Abstract
Introduction
Osteoporosis is a major disease state associated with significant morbidity, mortality, and health care costs. Less than half of the individuals sustaining a low energy hip fracture are diagnosed and treated for the underlying osteoporosis.
Objective
A multidisciplinary Canadian hip fracture working group has developed practical recommendations to meet Canadian quality indicators in post hip fracture care.
Methods
A comprehensive narrative review was conducted to identify and synthesize key articles on post hip fracture orthogeriatric care for each of the individual sections and develop recommendations. These recommendations are based on the best evidence available today.
Conclusion
Recommendations are anticipated to reduce recurrent fractures, improve mobility and healthcare outcomes post hip fracture, and reduce healthcare costs. Key messages to enhance postoperative care are also provided.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In response to the American Society for Bone and Mineral Research (ASBMR) [1], international call to action to address the low rate of diagnosis and treatment of osteoporosis post hip fracture a Canadian multi-disciplinary group has developed recommendations addressing post hip fracture care. The goal is to meet the Canadian quality indicators [2] and provide the best evidence-based strategies for care following a low trauma hip fracture from an orthopedic, geriatric medicine, and rehabilitation perspective. These recommendations are expected to reduce recurrent fractures and improve mobility and healthcare outcomes as well as healthcare costs.
This Canadian position paper outlining post hip fracture orthogeriatric care addresses the challenges and best practice strategies in Canada. It supports the global efforts of the International Osteoporosis Foundation (IOF) [3] in its goal to ensure effective pharmacologic intervention following fragility fracture with the launch of the IOF Capture the Fracture [4] initiative. The new Capture the Fracture Partnership in fact aims to reduce the incidence of hip and vertebral fractures due to osteoporosis by 25% by 2025 [4]. It also supports the initiatives of the Fragility Fracture Network (FFN) [5], which has emphasized the value of multi-disciplinary care with an orthogeriatric perspective focusing on early rehabilitation following a fragility fracture. The FFN also emphasizes the value of reliable secondary prevention, reducing falls risk and addressing bone health following a fragility fracture (FFN—four pillars).
This manuscript was developed by a team of multidisciplinary experts in post-fracture care. The patient perspective has also been captured and the document was reviewed and approved by the Bone Research and Education Center patient support program.
Key messages to enhance post-operative care are also provided.
Methodology
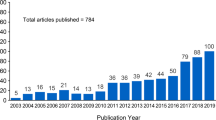
A comprehensive narrative review of the literature was conducted to identify and synthesize key articles on post hip fracture orthogeriatric care for each of the individual sections. Multiple search terms for each section were included (for example, emergency department, post hip fracture, and orthogeriatric care). Hand searching of reference lists of relevant articles was also conducted. We included articles with the following criteria (1) adults aged 50 years and older; (2) described care delivered to patients undergoing surgery for hip fracture including preoperative assessment, anesthesia management, surgery, pain management, post-operative management, osteoporosis management, nutrition, and rehabilitation; (3) randomized control trials (RCT), observational studies, systematic reviews, and guideline publications; and (4) English language articles. No limitations were placed on publication date to provide a comprehensive summary of current knowledge. Findings are summarized for each section below. This report is also guided by key quality indicators for hip fracture care provided by Health Quality Ontario (HQO) and Alberta Health Services (AHS) [2, 6].
Results
Emergency department management
The early recognition and initiation of treatment of patients with hip fractures in the emergency room optimizes care. A number of “Fast-Track” pathways have been developed that allow patients with suspected hip fractures to receive adequate analgesia, early optimization and rapid diagnosis, and ensure timely care [7]. Early diagnosis and transfer to an appropriate inpatient bed is required, as it may reduce the risk of pressure ulcers from prolonged periods of immobilization in emergency room stretchers. Pre-operative traction in this setting is of no increased benefit [8].
Multi-disciplinary care in the preoperative setting allows for rapid medical optimization and has the potential to reduce delays to surgery, incidence of delirium, and in-patient mortality [9, 10]. An orthogeriatric care model with co-management by orthopedic surgeons and clinicians with expertise in the care of geriatric patients has gained traction in recent years [11,12,13]. Co-management models have been shown to reduce the time to surgery and mortality rates in hip fracture patients [9]. Standardized pre-operative order sets should be initiated upon diagnosis in the emergency department. Standardized order sets and care pathways expedite care, reduce medical errors, and improve preoperative pain management [14]. Key pre-operative assessments should include a pre-fracture functional status, evaluation of fluid balance, cognitive and delirium screening, preoperative bloodwork, electrocardiography, and evaluation of home medications [15].
Surgery within 48 h
The evidence supporting timely surgery for patients with hip fractures has grown in recent years. Following a hip fracture, patients often experience significant pain, blood loss, and a period of immobilization. This inciting event leads to a hyper-coagulable, catabolic stress state that increases the risk of serious perioperative complications [16,17,18]. It is thought that timely surgical care shortens the exposure to this harmful state, reducing the risk of perioperative morbidity and mortality. Population-based cohort data from Ontario demonstrates that surgery within 24 h from presentation to hospital significantly reduces the overall mortality rate and risk of complications [19]. A recent RCT demonstrated that early surgery reduced mortality in high risk patients with elevated preoperative troponin levels [20]. If surgery is delayed for more than 12 h from the time of hospital admission, it is recommended that thromboprophylaxis be started pre-operatively with low molecular weight heparin (LMWH) [20, 21].
Early surgery in this population requires coordination among several medical and surgical specialists and allied health staff and administrators. Standardized protocols, order sets, and dedicated hip fracture care pathways are imperative to ensure that patients who have sustained a hip fracture receive surgery within 48 h of arriving to the hospital and as soon as possible [10]. Although a recent RCT found that “accelerated surgery” for hip fracture, i.e., within 12 h of arrival at hospital, did not significantly result in a reduction in death or a composite of major complications compared with “standard care” [20], it has been established that early surgery within 24–48 h has proven benefits [10, 19] and this approach has been widely adopted. Surgery should not be delayed if possible for patients on anticoagulation as the risks of delayed surgery outweigh the risks of intraoperative bleeding [22, 23]. Recent meta-analyses have identified that hip fracture patients who present on oral anti-coagulants have significantly delayed time-to-surgery and this is related to higher mortality rates [24, 25]. Hip fracture care pathways are being studied and there is increasing support for safe and early coordinated medical and surgical care for patients with hip fractures presenting on pre-injury anti-coagulation [26].
