Abstract
Summary
Bisphosphonates prevent future hip fractures. However, we found that one in six patients with hip fractures had a delay in bisphosphonate initiation and another one-sixth discontinued treatment within 12 months after discharge. Our results highlight the need to address hesitancy in treatment initiation and continuous monitoring.
Purpose
Suboptimal antiresorptive use is not well understood. This study investigated trajectories of oral bisphosphonate use following first hip fractures and factors associated with different adherence and persistence trajectories.
Methods
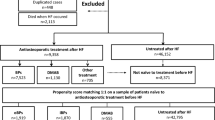
We conducted a retrospective study of all patients aged ≥ 50 years dispensed two or more bisphosphonate prescriptions following first hip fracture in Victoria, Australia, from 2012 to 2017. Twelve-month trajectories of bisphosphonate use were categorized using group-based trajectory modeling. Factors associated with different trajectories compared to the persistent adherence trajectory were assessed using multivariate multinomial logistic regression.
Results
We identified four patterns of oral bisphosphonate use in 1811 patients: persistent adherence (66%); delayed dispensing (17%); early discontinuation (9%); and late discontinuation (9%). Pre-admission bisphosphonate use was associated with a lower risk of delayed dispensing in both sexes (relative risk [RR] 0.28, 95% confidence interval [CI] 0.21–0.39). Older patients (\(\ge\) 85 years old versus 50–64 years old, RR 0.38, 95% CI 0.22–0.64) had a lower risk of delayed dispensing. Males with anxiety (RR 9.80, 95% CI 2.24–42.9) and females with previous falls had increased risk of early discontinuation (RR 1.80, 95% CI 1.16–2.78).
Conclusion
Two-thirds of patients demonstrated good adherence to oral bisphosphonates over 12 months following hip fracture. Efforts to further increase post-discharge antiresorptive use should be sex-specific and address possible persistent uncertainty around delaying treatment initiation.
Similar content being viewed by others
Introduction
Osteoporotic fractures are associated with significant disability, morbidity, and mortality. Hip fractures are responsible for considerable clinical and economic burden to individuals and the society [1, 2]. A recent projection based on data from 20 countries suggested the number of hip fractures will double from 2018 to 2050 [3]. The absolute number of hip fractures increased by 20% from 2012 to 2018 in Victoria, Australia [4].
Bisphosphonates are recommended as first-line treatment for patients with radiologically confirmed osteoporosis or following a minimal trauma fracture [5,6,7]. However, despite their established cost-effectiveness, bisphosphonates remain under-utilized [8, 9]. Undertreatment may arise from fear of possible negative impacts on fracture healing [10] or low treatment adherence and persistence [11]. Delayed dispensing may result in a missed opportunity for fracture prevention because the risk of second fracture is highest soon after the first fracture [12, 13], whereas non-adherence and non-persistence have been associated with up to a 40% increase in fracture risk [14]. Understanding the different trajectories of bisphosphonate use following fractures allows clinicians and policy makers to develop targeted strategies to address the longstanding problem of bisphosphonate underutilization.
Most studies on bisphosphonate adherence have used the medication possession ratio to dichotomize patients as adherent or non-adherent using various cut-offs [11]. More granular longitudinal understanding of bisphosphonate use after hip fracture is lacking. Group-based trajectory modeling is a useful agnostic epidemiological tool for identifying different trajectories of medication use based on similarities in actual dispensing patterns [15, 16].
The objective of our study was to investigate trajectories of oral bisphosphonate use following first hip fractures and factors associated with different adherence and persistence trajectories by using population-based linked datasets. The factors investigated included patient demographics, residence, comorbidities, polypharmacy, previous falls, osteoporosis diagnosis, and prior bisphosphonate use [11, 17, 18].
Methods
Data sources
Our population-based cohort study used linked data from the Victorian Admitted Episodes Dataset (VAED), Pharmaceutical Benefits Scheme (PBS), and National Death Index (NDI). VAED are routinely collected administrative data for all public and private hospital episodes in Victoria, Australia. The dataset contains comprehensive information on demographics, diagnoses, admission sources, and discharge destinations. Records for readmission within 1 day of discharge were combined with original admission as a single continuous hospitalization to account for transfers between hospitals. Hip fracture ascertainment using Australian administrative hospital data has a sensitivity (i.e., proportion of hip fractures captured in administrative data) around 95% and positive predictive value (i.e., proportion of recorded hip fractures were a new hip fracture) above 70% [19]. We restricted our investigation to first hip fracture to minimize false positives due to misclassification of subsequent episodes of care as new hip fractures. The PBS dataset contains information on pharmacy claims made by all Australian residents for medications subsidized by the Australian Government. This dataset contains records of medications dispensed at all community pharmacies, outpatient clinics and at hospital discharge. The PBS dataset does not contain information of medications dispensed during a hospitalization. NDI contains information on all deaths registered across Australia. Data from VAED and PBS were available from 1 July 2006 to 30 June 2018, whereas data from NDI were available from 1 July 2012 to 30 June 2018. Details on the datasets have been published previously [4].
