Abstract
Summary
This study evaluated the intraoperative physician assessment (IPA) of bone status at time of total knee arthroplasty. IPA was highly correlated with distal femur and overall bone mineral density. When IPA identifies poor bone status, formal bone health assessment is indicated.
Purpose
Intuitively, intraoperative physician assessment (IPA) would be an excellent measure of bone status gained through haptic feedback during bone preparation. However, no studies have evaluated the orthopedic surgeon’s ability to do so. This study’s purpose, in patients undergoing total knee arthroplasty (TKA), was to relate IPA with (1) the lowest bone mineral density (BMD) T-score at routine clinical sites; and (2) with distal femur BMD.
Methods
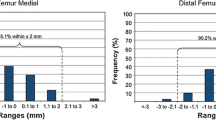
Seventy patients undergoing TKA by 3 surgeons received pre-operative DXA. Intraoperatively, bone quality was assessed on a 5-point scale (1 excellent to 5 poor) based on tactile feedback to preparation. Demographic data, DXA results, and IPA score between surgeons were compared by factorial ANOVA. Lowest T-score and distal femur BMD were associated with IPA using Spearman’s correlation.
Results
The mean (SD) age and BMI were 65.8 (7.6) years and 31.4 (5.1) kg/m2, respectively. Patient demographic data, BMD, and IPA (mean [SD] = 2.74 [1.2]) did not differ between surgeons. IPA correlated with the lowest T-score (R = 0.511) and distal femur BMD (R = 0.603–0.661). Based on the lowest T-score, no osteoporotic patients had an IPA above average, and none with normal BMD was classified as having poor bone.
Conclusions
IPA is highly correlated with local (distal femur) and overall BMD. This study supports the International Society for Clinical Densitometry position that surgeon concern regarding bone quality should lead to bone health assessment. As IPA is comparable between surgeons, it is logical this can be widely applied by experienced orthopedic surgeons. Future studies evaluating IPA at other anatomic sites are indicated.


Similar content being viewed by others
References
Shuhart CR, Yeap SS, Anderson PA, Jankowski LG, Lewiecki EM, Morse LR, Rosen HN, Weber DR, Zemel BS, Shepherd JA (2019) Executive summary of the 2019 ISCD position development conference on monitoring treatment, DXA cross-calibration and least significant change, spinal cord injury, peri-prosthetic and orthopedic bone health, transgender medicine, and pediatrics. J Clin Densitom 22:453–471
Anderson PA, Morgan SL, Krueger D et al (2019) Use of bone health evaluation in orthopedic surgery: 2019 ISCD official position. J Clin Densitom 22:517–543
Gehweiler D, Styger U, Gueorguiev B, Colcuc C, Vordemvenne T, Wähnert D (2021) Local bone quality measure and construct failure prediction: a biomechanical study on distal femur fractures. Arch Orthop Trauma Surg 142:1055
James TP, Pearlman JJ, Saigal A (2013) Predictive force model for haptic feedback in bone sawing. Med Eng Phys 35:1638–1644
Lin Y, Chen H, Yu D, Zhang Y, Yuan W (2017) A predictive bone drilling force model for haptic rendering with experimental validation using fresh cadaveric bone. Int J Comput Assist Radiol Surg 12:91–98
Chang E, Binkley N, Krueger D, Nickel BT, Anderson PA (2022) The use of bone health screening to identify surgical patients at high risk of osteoporosis for preoperative DXA. J Bone Miner Res 37(Suppl 1). Available at: asbmr.org/ItineraryBuilder/PresentationDetail.aspx?pid=faa80886-50fa-454c-88a9-
Borchardt G, Nickel B, Andersen Lucas, Hetzel Scott, Illgen R, Hennessy D, Anderson P, Binkley N, Krueger D (2022) Custom femur and tibia BMD measurement in elective total knee arthroplasty candidates. J Clin Densitom S1094-6950(22)00006-3. https://doi.org/10.1016/j.jocd.2022.01.004
Anderson PA, Jeray KJ, Lane JM, Binkley NC (2019) Bone health optimization: beyond own the bone: AOA critical issues. J Bone Joint Surg Am 101:1413–1419
Kadri A, Binkley N, Hare KJ, Anderson PA (2020) Bone health optimization in orthopaedic surgery. J Bone Joint Surg Am 102:574–581
Khatod M, Inacio MC, Dell RM, Bini SA, Paxton EW, Namba RS (2015) Association of bisphosphonate use and risk of revision after THA: outcomes from a US total joint replacement registry. Clin Orthop Relat Res 473:3412–3420
Namba RS, Inacio MC, Cheetham TC, Dell RM, Paxton EW, Khatod MX (2016) Lower total knee arthroplasty revision risk associated with bisphosphonate use, even in patients with normal bone density. J Arthroplasty 31:537–541
Misch CE (1999) Bone density: a key determinant for clinical success. In: Misch CE (ed) Contemporary implant dentistry, 2nd edn. Mosby Company, St. Louis, pp 109–118
Norton MR, Gamble C (2001) Bone classification: an objective scale of bone density using the computerized tomography scan. Clin Oral Implants Res 12:79–84
Oh JS, Kim SG (2012) Clinical study of the relationship between implant stability measurements using Periotest and Osstell mentor and bone quality assessment. Oral Surg Oral Med Oral Pathol Oral Radiol 113:e35-40
Lee S, Gantes B, Riggs M, Crigger M (2007) Bone density assessments of dental implant sites: 3. Bone quality evaluation during osteotomy and implant placement. Int J Oral Maxillofac Implants 22:208–212
Rokn A, RasouliGhahroudi AA, Daneshmonfared M, Menasheof R, Shamshiri AR (2014) Tactile sense of the surgeon in determining bone density when placing dental implant. Implant Dent 23:697–703
Randall C, Bridges D, Guerri R et al (2013) Applications of a new handheld reference point indentation instrument measuring bone material strength. J Med Device 7:410051–410056
Hoppe S, Uhlmann M, Schwyn R, Suhm N, Benneker LM (2015) Intraoperative mechanical measurement of bone quality with the DensiProbe. J Clin Densitom 18:109–116
Tulner SAF, Zdravkovic V, Külling F, Jost B, Puskas GJ (2017) Haptic assessment of bone quality in orthopedic surgery: no consensus but perspective for high training potential. Int J Med Educ 8:437–438
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nickel, B., Krueger, D., Borchardt, G. et al. Intraoperative physician assessment of bone: correlation to bone mineral density. Osteoporos Int 34, 1093–1099 (2023). https://doi.org/10.1007/s00198-023-06729-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06729-3