Multi-modal analgesia/nerve blocks
In addition to around the clock simple analgesia such as acetaminophen, regional nerve blocks can be a safe adjunctive method to improve pain management in patients with hip fractures. They have been shown to decrease opioid use and reduce the rate and length of delirium while also decreasing the length of stay in the hospital [27,28,29]. When done early, they can also assist with decreasing the time to mobility while also increasing functional walking distance [27]. This can be done and supplemented with other modes of analgesia as well to provide optimal pain relief for the patient.
The most common blocks are the femoral nerve block and the fascia iliaca compartment block (FICB). Both have been shown to be effective in providing analgesia to patients and can be done as a single-shot injection within the first few hours of presentation once the fracture is confirmed. These can be done under ultrasound guidance to help visualize the anatomy and target the specific region or using the landmark technique. These should be performed by a trained medical professional but can be done by providers of any specialty who have undergone sufficient training.
Typically, a long-acting anesthetic, such as ropivacaine or bupivacaine, is chosen. Pain relief can be felt up to 12 h or more, with the ability to repeat the block until surgery is performed. Patients should be monitored for 30–60 min after the block for signs of local systemic anesthetic toxicity (LAST). Absolute contraindications include patient refusal or allergy to local anesthetic agents. Patients on anticoagulation can receive regional nerve blocks for hip fractures with complications being rare but will need to be considered on an individual basis with risks such as hematoma or minor bleeding around the puncture site [30].
Surgery for stable intertrochanteric fractures
Inter-trochanteric hip fractures are extracapsular and have minimal risk of nonunion or subsequent osteonecrosis of the femoral head. Given this, they are treated with fixation with either a sliding hip screw (Fig. 1a) or with an intramedullary nail (Fig. 1b). The stability of inter-trochanteric fractures is generally determined by the fracture morphology and involvement of the post-eromedial calcar. Stable fracture patterns generally resist further fracture displacement following an adequate reduction and generally include two-part intertrochanteric fractures [31]. For stable intertrochanteric fractures, the clinical and radiographic outcomes are similar between sliding hip screws and intramedullary nails [32, 33]. Sliding hip screws are significantly less expensive than intramedullary nails and are more cost-effective for stable inter-trochanteric hip fractures [34]. In the era of value-based healthcare, sliding hip screws should be utilized preferentially when indicated in this patient population.
Surgery for subtrochanteric or unstable intertrochanteric fractures
Sub-trochanteric and unstable inter-trochanteric hip fractures are a challenging entity that commonly present to orthopedic surgeons. Unstable intertrochanteric hip fractures include those with post-eromedial comminution, a reverse obliquity fracture pattern, sub-trochanteric extension, and lateral wall comminution [31, 35] (Fig. 2). These unstable fracture patterns are associated with fixation failure and a cephalomedullary nail provides a more favorable biomechanical construct compared to a sliding hip screw in this setting. Patients with a sub-trochanteric or reverse obliquity inter-trochanteric fracture should be treated surgically with intramedullary nails to reduce complication rates [2]. Patients who are low demand with unstable inter-trochanteric fractures can be treated surgically with intra-medullary nails or sliding hip screws as the use of intramedullary nail fixation may be less beneficial in this setting and may not lead to improved functional outcomes [2, 36]. Patients with unstable fracture patterns who are high demand and are able to ambulate without walking aids should be treated surgically with intra-medullary nails [37]. Fracture reduction and implant position are critical variables that play a large role in outcome for all methods of treatment [38]. Long intra-medullary nails are recommended over short nails by some authors, but most comparative studies show no advantage of one technique over the other [39, 40].
Surgery for displaced intracapsular fractures
Displaced intra-capsular hip fractures (femoral neck fractures) (Fig. 3) are at a high risk of avascular necrosis (AVN) and nonunion due to disruption of the blood supply to the femoral neck and head. Surgical options for displaced femoral neck fractures include fixation with either a sliding hip screw or cannulated screws or hip arthroplasty (Fig. 4a). In the elderly patient population, arthroplasty has demonstrated superior results compared to fixation. Arthroplasty results in lower reoperation rates and improved functional outcomes and higher patient satisfaction and quality of life when compared to fixation [41]. In young patients (< 60) who are high functioning and active, clinicians may choose to perform fixation in attempts to save the native joint after discussing the risks and benefits with the patient [42]. Given the risk of AVN, some experts advocate for expedited surgery early after diagnosis. However, there is growing evidence to suggest that the risk of AVN and poor outcomes is directly correlated with the initial fracture displacement and reduction, and surgical timing may not impact outcomes in this population [43].
In patients undergoing arthroplasty for a displaced intra-capsular hip fracture, both hemiarthroplasty and total hip arthroplasty are surgical options [44] (Fig. 4b and c). Hemiarthroplasty involves replacing the femoral head and neck with a prosthesis and total hip arthroplasty involves replacing both the femoral head and acetabular articular surface with prosthetic components. A recent large, international, RCT comparing hemiarthroplasty to total hip arthroplasty demonstrated similar outcomes between the two groups [44]. Total hip arthroplasty should be considered in patients with pre-existing arthritic hip pain or younger, active patients with a longer life expectancy. In considering the use of hemiarthroplasty, modern unipolar and bipolar implants may both be advantageous. When undergoing arthroplasty for a displaced intra-capsular hip fracture, cemented components for the femur should be used to reduce the risk of re-operation and periprosthetic fractures.
Weight-bearing as tolerated
Early post-operative mobilization in hip fracture patients reduces serious post-operative complications including pneumonia, thromboembolism, urinary tract infections, and pressure ulcers. Prolonged immobilization and lack of early weight-bearing have been shown to increase mortality in this patient population [45, 46]. Older patients with hip fractures, particularly those with underlying dementia and delirium, may not be able to comply with weight-bearing restrictions in the postoperative period [47]. Weight-bearing restrictions have been shown to reduce overall mobility without actually reducing the load placed on the affected extremity [48]. Immediate post-operative weight-bearing after hip fracture surgery has not been shown to increase the rate of revision surgery [47, 49, 50]. Given the negative consequences and ineffectiveness of weight-bearing restrictions in hip fracture patients, they should be avoided, and the vast majority of patients should be allowed to mobilize and weight bear as tolerated. Weight-bearing restrictions may be warranted in younger patients who undergo fixation of intra-capsular hip fractures in attempts to salvage the native joint. In these rare situations in which restricted weight-bearing is warranted, a clear plan for progression of mobility and weight bearing should be in place prior to hospital discharge.