Study population
All patients aged 50 years or above and discharged from any public or private hospital in Victoria between 1 July 2012 and 30 June 2017 following hip fractures were included. Patients with a principal diagnosis of hip fracture (International Statistical Classification of Diseases and Related Health Problems, Tenth Revision, Australian Modification [ICD-10-AM] S72.0-S72.2) [19,20,21,22] were included. Patients with a hip fracture or cancer diagnosis (ICD-10-AM C00-C99) within 5 years prior to the index hip fracture were excluded to ensure we investigated incident hip fractures and their bisphosphonate use were not affected by other indications (e.g., bone metastases or hypercalcemia). To avoid including patients who discontinued due to intolerance after their first dose, our study included patients with at least 2 dispensings of any oral bisphosphonates (World Health Organization Anatomical Therapeutic Chemical Classification [ATC] M05BA04, M05BA07, M05BB02-M05BB07) within 12 months after discharge. Patients dispensed other osteoporosis medications (i.e., denosumab [ATC M05BX04], zoledronic acid [ATC M05BA08, M05BB08], and raloxifene [ATC G03XC01]) within the follow-up period were excluded. Patients dispensed denosumab within 6 months before discharge were also excluded to avoid including patients not initiated on bisphosphonates at discharge for this reason. Patients who died within 12 months after discharge were excluded [23, 24]. Patients who were hospitalized for more than 1 month in the 12 months post-discharge were also excluded to avoid missing data from lack of inpatient dispensing data.
Trajectories determination
Dispensings of oral bisphosphonates were ascertained for each 30-day period after discharge for 12 months. Each oral bisphosphonate dispensing in Australia represents 30 days’ supply. If there were two or more bisphosphonate dispensings in a 30-day period, the extra prescriptions were carried forward to the subsequent months for which there was no dispensing. Trajectories of oral bisphosphonate use were identified by group-based trajectory modeling with SAS PROC TRAJ [25]. The number of trajectories was first determined using the highest order possible with the procedure, which allows the maximum number of inflection points thus flexibility in fitting each trajectory [15]. Bayesian information criterion (BIC) across all models was compared and models with less negative BIC were preferred (Supplemental Table 1) [15]. A model with 4 trajectories was chosen as any larger number of trajectories did not provide stratification of clinical significance. Different orders for each trajectory were then explored (Supplemental Table 2). Average posterior probability of group membership (AvePP) and odds of correct classification (OCC) for each trajectory were calculated to evaluate adequacy of the models [15]. The final best-fitting model was chosen based on the following criteria: (a) AvePP > 0.7, (b) OCC > 5, (c) the highest order parameter of each trajectory was statistically significant, (d) the group proportions estimated by the model was similar to the actual proportions of individuals assigned to each group based on their maximum posterior probability, (e) the BIC, (f) parsimony principle, and (g) clinical judgement (Supplemental Table 2) [15].
