone mineral density changes after implantation of a curved bone preserving hip stem compared to a standard length straight stem: 5-yr results of a prospective, randomized DXA-analysis. J Clin Densitom 22:96–103
Peitgen DS, Innmann MM, Merle C, Gotterbarm T, Moradi B, Streit MR (2018) Periprosthetic bone mineral density around uncemented titanium stems in the second and third decade after total hip arthroplasty: a DXA study after 12, 17 and 21 years. Calcif Tissue Int 103:372–379
Knutsen AR, Lau N, Longjohn DB, Ebramzadeh E, Sangiorgio SN (2017) Periprosthetic femoral bone loss in total hip arthroplasty: systematic analysis of the effect of stem design. Hip Int 27:26–34
Morita A, Kobayashi N, Choe H, Ike H, Tezuka T, Higashihira S, Inaba Y (2020) Effect of switching administration of alendronate after teriparatide for the prevention of BMD loss around the implant after total hip arthroplasty, 2-year follow-up: a randomized controlled trial. J Orthop Surg Res 15:17
Yukizawa Y, Inaba Y, Kobayashi N, Choe H, Kubota S, Saito T (2017) Efficacy of alendronate for the prevention of bone loss in calcar region following total hip arthroplasty. J Arthroplasty 32:2176–2180
Luzzi AJ, Fleischman AN, Matthews CN, Crizer MP, Wilsman J, Parvizi J (2018) The “bundle busters”: incidence and costs of postacute complications following total joint arthroplasty. J Arthroplasty 33:2734–2739
Jennnison T, Yarlagadda R (2020) A case-control study of 30-day mortality in periprosthetic hip fractures and hip fractures. Ann R Coll Surg Engl 102:229–231
Lyons RF, Piggott RP, Curtin W, Murphy CG (2018) Periprosthetic hip fractures: a review of the economic burden based on length of stay. J Orthop 15:118–121
Eschbach D, Buecking B, Kivioja H et al (2018) One year after proximal or distal periprosthetic fracture of the femur -two conditions with divergent outcomes? Injury 49:1176–1182
Zheng H, Gu H, Shao H, Huang Y, Yang D, Tang H, Zhou Y (2020) Treatment and outcomes of Vancouver type B periprosthetic femoral fractures. Bone Joint J 102-b:293–300
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med 158:588–595
Pickhardt PJ, Lauder T, Pooler BD, Munoz Del Rio A, Rosas H, Bruce RJ, Binkley N (2016) Effect of IV contrast on lumbar trabecular attenuation at routine abdominal CT: correlation with DXA and implications for opportunistic osteoporosis screening. Osteoporos Int 27:147–152
Anderson PA, Morgan SL, Krueger D et al (2019) Use of bone health evaluation in orthopedic surgery: 2019 ISCD official position. J Clin Densitom 22:517–543
Shane E, Burr D, Abrahamsen B et al (2014) Atypical subtrochanteric and diaphyseal femoral fractures: second report of a task force of the American Society for Bone and Mineral Research. J Bone Miner Res 29:1–23
McCloskey E, Rathi J, Heijmans S et al (2021) The osteoporosis treatment gap in patients at risk of fracture in European primary care: a multi-country cross-sectional observational study. Osteoporos Int 32:251–259
Kanis JA, Svedbom A, Harvey N, McCloskey EV (2014) The osteoporosis treatment gap. J Bone Miner Res 29:1926–1928
Binkley N, Nickel B, Anderson PA (2023) Periprosthetic fractures: an unrecognized osteoporosis crisis. Osteoporos Int 34:1055–1064
Prieto-Alhambra D, Javaid MK, Judge A, Maskell J, Cooper C, Arden NK (2015) Hormone replacement therapy and mid-term implant survival following knee or hip arthroplasty for osteoarthritis: a population-based cohort study. Ann Rheum Dis 74:557–563
Prieto-Alhambra D, Lalmohamed A, Abrahamsen B, Arden NK, de Boer A, Vestergaard P, de Vries F (2014) Oral bisphosphonate use and total knee/hip implant survival: validation of results in an external population-based cohort. Arthritis Rheumatol 66:3233–3240
McDonald CL, Lemme NJ, Testa EJ, Aaron R, Hartnett DA, Cohen EM (2022) Bisphosphonates in total joint arthroplasty: a review of their use and complications. Arthroplasty Today 14:133–139
Smith-Bindman R, Kwan ML, Marlow EC et al (2019) Trends in use of medical imaging in US health care systems and in Ontario, Canada, 2000–2016. J Am Med Assoc 322:843–856
Cohen JS, Agarwal AR, Kinnard MJ, Thakkar SC, Golladay GJ (2023) The association of postoperative osteoporosis therapy with periprosthetic fracture risk in patients undergoing arthroplasty for femoral neck fractures. J Arthroplasty 38:726–731
Zhao AY, Agarwal AR, Harris AB, Cohen JS, Golladay GJ, Thakkar SC (2023) The association of prior fragility fractures on 8-year periprosthetic fracture risk following total hip arthroplasty. J Arthroplasty 38:S265–S269
Agarwal AR, Cohen JS, Tarawneh OH, Gu A, Debritz J, Golladay GJ, Thakkar SC (2023) The impact of prior fragility fractures on long-term periprosthetic fracture risk following total knee arthroplasty. Osteoporosis Int 34:1429–1436
Ross AJ, Ross BJ, Lee OC, Guild GN 3rd, Sherman WF (2021) The impact of prior fragility fractures on complications after total hip arthroplasty: a propensity score-matched cohort study. Arthroplasty Today 11:41–48
Albright JA, Testa EJ, Meghani O, Chang K, Daniels AH, Barrett TJ (2023) Increased risk of hospital readmissions and implant-related complications in patients who had a recent history of fragility fracture: a matched cohort analysis. J Arthroplasty 38:266–273
Testa EJ, Albright JA, Lemme NJ, Molla V, McCrae B, Daniels AH, Paxton ES (2023) Increased risk of periprosthetic fractures and revision arthroplasty in patients undergoing shoulder arthroplasty with a history of prior fragility fractures: a matched cohort analysis. J Am Acad Orthop Surg 31:e473–e480
Ferreira P, Bates P, Daoub A, Dass D (2023) Is bisphosphonate use a risk factor for atypical periprosthetic/peri-implant fractures? - A metanalysis of retrospective cohort studies and systematic review of the current evidence. Orthop Traumatol Surg Res 109:103475
Lee YK, Park CH, Kim KC, Hong SH, Ha YC, Koo KH (2018) Frequency and associated factor of atypical periprosthetic femoral fracture after hip arthroplasty. Injury 49:2264–2268
Nickel B, Krueger D, Borchardt G, Andersen L, Illgen R, Hennessy D, Hetzel S, Binkley N, Anderson PA (2023) Intraoperative physician assessment of bone: correlation to bone mineral density. Osteoporos Int 34:1093–1099
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. S Whiting, K. Hare, D. Krueger, G. Borchardt, K. Parvanta-Johnson, J. Bernatz, and P. A. Anderson declare no conflict of interest. Neil Binkley declares no conflict of interest for the content of this paper; research funding from Radius; consultant Amgen and Radius.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Whiting, P.S., Hare, K., Krueger, D. et al. Periprosthetic fractures are osteoporotic fractures: missed opportunities for osteoporosis diagnosis. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07057-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07057-w