Screening for and managing delirium
Delirium, characterized by an acute onset and fluctuation in cognition, consciousness, disorganized thinking, and attention, is a common and serious complication in older patients after hip fracture surgery [51, 52]. The incidence of delirium among hip fracture patients is 20–50% [53]. Post-operative delirium is often associated with falls, impaired functional and cognitive recovery, prolonged hospital stays, discharge to long-term care, and mortality compared to hip fracture patients without delirium, and it may also increase the risk of dementia [54,55,56]. See Tables 1 and 2 for risk factors and causes of delirium. Evaluating risk factors for delirium prior to hip fracture surgery can assist clinicians in identifying patients at risk and facilitating optimal use of preventative measures.
Hip fracture patients should be screened for delirium at admission and throughout the hospital stay as an important step in delirium management is early detection and prevention [58]. Routine laboratory tests, review of patient’s medical history and current illness, and the implementation of a screening test on admission can assist in evaluating a patient for delirium. The Confusion Assessment Method (CAM) is a quick, accurate, and commonly used tool for screening for delirium [59, 60]. It can be incorporated into routine assessments of patients and has been shown to have high sensitivity and specificity (sensitivity of 94% (95% confidence interval (CI), 91–97%) and specificity of 89% (95% CI, 85–94%)) [59, 61]. Diagnosis of delirium may also be completed according to the diagnostic criteria of the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition (DSM-V) criteria, International Classification of Diseases (ICD-10), and the Delirium Rating Scale [51, 62, 63]. As delirium is often associated with pre-existing cognitive impairment, baseline cognitive assessment can be performed, using assessment tools such as the Standardized Mini-Mental State Examination (MMSE) [64], Montreal Cognitive Assessment (MoCA) [65], Mini-Cog [66], Short Portable Mental Status Questionnaire (SPMSQ) [67], and upon hospital admission [68]. Due to the high prevalence of post-operative delirium, hospitalized adult patients should be assessed at least daily for delirium [69].
Management strategies for delirium should be focused on prevention and symptom management. Once delirium has developed, there is limited evidence that pharmacologic therapy is beneficial [70]. A non-pharmacological multicomponent approach is highly effective to reduce the number and duration of delirium episodes [71]. Programs such as the Hospital Elder Life Program (HELP) is a multicomponent approach that uses delirium prevention strategies (such as maintaining orientation, reducing sensory deficits, ensuring adequate nutrition, and hydration) to reduce functional decline, placement in long-term care facilities, and improve overall quality of hospital care [72, 73]. In-patient geriatric consultation as part of a multidisciplinary team has also been shown to decrease episodes of delirium by 40% in patients with hip fracture [74]. A comprehensive geriatric assessment focusing on evaluation of medications, alcohol intake, detailed patient history, early identification and treatment of complications, and mobilization has been shown to decrease the occurrence of delirium [75]. Physical exercise and rehabilitation can improve cognitive function among older adults and decrease the risk of delirium [76,77,78]. Prevention strategies should be prioritized in at-risk patients as such approaches can reduce the development of delirium but have no impact on duration of delirium once it develops.
Once delirium is diagnosed, it is important to identify and treat underlying causes, provide supportive care, and prevent complications. It should be noted that there no specific drugs that are approved the management of delirium. Drug treatments can lead to increased harm to patients, including increased morbidity (including falls and fractures) and mortality.
Pharmacological therapy should only be initiated if non-pharmacological strategies are not adequate to control symptoms and the patient is at risk of harm to themselves or others.
See Table 3 for pharmacologic therapy that may be initiated as indicated [2, 6, 58].
Frailty is a clinical condition associated with increased vulnerability, which results from aging-related decline across psychological, physical, and social functioning [79]. Frail older adults undergoing hip fracture surgery are at increased risk of developing postoperative delirium, longer length of hospital stay, poor functional status, inability to recover pre-fracture mobility, and are more likely to be discharged to a long-term care facility [80]. Examples of frailty assessment methods include the Cardiovascular Health Study (CHS) frailty phenotype method (Fried’s phenotype method) [79] and the Frailty Index (FI) [81]. The Canadian Study of Health and Aging-Clinical Frailty Scale (CSHA-CFS) is a reliable tool to predict mortality or institutional care needs after hip fracture (available here: https://www.dal.ca/sites/gmr/our-tools/clinical-frailty-scale.htmll) [82]. Evaluating frailty is essential in patients undergoing hip fracture surgery to prevent adverse outcomes and improve the overall health status of older adults at discharge.
In summary, delirium is a preventable clinical syndrome that is associated with multiple complications including dementia, functional impairment, prolonged length of stay, long-term care admission, and death [83, 84]. Implementation of a multi-component non-pharmacological prevention program is effective in preventing delirium and improving outcomes for older adults.
Post-operative management
Hip fractures are associated with a high risk of post-operative complications including heart failure, chest infections, pressure injuries, and delirium [85,86,87]. Factors associated with increased risk of post-operative complications include three or more co-morbidities, frailty, underlying respiratory disease, and malignancy [85, 88]. Cohesive, inter-disciplinary, orthogeriatric management has been recommended to optimize care [2, 89, 90].
A systematic approach to post-operative management is required to optimize recovery. Areas of focus should include the following:
-
1.
Nutritional assessment (see Sect. "Nutrition" for more detail)
Nutritional assessment is essential. Malnutrition can be screened for using validated tools including the mini-nutritional assessment-short form (MNA-SF) [91] and malnutrition universal screening tool (MUST) [92]. Accurate assessment of muscle mass and body weight is advised. Protein and high-energy supplements should be provided if required.
-
2.