Factors associated with trajectories
We investigated factors that have been associated with adherence and persistence to oral bisphosphonates in previous research, including selected comorbidities related to cognitive, mental, and gastrointestinal health [11]. We also investigated factors that were associated with 1-year mortality following hip fracture in our previous research [4]. These factors included age, sex, discharge to residential aged care facilities (RACF), and frailty [4]. Frailty was assessed using the validated Hospital Frailty Risk Score (HFRS), a weighted score of 109 diagnoses recorded within 2 years prior to discharge [26]. Patients were categorized as having low frailty risk (HFRS < 5), intermediate frailty risk (HFRS 5–15), and high frailty risk (HFRS > 15) [26]. Comorbidities were identified from ICD-10-AM diagnosis codes recorded within 5 years prior to discharge. Previous falls and previous osteoporosis were identified from ICD-10-AM diagnoses recorded within 5 years prior to admission. A 5-year lookback period was used to improve the detection of comorbidities across multiple hospitalizations for each patient. This was because not all comorbidities may have been recorded at the index hospitalization. Pre-admission bisphosphonate use (any oral bisphosphonate dispensing within 6 months prior to admission) and pre-admission polypharmacy (5 or more different medications dispensed within 60 days prior to admission) were also assessed. Factors associated with different trajectories compared to the persistent adherence trajectory were assessed using multivariate multinomial logistic regression. The model was adjusted for age, sex, discharge to RACF, HFRS, comorbidities, previous falls, previous osteoporosis diagnosis, pre-admission bisphosphonate use, and pre-admission polypharmacy. Statistical significance was defined as p-value < 0.05. All analyses were performed using SAS (version 9.4) and R (version 4.0.0). As management of osteoporosis is sex-specific, sex-stratified subgroup analysis was performed to examine any differences across sex in bisphosphonate use after hip fractures. Sensitivity analysis was conducted to explore the possible effect of subsequent fractures on the analysis by excluding patients with second hip fractures from the multivariate multinomial logistic regression.
Ethics
The study was approved by Australian Institute of Health and Welfare Ethics Committee (EO2018-4–468) and Monash University Human Research Ethics Committee (14,339).
Results
Among 13,112 patients hospitalized for hip fractures and eligible for evaluation of oral bisphosphonate use, 1811 patients dispensed \(\ge\) 2 prescriptions were included for trajectories evaluation (Supplemental Fig. 1). Among these included patients, 80% (n = 1439) were females, 77% (n = 1395) were 75 years or older, and 14% (n = 244) were discharged to RACF. The majority (72%, n = 1300) had intermediate frailty risk (HFRS 5–15) at discharge, while 16% (n = 290) had low frailty risk (HFRS < 5) and 12% (n = 221) had high frailty risk respectively. Overall, 43% (n = 775) had oral bisphosphonates dispensed within 6 months pre-admission. The median (interquartile range) number of medications dispensed within 60 days pre-admission was 6 (3–8) and 62% (n = 1117) of patients had pre-admission polypharmacy (Table 1).
Trajectories of bisphosphonate use
The four trajectories identified by group-based trajectory modeling were labelled as “persistent adherence,” “delayed dispensing,” “early discontinuation,” and “late discontinuation.” The proportions of patients that were categorized into the different trajectories were 66% (n = 1191), 17% (n = 305), 9% (n = 161), and 9% (n = 154) respectively. Patients with “persistent adherence” had > 80% probability of monthly bisphosphonate dispensing throughout the 12 months. The probability of dispensing bisphosphonates for patients with “delayed dispensing” was low initially and increased to 50% at 6 months after discharge. The probability of bisphosphonate dispensing for patients with “early discontinuation” and “late discontinuation” decreased to 50% at around 3 and 8 months respectively (Fig. 1 and Supplemental Table 3).
Factors associated with trajectories
Patients aged 85 years or older and patients with intermediate frailty risk (HFRS 5–15) were more likely to have persistent adherence, as evidenced by their lower risk of delayed dispensing (\(\ge\) 85 years old versus 50–64 years old: relative risk [RR] 0.38, 95% confidence interval [CI] 0.22–0.64; HFRS 5–15 VS HFRS < 5: RR 0.66, 95% CI 0.47–0.93). In addition, patients who were on bisphosphonates pre-admission had a lower risk of delayed dispensing (RR 0.28, 95% CI 0.21–0.39). Patients with dementia were at higher risk of late discontinuation when compared with persistent adherence (RR 1.92, 95% CI 1.09–3.38), while patients with anxiety disorder had a higher risk of early discontinuation (RR 1.92, 95% CI 1.08–3.43) (Table 2).
When stratified by sex, females aged 85 years or older were more likely to have persistent adherence, as demonstrated by their lower risk of delayed dispensing (RR 0.39, 95% CI 0.21–0.72). However, there was no difference for males aged 85 years or older (RR 0.35, 95% CI 0.12–1.03). However, the estimates remained similar. Similarly, females but not males with intermediate frailty risk were more likely to display persistent adherence, as evidenced by their lower risk of delayed dispensing (females: RR 0.68, 95% CI 0.46–1.00; males: RR 0.57, 95% CI 0.26–1.24) with intermediate frailty risk. For patients who were on bisphosphonates pre-admission, decreased risks remained evident for delayed dispensing in both sexes (males: RR 0.17, 95% CI 0.06–0.49; females: RR 0.30, 95% CI 0.21–0.42). Higher risk of early discontinuation for patients with history of anxiety disorder remained significant for males (RR 9.81, 95% CI 2.24–42.9) but was not evident in females (RR 1.37, 95% CI 0.69–2.70). Additionally, females hospitalized for falls previously had higher risk of early discontinuation (RR 1.80, 95% CI 1.16–2.78). Higher risk of late discontinuation in patients with dementia became insignificant for both males (RR 1.82 95% CI 0.49–6.78) and females (RR 1.89 95% CI 1.00–3.58) (Tables 3 and 4).
Sex, type of residence, history of depression, gastroesophageal reflux, previous osteoporosis diagnosis, and pre-admission polypharmacy were not associated with different trajectories in both main and sex-stratified analyses (Tables 2, 3, and 4). Sensitivity analysis excluding patients with second hip fractures from the analyses produced similar results for both overall and sex-stratified analyses. The study is reported in accordance with STROBE statement (Supplemental Table 4) [27].
Discussion
The main finding of our study was that two-thirds of patients demonstrated persistent adherence over 12 months following their first hip fracture. However, one-sixth of patients had delayed dispensing following discharge. Older age, increased frailty, and pre-admission bisphosphonate use were associated with lower risk of delayed dispensing. The remaining one-sixth of patients discontinued early or late over the 12-month post-discharge. Males with anxiety disorder and females with previous falls were associated with increased risk of early discontinuation.
The proportion of patients with persistent adherence was higher than for other chronic medications [28]. For example, 55% of older adults using statins in Australia were non-adherent and 45% discontinued their statins within 12 months [29]. Our study was comparable to a recent systematic review which revealed 12-month persistence was within the 18–75% range [11]. The high proportion of patients with persistent adherence may be because their recent hip fracture reinforced the need for adherence to prophylactic treatment. Another reason may be that patients at risk of non-adherence were preferentially prescribed denosumab, which has been shown to be associated with better adherence [30].
One in six patients had delayed dispensing. Primary non-adherence (i.e., a delay in having a prescription dispensed) may have contributed to this observed delay. However, despite a meta-analysis reporting that primary non-adherence was prevalent for osteoporosis medications [31], an Australian study reported that around 95% of patients filled their first antiresorptive prescription within 1 month [32]. Clinicians’ fear of bisphosphonates slowing bone healing may have also contributed to the observed delay. However, recent systematic reviews suggest initiating bisphosphonates soon after fracture does not lead to adverse outcomes [33, 34]. During our study period, Australian guidelines recommended patients receive dental assessment prior to initiating bisphosphonates [6, 7]. This may have also contributed to the observed delay. Older Australians visit dentists more frequently than younger Australians [35], which may partly explain why older patients were less likely to have delayed dispensing. Clinical inertia (i.e., failure to initiate or intensify therapy when indicated) [36] may have also contributed to the observed delay. Higher perceived risk of fracture in patients with intermediate frailty may decrease clinical inertia. The absence of clinical inertia in patients already taking bisphosphonates may explain the reduced risk of delayed dispensing. Education addressing the risks of bisphosphonates and fractures following minimal-trauma fractures is needed to reduce apparent prescribing hesitancy.
Another one-sixth of patients did not persist with bisphosphonates over 12 months. More than half of these patients discontinued soon after discharge. Pre-admission bisphosphonate use had minimal effect on early or late discontinuation. This was largely consistent with a recent study that demonstrated pre-admission bisphosphonate users had different adherence patterns after fractures [37]. Males with history of anxiety were more likely to discontinue early, which is consistent with a previous study that reported anxiety was associated with medication non-adherence [38]. The greater disability experienced by males with anxiety may partly explain the differential effect across sex [39]. On the other hand, females, but not males, with previous falls had increased risk of early discontinuation. This may be because more osteoporosis guidelines focus on treating post-menopausal women [5], leading to more females than males being prescribed with bisphosphonates after a previous fall. Our results highlight the importance of sex-specific initiatives to improve bisphosphonate use during early post-fracture follow-up.
One-tenth of patients discontinued more than 6 months after discharge. Patients with dementia had increased risk of late discontinuation, which may result from cognitive impairment, lack of contact with medical specialists such as endocrinologists, or change in the goals of care [40, 41]. Our results underscore the importance of understanding the benefits and risks of ongoing treatment in people with dementia.