Pressure injury prevention and care
Pressure injuries are common yet preventable [93]. They are associated with delayed rehabilitation, poorer prognosis, and increased risk of death [94]. Risk factors include poor nutritional status, low body weight, incontinence, diabetes, neuropathy, poor skin condition, and prolonged immobility. Pressure injury risk assessment should be undertaken using a validated tool such as the Braden Scale [95]. Skin care precautions should be taken, such as proper turning, repositioning, and use of pressure relieving equipment.
-
3.
Catheter care
Urinary catheters should be removed by post-operative day 1. If post-operative catheterization is necessary beyond day 1, consider intermittent catheterization. Urinary retention is not uncommon with the addition of iron, calcium, decreased mobility, and constipation—consider post-void residuals if patient is not voiding, has delirium, and/or constipation.
-
4.
Fluid balance assessment
Changes in fluid balance are common post-operatively. The goal of perioperative fluid management is to optimize cardiac output without precipitating cardiac failure. Dehydration can lead to hypotension, acute kidney injury, and delirium whereas fluid overload can lead to cardiac failure. Post-operative strategies to optimize fluid status include avoiding prolonged periods of fasting, assisting with oral fluid intake, monitoring fluid intake and output and the patient’s vital signs [87]. If dehydration cannot be rectified through oral rehydration, consider careful iv fluid administration with regular monitoring.
-
5.
Venous thromboprophylaxis
In patients undergoing hip fracture surgery, the American College of Chest Physicians (CHEST) recommends the use of thromboprophylaxis for a minimum of 10 days post-operatively [21]. The National Institute for Health and Care Excellence (NICE) recommends the use of LMWH or fondaparinux for 28 to 35 days, while Thrombosis Canada similarly supports enoxaparin, dalteparin, tinzaparin, or fondaparinux for 14 to 35 days post-operatively [96, 97]. Other subspecialty societies, including the Orthopedic Trauma Association (OTA) and the European Society of Anesthesiology also support aspirin use post-operatively for up to 35 days following hip fracture surgery [98, 99]. Recent meta-analyses demonstrate equivalence for the use of Direct Oral Anti-Coagulants (DOACs), compared with other pharmacologic thromboprophylaxis [100, 101]. Therefore, pharmacologic thromboprophylaxis using LMWH, aspirin (ASA), or DOACs are recommended for up to 35 days following hip fracture surgery (Table 4) [100,101,102].
-
6.
Fall risk assessment including medication review
A multi-factorial falls risk assessment should be performed including the following domains [103].
-
a.
Focused fall history
-
b.
Detailed medication review including identification of fall risk inducing drugs (FRIDs) [104]
-
c.
Physical examination including gait, balance, mobility, neurological and cognitive function, muscle strength, cardiovascular status, visual acuity, and examination of feet and footwear
-
d.
Functional assessment
-
e.
Environmental assessment
Rehabilitation
Morbidity post-fracture is due to decreased mobility, impaired balance, and fear of falling [105], resulting in an increased risk of falls. These causes prevent approximately 40% of older people from returning to pre-fracture daily activity [106].
Cognitive impairment (dementia or delirium) does not preclude rehabilitation [78, 107]. Delay in initiation of rehabilitation increases risk for hospital mortality (OR 2.2, 95% CI 1.06–4.42, p value 0.034) [108]. Appropriate adaptation of the program to meet individual patient’s needs is advised [109]. See Alberta Health Services regarding post-discharge instructions (available here: http://www.rehabcarealliance.ca/uploads/File/Initiatives_and_Toolkits/QBP/UPDATED_November_2017-_Hip_Fracture_QBP_Rehabilitative_Best_Practices_Framework.pdf) [110]. It is important that rehabilitation happens not only acutely, but post-acutely (recovery hospital) and in the community after discharge. It can take up to 9 months for balance deficits and approximately 1 year for gait and walking speed to recover.
Mechanical load induced by exercise produces stress upon bones and enhances bone formation. Progressive resistance exercise, weight-bearing impact training, and functional balance training constitute most exercise programs. Resistance exercise and impact training promote the greatest bone formation. These recommendations have been developed in a pre-fragility fracture population [111] but are now being applied to post-fracture populations [112]. The general principles are correct technique, gradual loading increments, and avoiding activities that might increase risk for falls [113].
Rehabilitation should include balance training to reduce risk of future falls and fractures. A recent meta-analysis revealed that the balance training group had improved overall physical functioning, gait, lower limb strength, performance tasks, and activity of daily living compared with the control group [114]. More high-quality and large-scale RCTs are needed to identify the optimal regimen of balance training after hip fracture.
Individualized exercise approaches, considering patient preferences and integrating factors associated with patient adherence within the context of physiotherapy (such as counseling sessions, workbooks and goal setting, motivational interviewing, and cognitive behavioral therapy) will improve outcomes [109]. Recently published Clinical Practice Guidelines [115] in post-operative hip fracture patients included a multi-disciplinary approach, progressive resistance exercises, and balance training. Early ambulation, weight-bearing exercises, activities of daily living training, community-level rehabilitation, management of comorbidities/complication prevention, and nutritional support were also suggested [115]. However, in a Cochrane analysis [116] although number needed to treat was 25 patients (95% CI 15 to 100) to avoid one “poor outcome” (defined as mortality and decline in residential status at one year), results were generally borderline. In a hospital in-patient setting, there is moderate-certainty evidence that rehabilitation after hip fracture surgery, when delivered by a multidisciplinary team and supervised by an appropriate medical specialist, results in fewer cases of “poor outcome” (death or deterioration in residential status). However, there is low-certainty evidence that multi-disciplinary rehabilitation may result in fewer deaths in hospital and at 4 to 12 months; however, it may also result in slightly more. There is low-certainty evidence that multi-disciplinary rehabilitation may reduce the numbers of people with poorer mobility at 12 months. The borderline measurable effect of rehabilitation has prompted combination strategies-with nutrition (see section on nutrition) and/ or medications.