Strengths and limitations
Strengths of our study include the use of linked administrative health data for all patients with hip fracture in Victoria [42]. Our group-based trajectory modeling was based on 30-day dispensing rather than prescription data or 60-day or 90-day dispensing. Group-based trajectory modeling was an agnostic approach to identify trajectories which avoided potential bias arising from defining adherence using arbitrary cut-offs or dichotomization of patients [16, 43, 44]. Particularly, our model identified patients with delayed dispensing and late discontinuation. These dispensing patterns would not have been evident had we calculated the possession ratio (MPR), another adherence measure with common cut-offs of low (MPR < 0.5), moderate (MPR 0.5 to < 0.8), and high (MPR 0.80 to 1.00) adherence. Our study allowed identification of risks factors for bisphosphonate use patterns that would have been obscured otherwise. Another strength of our study is our stringent inclusion and exclusion criteria. By including only those with at least 2 dispensings of bisphosphonate and excluding patients who used other anti-osteoporosis medications during follow-up, our results are not biased by patients who discontinued due to intolerance or contraindications or those who switched to other anti-osteoporosis medications.
While this study included the entire population in Victoria, Australia, one limitation of our study is that it may not be generalizable to other populations. Patterns of bisphosphonate use may be different in other populations due to differences in guidelines around medication selection, initiation, availability of dental examination, and medication reimbursement criteria. Other limitations include we only included patients dispensed two or more oral bisphosphonate prescriptions and did not investigate the characteristics of patients not initiated on bisphosphonates. While we adjusted for pre-admission bisphosphonate use in our analysis, we did not account for the duration of previous use. Our study also did not investigate the use of parenteral antiresorptives (e.g., denosumab, zoledronic acid) because of their different dosing and dispensing frequencies. We did not exclude patients dispensed zoledronic acid within 1 year prior to discharge. However, we do not anticipate this would result in significant overestimation of delayed dispensing because oral bisphosphonates and denosumab are the most common antiresorptives in Australia [6]. Misclassification bias, common in administrative data, is also present in our study. However, data quality was maximized with regular Australian Government data integrity audits [45] and our frequent monthly data also minimized the effect of single dispensing on trajectory determination. It was a strength of our study that we used a 5-year lookback period to maximize detection of comorbidities. However, we acknowledge that this may have led to the inclusion of comorbid conditions that were no longer acutely symptomatic. We were also not able to investigate why patients exhibit their respective trajectories. However, this may be partly related to patients’ beliefs regarding the benefits and harms of medications, which have been demonstrated to impact adherence [46].
Conclusion
In conclusion, two-thirds of patients had persistent adherence to oral bisphosphates over 12 months following hip fracture. However, one-sixth of patients had delayed dispensing and another one-sixth had early or late discontinuation. Efforts to further increase post-discharge antiresorptive use should be sex-specific and address possible persistent uncertainty around delaying treatment initiation.
Data Availability
Restrictions apply to the availability of all data generated and analyzed during this study to preserve patient confidentiality. By Australian legislation, individual patient level data cannot be made publicly available.