Encouraging data comparing in-hospital geriatric care and rehabilitation, to early discharge with a home-based rehabilitation program, has shown that in older people with hip fracture, early discharge followed by geriatric interdisciplinary home rehabilitation resulted in a comparable recovery of independence in activities of daily living (ADL) at 3 and 12 months [117]. A retrospective study also showed similar outcomes between home and in-patient rehabilitation, even though the inpatient group was more medically complex [118]. In addition, outpatient rehabilitation has been shown to be cost saving in one 10-week outreach rehabilitation intervention for nursing home residents who sustained a hip fracture, through reduced post-fracture hospital re-admissions [119]. In-patient clinical care pathways (CCPs) that extended to the outpatient setting showed greater improvements in Health-Related Quality of Life (HRQoL) and physical function compared to CCPs that were only inpatient or outpatient [120]. A feasibility trial also demonstrated that outreach participants achieved better locomotion by 3 months post-fracture compared with participants receiving usual post-fracture care; benefits were sustained to 12 months post-fracture. In adjusted analyses, outreach participants also showed sustained benefits in physical function and HRQoL [121]. See the Fresh Start program for hip fracture recovery guide (available here: https://vch.eduhealth.ca/PDFs/FB/FB.863.F73.pdf) [122].
Inequity to access post hip fracture rehabilitation is an issue in most countries. Consistent decision criteria for access to hip fracture rehabilitation will assist in guiding a standard approach to providing rehabilitation, particularly for patients with cognitive impairment [107, 113].
Recommendations: early mobilization post-operatively including strength, balance, and ADL exercises, home or hospital based are both feasible options; ideally, continuation of the program in the community; ensure equity with clinical practice guidelines; combine rehabilitation with nutritional support.
Osteoporosis management and fracture prevention
Osteoporosis is associated with an increased fracture risk. The estimated mortality rate within the first year following a hip fracture is approximately 37% and 28% in men and women, respectively [123]. Given the high risk of fracture among older adults, it is important to initiate pharmacologic therapy for osteoporosis to prevent fractures both in acute and long-term or outpatient care. Following a hip fracture, patients should undergo a comprehensive assessment by a clinician with osteoporosis expertise and be offered appropriate pharmacologic intervention. Currently, osteoporosis treatment rate following a major osteoporotic fracture is unacceptably low [124, 125]. Pharmacotherapy can reduce the risk of subsequent clinical fractures, as well as improve survival [126]. BMD can be used to monitor treatment efficacy.
Hip and vertebral fractures confer a very high fracture risk and require pharmacologic therapy, preferably with an anabolic agent in order to improve the quality and microstructure of the skeleton [127, 128]. After an initial fracture (spine, hip, pelvis, femur, or clavicle), women have an increased risk of fracture with as high as a 25% risk of second fracture within 2 years, and the risk increases with age [129]. Among women with a prior clinical fracture, 17.9% fractured again within 2-years following the initial fracture and 4.8% sustained a hip fracture [129]. This concept of imminent fracture risk, with an acute rise in fracture risk within the first two years following an index fragility fracture, supports the initiation of targeted therapeutic intervention as soon as possible after a fragility fracture [130]. Appropriate pharmacologic therapy for osteoporosis should be offered for patients, regardless of patient age.
Risk factors for osteoporosis include postmenopausal bone loss as well as age related declines in bone density [131]. Many other diseases and drugs may contribute to further bone loss [132,133,134,135]. A detailed evaluation with exclusion of secondary causes of bone loss prior to confirming a diagnosis of postmenopausal osteoporosis is essential (see Table 5).
We recommend completing the following laboratory tests listed in Table 4 on admission to hospital in order to expedite initiation of appropriate pharmacologic intervention for the underlying osteoporosis.
General internal medicine (GIM) specialists are also closely involved in the care of hospitalized patients post hip fracture. Often, these patients are referred to internal medicine for pre-operative assessment and GIM is concurrently involved in the management of their medical concerns post-operatively. Unfortunately, osteoporosis care is often overlooked during these critical assessments. We strongly recommend internists address skeletal health and ensure exclusion of secondary causes of osteoporosis during the pre-operative assessment of hip fracture patients. It is essential to provide appropriate post-op follow-up with implementation of drug therapy for the underlying osteoporosis prior to discharge.
Renal osteodystrophy chronic kidney disease (CKD) stage 4 (eGFR < 30 ml/min) and 5 (eGFR < 15 ml/min) are associated with changes in serum calcium, phosphorus, parathyroid hormone (PTH), 1,25 dihydroxyvitamin D, and fibroblast growth factor-23 (FGF-23) resulting in abnormal bone structure and function [136]. Hip fracture risk increases dramatically with declines in eGFR. A careful evaluation of the biochemical profile is necessary prior to implementation of drug therapy. In the presence of CKD, osteoporosis may also be complicated by the presence of impaired bone mineralization or osteomalacia. Bone turnover may be elevated or suppressed, and this will impact the choice of drug therapy. It is necessary to normalize vitamin D levels as well as both serum calcium corrected for albumin as well as serum phosphate. PTH should be evaluated and is expected to be elevated with declines in eGFR below 60mls/min [136]. In patients with CKD stage 3a–5 not on dialysis, the optimal PTH level is not known. The Kidney Disease Improving Global Outcomes (KDIGO) guidelines suggest that patients with levels of intact PTH progressively rising or persistently above the upper normal limit for the assay be evaluated for modifiable factors, including hyperphosphatemia, hypocalcemia, high-phosphate intake, and vitamin D deficiency. The current KDIGO guidelines [136] suggest in stage 5 CKD that the PTH level be maintained in the 2–9 × the upper level of normal. Pharmacologic intervention with an anabolic agent may be appropriate off label in the presence of low turnover and an anti-resorptive agent may be suitable if remodeling is elevated. Bisphosphonates are contraindicated if the eGFR < 30-35mls/min.
Fracture risk assessment with and without BMD
High fracture risk is confirmed in the presence of a hip or vertebral fracture, OR > 1 fragility fracture, OR steroid use (prednisone ≥ 7.5 mg or equivalent for ≥ 3 months in the previous year) and concomitant history of a prior fragility fracture. All fragility fractures (low trauma) of the hip have a high fracture risk and require consideration of pharmacologic intervention regardless of the calculated fracture risk. Fracture risk can be calculated by the Fracture Risk Assessment Tool (FRAX) or Canadian Association of Radiologists and Osteoporosis Canada (CAROC) tool [137,138,139,140]. FRAX has been developed and validated in 11 different cohorts including the Canadian population and has been calibrated to fracture and mortality rates in Canada. FRAX can be used with or without BMD to predict the 10-year risk of hip and major osteoporotic fracture (MOF) [141,142,143]. FRAX with BMD (area under the curve (AUC) = 0.72) had a higher discriminative ability for osteoporotic fracture than FRAX without BMD (AUC = 0.69) [144].
Self-reported falls in the previous year are an additional risk factor, independent of FRAX, with a hazard ratio (HR) of 1.64 in women aged 70–90 [145].
Non-pharmacologic interventions and treatment of osteoporosis
-
Nutrition: see section on nutrition page 27
-
Calcium and vitamin D
-
o
Adults aged 50 years and older should ensure an adequate calcium intake of 1200 mg elemental calcium daily [146], ideally from dietary sources as there have been concerns regarding the association of calcium supplements and increased risk of cardiovascular disease and nephrolithiasis [147, 148]. Estimation of dietary calcium intake can be performed using the Osteoporosis Canada calcium calculator, https://osteoporosis.ca/calcium-calculator [149]. If supplements are necessary, calcium carbonate or calcium citrate can be prescribed
-
p
Vitamin D adequacy is essential for optimal intestinal calcium absorption and may also improve balance and muscle strength and decrease the risk of falls [150, 151]. A meta-analysis conducted in postmenopausal women showed a significant reduction in hip and non-vertebral fracture risk with vitamin D supplements at doses of 700–800 IU or more daily [151]. Vitamin D supplementation should be offered, targeting a serum 25 hydroxyvitamin D (25(OH)D) level of 75–125 nmol/L. It is important to ensure that the 25(OH) vitamin D levels are normal before initiating anti resorptive treatment. Vitamin D levels below 25 nmol/L may be associated with osteomalacia and may require replacement for several months prior to initiating additional pharmacologic intervention [152]
-
o
-
Physical activity
-
o
A daily weight bearing exercise program should be emphasized, as regular physical activity has been shown to improve femoral neck (FN) and lumbar spine (LS) BMD in postmenopausal women [153]
-
o
-
Lifestyle changes
-
Fall prevention programs for the elderly
Multiple risk factors for falls have been identified in elderly patients, including cognitive impairment, use of sedative medications, disabilities affecting the lower extremities, poor vision, and abnormalities of balance and gait [156]. Interventions targeting those risk factors may decrease the risk of falls and meta-analysis have proven fall prevention programs to be effective both in community dwelling elderly as well as nursing home residents [157]
Pharmacologic interventions
Osteoporosis treatment options include [128, 158,159,160]:
-
Bisphosphonates, oral (alendronate, risedronate), or intravenous (zoledronate)
-
Denosumab
-
Romosozumab
-
Teriparatide/abaloparatide
-
Selective estrogen receptor modulators (SERMS) (raloxifene or bazedoxifene)
-
Menopausal hormonal therapy (MHT)
Treatment options
Anabolic therapy
An anabolic agent is the preferred option following a hip fracture due to greater impact on fracture risk reduction in comparison to bisphosphonate therapy, see Table 6 and Fig. 5. This was demonstrated in the vertebral fracture treatment comparisons in osteoporotic women (VERO) study comparing the efficacy of teriparatide 20 µg sc daily versus risedronate 35 mg weekly in this head-to-head trial on the occurrence of new radiographic vertebral fractures [161]. Teriparatide decreased new vertebral fractures by 56%, relative risk (RR) 0.44, CI 0.29–0.68, p < 0.01, and clinical fractures (vertebral and non-vertebral) by 52% (hazard ratio (HR) 0.48, CI 0.32–0.74, p < 0.01) in comparison to risedronate [161]. The Active-Controlled Fracture Study in Postmenopausal Women with Osteoporosis at High Risk (ARCH) study compared romosozumab to alendronate in a head to head trial [162]. The romosozumab treated group had a 48% lower risk of new vertebral fractures and a 27% lower risk of clinical fractures when compared to alendronate [162].
-
Romosozumab: is a humanized monoclonal antibody to sclerostin. It increases bone formation and reduces bone resorption and is indicated in the presence of a very high fracture risk. The treatment dose is 210 mg subcutaneously (given as 2 injections of 105 mg each) monthly for up to 12 months. Romosozumab has been shown to reduce the risk of vertebral, hip, and non-vertebral fractures [162, 163]. In the fracture study in postmenopausal women with osteoporosis (FRAME), study romosozumab was compared to placebo and was effective in reducing vertebral and clinical fracture risk [164]. It was well tolerated with no increase in the risk of major adverse cardiovascular events. In the ARCH trial, romosozumab was compared to alendronate [162]. Major adverse cardiovascular adverse events were seen more frequently in the romosozumab group (2.0%) than in the alendronate group (1.1%) [162, 163]. Therefore, romosozumab is contraindicated in the presence of a prior myocardial infarct or stroke and clinicians should carefully consider the risks/benefits ratio in patients with multiple cardiovascular risk factors
-
Teriparatide: is a recombinant human parathyroid hormone (rPTH) 1–34 and is an anabolic agent indicated in the presence of a very high fracture risk. It increases bone formation as well as bone resorption. The treatment dose is 20 mcg subcutaneously daily for up to 24 months. Teriparatide has been shown to reduce the risk of both vertebral and non-vertebral fragility fractures in post-menopausal women at high fracture risk [161]. In the Abaloparatide Comparator Trial In Vertebral Endpoints (ACTIVE) trial, the incidence of hypercalcemia was 6.4% in teriparatide treated patients [165]. It is important to ensure that the serum calcium corrected for albumin and PTH levels are normal prior to initiating therapy. Teriparatide is contraindicated in individuals with a prior history of malignancy or radiation therapy, as well as in patients with eGFR < 15 ml/min
-
Abaloparatide: is a modified PTH-related peptide. It is an anabolic agent indicated in the presence of a very high fracture risk. It increases bone formation as well as bone resorption. The treatment dose is 80 mcg subcutaneously once daily for up to 24 months. It has been shown to reduce both vertebral and non-vertebral fragility fractures [165]. In the ACTIVE study, the incidence of hypercalcemia was 3.4% in abaloparatide treated patients and hypercalcemia and hyperparathyroidism need to be excluded prior to treatment initiation. It is also contraindicated in the presence of prior malignancy or radiation therapy [165]
-
Anti-resorptive therapy
If it is not possible to proceed with an anabolic after a hip fracture, then, denosumab or other anti-resorptive therapies such as IV zoledronate or an oral bisphosphonate such as alendronate or risedronate may be offered. Due to the high risk of fracture recurrence, it is advised that treatment be initiated prior to discharge from hospital if at all possible.