References
Liu J, Gong T, Xu X, Fox KM, Oates M, Gandra SR (2022) Heavy clinical and economic burden of osteoporotic fracture among elderly female Medicare beneficiaries. Osteoporos Int 33:413–423
Wu AM, Bisignano C, James SL et al (2021) Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev 2:e580–e592
Sing CW, Lin TC, Bartholomew S et al (2023) Global epidemiology of hip fractures: secular trends in incidence rate, post-fracture treatment, and all-cause mortality. J Bone Miner Res 38:1064–1075
Leung MTY, Marquina C, Turner JP, Ilomaki J, Tran T, Bell JS (2023) Hip fracture incidence and post-fracture mortality in Victoria, Australia: a state-wide cohort study. Arch Osteoporos 18:56
American College of Obstetricians and Gynecologists (2022) Management of postmenopausal osteoporosis. Obstet Gynecol 139:698–717
Bone and Metabolism Expert Group (published 2019 Jun; amended 2022 Aug) Osteoporosis and minimal-trauma fracture. In: Therapeutic guidelines: Bone and Metabolism. Therapeutic Guidelines Limited, Melbourne
The Royal Australian College of General Practitioners and Osteoporosis Australia (2017) Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age. 2nd edn. The Royal Australian College of General Practitioners, East Melbourne, VIC
Compston J (2020) Reducing the treatment gap in osteoporosis. Lancet Diabetes Endocrinol 8:7–9
Milat F, Ebeling PR (2016) Osteoporosis treatment: a missed opportunity. Med J Aust 205:185–190
Molvik H, Khan W (2015) Bisphosphonates and their influence on fracture healing: a systematic review. Osteoporos Int 26:1251–1260
Fatoye F, Smith P, Gebrye T, Yeowell G (2019) Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 9:e027049
Johansson H, Siggeirsdóttir K, Harvey NC, Odén A, Gudnason V, McCloskey E, Sigurdsson G, Kanis JA (2017) Imminent risk of fracture after fracture. Osteoporos Int 28:775–780
Johnell O, Kanis JA, Odén A, Sernbo I, Redlund-Johnell I, Petterson C, De Laet C, Jönsson B (2004) Fracture risk following an osteoporotic fracture. Osteoporos Int 15:175–179
Ross S, Samuels E, Gairy K, Iqbal S, Badamgarav E, Siris E (2011) A meta-analysis of osteoporotic fracture risk with medication nonadherence. Value Health 14:571–581
Nagin DS (2005) Group-based modeling of development. Harvard University Press, Cambridge
Alhazami M, Pontinha VM, Patterson JA, Holdford DA (2020) Medication adherence trajectories: a systematic literature review. J Manag Care Spec Pharm 26:1138–1152
Yap AF, Thirumoorthy T, Kwan YH (2016) Systematic review of the barriers affecting medication adherence in older adults. Geriatr Gerontol Int 16:1093–1101
Strampel W, Emkey R, Civitelli R (2007) Safety considerations with bisphosphonates for the treatment of osteoporosis. Drug Saf 30:755–763
Thuy Trinh LT, Achat H, Loh SM, Pascoe R, Assareh H, Stubbs J, Guevarra V (2018) Validity of routinely collected data in identifying hip fractures at a major tertiary hospital in Australia. Health Inf Manag 47:38–45
Llopis-Cardona F, Armero C, Hurtado I, García-Sempere A, Peiró S, Rodríguez-Bernal CL, Sanfélix-Gimeno G (2022) Incidence of subsequent hip fracture and mortality in elderly patients. A multistate population-based cohort study in Eastern Spain. J Bone Miner Res 37:1200–1208
Walsh ME, Ferris H, Coughlan T, Hurson C, Ahern E, Sorensen J, Brent L (2021) Trends in hip fracture care in the Republic of Ireland from 2013 to 2018: results from the Irish Hip Fracture Database. Osteoporos Int 32:727–736
Australian Institute of Health Welfare (2018) Hip fracture incidence and hospitalisations in Australia 2015–16. Cat. no. PHE 226. Australian Institute of Health Welfare, Canberra
Deardorff WJ, Cenzer I, Nguyen B, Lee SJ (2022) Time to benefit of bisphosphonate therapy for the prevention of fractures among postmenopausal women with osteoporosis: a meta-analysis of randomized clinical trials. JAMA Intern Med 182:33–41
Friesen KJ, Bugden S, Falk J (2020) Time to benefit and the long-term persistence of new users of oral bisphosphonates. J Bone Miner Metab 38:371–377
Jones BL, Nagin DS, Roeder K (2001) A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res 29:374–393
Gilbert T, Neuburger J, Kraindler J et al (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391:1775–1782
Vandenbroucke JP, Ev Elm, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, Poole C, Schlesselman JJ, Egger M (2007) Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Ann Intern Med 147:163–194
World Health Organization (2003) Adherence to long-term therapies: evidence for action. World Health Organization, Geneva
Ofori-Asenso R, Ilomäki J, Tacey M, Si S, Curtis AJ, Zomer E, Bell JS, Zoungas S, Liew D (2019) Predictors of first-year nonadherence and discontinuation of statins among older adults: a retrospective cohort study. Br J Clin Pharmacol 85:227–235
Morizio P, Burkhart JI, Ozawa S (2018) Denosumab: a unique perspective on adherence and cost-effectiveness compared with oral bisphosphonates in osteoporosis patients. Ann Pharmacother 52:1031–1041
Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J (2019) Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pract 73:e13350
Australian Institute of Health and Welfare (2011) Use of antiresorptive agents for osteoporosis management. AIHW, Canberra
Barton DW, Smith CT, Piple AS, Moskal SA, Carmouche JJ (2020) Timing of bisphosphonate initiation after fracture: what does the data really say? Geriatr Orthop Surg Rehabil 11:2151459320980369
Gao Y, Liu X, Gu Y, Song D, Ding M, Liao L, Wang J, Ni J, He G (2021) The effect of bisphosphonates on fracture healing time and changes in bone mass density: a meta-analysis. Front Endocrinol (Lausanne) 12:688269
Brennan D, Chrisopoulos S, Do L, Ellershaw A, Luzzi L, Peres M (2019) Australia’s oral health: national study of adult oral health 2017–18. The University of Adelaide, South Australia, Adelaide
Phillips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, Miller CD, Ziemer DC, Barnes CS (2001) Clinical inertia. Ann Intern Med 135:825–834
Kline GA, Morin SN, Lix LM, Leslie WD (2022) Divergent patterns of antifracture medication use following fracture on therapy: a population-based cohort study. J Clin Endocrinol Metab 107:491–499
Sundbom LT, Bingefors K (2013) The influence of symptoms of anxiety and depression on medication nonadherence and its causes: a population based survey of prescription drug users in Sweden. Patient Prefer Adherence 7:805–811
Ferrari AJ, Norman RE, Freedman G et al (2014) The burden attributable to mental and substance use disorders as risk factors for suicide: findings from the Global Burden of Disease Study 2010. PLoS ONE 9:e91936
Maxwell CJ, Stock K, Seitz D, Herrmann N (2014) Persistence and adherence with dementia pharmacotherapy: relevance of patient, provider, and system factors. Can J Psychiatry 59:624–631
El-Saifi N, Moyle W, Jones C, Tuffaha H (2018) Medication adherence in older patients with dementia: a systematic literature review. J Pharm Pract 31:322–334
Australian Institute of Health Welfare (2022) Health system overview. AIHW, Canberra
Hawley CE, Lauffenburger JC, Paik JM, Wexler DJ, Kim SC, Patorno E (2022) Three sides to the story: adherence trajectories during the first year of SGLT2 inhibitor therapy among Medicare beneficiaries. Diabetes Care 45:604–613
Rodríguez-Bernal CL, Sánchez-Saez F, Bejarano-Quisoboni D, Hurtado I, García-Sempere A, Peiró S, Sanfélix-Gimeno G (2022) Assessing concurrent adherence to combined essential medication and clinical outcomes in patients with acute coronary syndrome. A population-based, real-world study using group-based trajectory models. Front Cardiovasc Med 9:863876
Victorian Agency for Health Information (2022) Health data integrity program. https://vahi.vic.gov.au/ourwork/health-data-integrity-program Accessed 1 December 2022
Pepe J, Cipriani C, Cecchetti V, Ferrara C, Della Grotta G, Danese V, Colangelo L, Minisola S (2019) Patients’ reasons for adhering to long-term alendronate therapy. Osteoporos Int 30:1627–1634
Acknowledgements
The authors gratefully acknowledge the Centre for Victoria Data Linkage and Australian Institute of Health and Welfare for provision of the data.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions This study was financially supported by the Dementia Australia Research Foundation – Yulgilbar Innovation Grant. MTYL is supported by Australian Government Research Training Scholarship. JSB is supported by a National Health and Medical Research Council (NHMRC) Dementia Leadership Fellowship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
MTYL, JPT, CM, and TT have nothing to declare. JI has received grant or consulting funds from the National Health and Medical Research Council, Medical Research Future Fund, Dementia Australia Research Foundation, Yulgilbar Foundation, National Breast Cancer Foundation, AstraZeneca, and Amgen unrelated to this work. JSB has received grant funding or consulting funds from the National Health and Medical Research Council, Medical Research Future Fund, Victorian Government Department of Health and Human Services, Dementia Australia Research Foundation, Yulgilbar Foundation, Aged Care Quality and Safety Commission, Dementia Centre for Research Collaboration, Pharmaceutical Society of Australia, Society of Hospital Pharmacists of Australia, GlaxoSmithKline Supported Studies Programme, Amgen, and several aged care provider organizations unrelated to this work. All grants and consulting funds were paid to the employing institution.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Leung, M.T.Y., Turner, J.P., Marquina, C. et al. Trajectories of oral bisphosphonate use after hip fractures: a population-based cohort study. Osteoporos Int 35, 669–678 (2024). https://doi.org/10.1007/s00198-023-06974-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06974-6