-
Denosumab: is an anti-resorptive agent indicated in the presence of osteoporosis in postmenopausal women or men at a high fracture risk. Denosumab has been shown to reduce the incidence of vertebral, hip, and non-vertebral fracture by 68%, 40%, and 20%, respectively [166]. The treatment dose is 60 mg subcutaneously every 6 months and it can be given safely for up to 10 years. After therapy is discontinued, there is a rapid rebound in increase in osteoclastogenesis and bone resorption that is associated with an increased risk of fractures, and denosumab cessation should be followed by an anti-resorptive molecule such as bisphosphonates [167]. Osteonecrosis of the jaw (ONJ) and atypical femoral fracture (AFF) are rare complications of denosumab treatment, with incidence of 5.2/10,000 person years and 0.8/10,000 person years, respectively [168]. Prior to denosumab initiation, it is important to ensure that serum calcium corrected for albumin and vitamin 25(OH)D level is normal and eGFR should be > 15 ml/min in order to reduce the risk of hypocalcemia[169]
-
Bisphosphonates: Intravenous zoledronate 5 mg is given as an infusion over 30–60 min. A single dose of IV zoledronate can provide long term skeletal protection and may be repeated in 2 yrs [170]. Prior to starting IV zoledronate, it is essential to ensure that serum calcium corrected for albumin and 25 (OH)D are normal and the eGFR must be ≥ 35 mls/min in order to avoid hypocalcemia. Rapid infusion of IV zoledronate may result in declines in renal function and must be avoided [136]. It is also important to ensure that individuals are well hydrated prior to the infusion of IV zoledronate. An acute phase reaction with myalgias, arthralgias, and fever and chills and flu like reaction may occur post-infusion and may last for a several days and is best treated with acetaminophen [171]. The oral bisphosphonate alendronate (70 mg once weekly) and risedronate (35 mg once weekly) are contraindicated in the presence of gastroesophageal reflux disease (GERD), stricture, achalasia, or impaired motility. They are also not suitable in the presence of malabsorption or prior bowel surgery. Patients are also required to sit and remain upright for 30–60 min after the oral bisphosphonate to ensure that the tablet does not reflux into the esophagus. If patients are not able to follow the dosing requirements for an oral bisphosphonate; then, parenteral anti-resorptive therapy should be considered with IV zoledronate or denosumab.
Fractures may occur in patients who have been on drug therapy. In these situations, we would recommend a careful review ensuring that a secondary cause of osteoporosis has not been overlooked. Compliance with therapy should also be evaluated. If the patient was on a bisphosphonate, therapy may be switched to an anabolic agent or denosumab. If the patient was on denosumab then a switch to romosozumab or the addition of teriparatide may be considered [172, 173].
Biomarkers are still being evaluated regarding their applicability in decision making post-fracture and are currently not recommended.
There is no evidence that osteoporosis drug therapy will impact wound, or fracture healing and therapy should be initiated pre-discharge if at all possible. The options available will also be impacted by financial resources and provincial formularies.
Treatment algorithm (reproduced with permission) [127]
Follow-up care
Following hip fracture surgery, patients should be followed up by their primary care provider within two-weeks of discharge from hospital as well as the orthopedic surgeon as advised. This timeframe is important as it embodies the fragmented period in the care transition from acute hospital care to the community where patients may experience poor satisfaction with care, unmet healthcare needs, medication discrepancy, and adverse clinical events [174]. As hip fracture patients may transition between a variety of healthcare settings (i.e., acute care, rehabilitation, home care, and long-term care), patients and families should be provided with standardized education and support on care transition processes.
Patients who experience a hip fracture are also at high risk of secondary fracture. In fact, one in three patients who experience a hip fracture will sustain another fracture within 12 months and over 50% of patients will experience another fracture within 5 years [175]. Although pharmacologic therapy and fall prevention strategies have been demonstrated to be effective in reducing the risk of secondary fractures, fall prevention counseling and osteoporosis treatment rates continue to be low following a hip fracture. Fewer than 20% of patients who sustain a fragility fracture receive pharmacologic treatment in the year following a fracture [176]. Therefore, secondary prevention methods should include treatment and management of osteoporosis and fall prevention. The National Hip Fracture Tool Kit (available here: http://boneandjointcanada.com/hip-fracture/) [177] recommends strategies for fall prevention including:
-
1)
Environment modifications to eliminate fall hazards (removing carpets, handrails, etc.)
-
2)
Physical activity
-
3)
Beware of medications that increase the risk of falling (due to dizziness, drowsiness, gait disturbance, etc.)
-
4)
Equipment such as mobility aids and hip protectors
-
5)
Counseling on fear of falling (which can lead to restricted activity and altered gait that increases the risk of future falls and injuries). Fear of falling can be evaluated using the Falls Efficacy Scale-International [178] (FES-I, short or long version)
-
6)
Healthcare provider and staff education on evidence-based fall prevention (e-learning available through the Canadian Falls Prevention Curriculum)
Educational resources for patient and family on fall prevention are important for secondary fracture prevention. Education and resources are available at Osteoporosis Canada (https://osteoporosis.ca) [179] and Public Health Agency of Canada (http://www.phac-aspc.gc.ca/seniors-aines/publications/public/injuryblessure/falls-chutes/index-eng.php) [180]
Nutrition
Malnutrition, in particular protein and caloric under-nutrition, is considered fracture risks by impairing muscle strength and function, thereby increasing the risk of falling. Compromised bone strength results in increased bone fragility and reduced soft tissue protection around the hip [181].
Malnutrition in older hip fracture patients is also associated with increased complication rates and mortality [182]. In those with malnutrition, mortality is increased more than two-fold [183]. Reported prevalence of malnutrition is common and ranges from 18 to 45% [184] to 85% in hip fracture patients [185]. Pre-fracture nutritional status also affects rehabilitation time and level of recovery [186]. Malnutrition (defined by Subjective Global assessment (SGA)) led to lower rehabilitation efficiency scores and poorer functional outcomes (OR 21.5) when correcting for all other confounders [186]. The global nutrition community is advocating for the Global Leadership Initiative on Malnutrition (GLIM) criteria to be the global standard of care [187]. The GLIM criteria include both phenotypic (weight loss, low body mass index (BMI), and reduced muscle mass) and etiologic (reduced food intake or assimilation and disease burden/inflammation) assessment criteria. However, the SGA is felt to be the most validated tool for diagnosing malnutrition, with a 2020 study suggesting the GLIM tool had low sensitivity compared to the SGA [188].
Serum albumin concentration < 3.5 g/l (< 35gm/L) was previously believed to be suggestive of malnutrition but is now felt to be more a marker of inflammation (along with C-reactive protein or pre-albumin). Hypoalbuminemia is a powerful independent risk factor for mortality following a surgical procedure for geriatric hip fracture [189]. Hypoalbuminemic patients had higher rates of death (9.94% compared with 5.53% (adjusted relative risk, 1.52 (95% CI, 1.37 to 1.70); p < 0.001)) and increased rates of sepsis, risk for intubation, and length of stay [189]. Despite this, correction of albumen in hip fracture patients has not been shown to improve outcomes.
Widespread, prolonged nil-by-mouth fasting (no food or fluids orally), is common [190], exceeding twice the recommended duration for solids and 4 times the recommended duration for fasting with clear fluids. Rates of supplementation remain low, with less than half of patients receiving snacks or nutritional supplements preoperatively, and only 56% of patients having received a solid meal prior to surgery in one region of the United Kingdom (UK). This is likely a common practice in many other regions and countries and has been reported by other groups [190]. Fasting periods regularly exceed 14 h, despite recommendation of 6 h for solid food by the European Society of Anaesthesiology [191], and 6 to 8 h by the American Society of Anesthesiologists, depending on the type of solid ingested [192]. This is often attributed to the common practice of prescribing nil-by-mouth fasting sting at midnight on the day of surgery [193]. The addition of 1 extra meal a day to hip fracture patients was shown to halve mortality across six National Health Service (NHS) trusts in northern England and Scotland [194].
A meta-analysis of pre-operative oral nutrition supplements on post-operative outcomes in geriatric hip fracture patients showed some lowering of post-operative complications (OR 0.48), but the studies available for review were few [195]. In addition, practically speaking, pre-operative supplementation is seldom realistic with the goal for surgery being within 24 h of fracture.
Early post-operative nutritional supplement utilization in malnourished hip fracture patients was associated with significantly shorter length of stay (5.8 (6.6) days vs. 7.6 (5.8) days; p < 0.001) [196] but there was no association between early nutritional supplementation and secondary outcomes, such as infectious complications, hospital mortality, intensive care unit (ICU) admission, and total hospital cost. However, early oral nutritional supplementation (protein intake approximately 70 g/day) reduced the incremental increase of postoperative IL-6 levels, with less time in bed, and better quality of life at 3 months, compared to controls [197].
Combining nutritional supplements and rehabilitation showed a significant reduction in mortality (RR 0.61, 95% CI 0.39, 0.93; I2 = 0%) and complications (RR 0.67, 95% CI 0.44, 1.03; I2 = 79%) and improved grip strength (mean difference = 2.01, 95% CI 0.81, 3.22; I2 = 0%), with the caveat that the quality of the evidence in this meta-analysis was felt to be low [198].
Higher amounts of protein are recommended in older subjects, from a recommended daily allowance of 0.8 g /kg body weight to up to 1.3–1.5, in situations of stress or inflammation, where the needs are higher. PROT-AGE study group [199] recommends 1.0 to 1.2 g protein per kilogram of body weight per day to help older adults maintain and regain lean body mass and function, ≥ 1.2 g/kg body weight/day is recommended for older adults who are exercising, and 1.2–1.5 g/kg body weight/day is recommended for those with chronic disease [199]. Increased protein in those with baseline CKD remains unanswered [200]. But plant-based proteins are safer in those with baseline chronic renal impairment because of their lower bioavailability of phosphate and lower nonvolatile acid loads [201]. Therefore, recommendations are for close monitoring of CKD patients and balancing risks versus benefits in each case.
The effects of nutritional supplements in hip fracture patients have been evaluated in 2 meta-analyses including different numbers of studies [202, 203]. Medical complications, wound, respiratory, and urinary infections were significantly reduced [202] as well as overall unfavorable outcomes including both deaths and medical complications [203].
The ESPEN guidelines on clinical nutrition and hydration in geriatrics [204] recommend routine screening for malnutrition in order to identify an existing risk early; oral nutrition including food modification and oral nutritional supplements, or enteral nutrition where indicated; to avoid dietary restrictions; to consider all to be at risk of low-intake dehydration and encourage adequate fluid intake (as measured by osmolality, 300 mOsm/kg) [204]. They do have recommendations specifically for post hip fracture and orthopedic surgery older adults with hip fracture which state, with good evidence, the benefit of oral nutritional supplements post-operatively to improve dietary intake and reduce risk of complications, regardless of the baseline nutritional state. Nutrition and hydration interventions have also been shown to be efficacious in the prevention of delirium.
Recommendations: objective assessment of nutritional status (e.g., SGA) and serum albumin; avoid unnecessarily prolonged nil-by-mouth fasting and follow evidence-based guidelines on fasting and clear-fluid restrictions; early post-operative nutritional supplementation including adequate calories and protein 1–1.5 g/kg/day; adequate hydration (maintaining serum osmolality < 300 mOsm/kg).
Patient perspective
Patients emphasize the need to provide easily accessible clear direction to physicians so that drugs associated with delirium and falls are avoided. Early surgical intervention should be prioritized with attention given to adequate pain control. Evaluation of skeletal health is seen as critical with identification of underlying metabolic bone disorders which may have contributed to the impaired bone strength and fragility fracture.
Summary
Currently, post hip fracture care in Canada is sub-optimal and a multi-disciplinary approach aimed at optimizing medical and surgical care as well as rehabilitation post hip fracture is expected to improve health care outcomes. It is also anticipated that this will lower morbidity and mortality following a hip fracture. Implementation of strategies designed to achieve the key quality indicators require further education and awareness as well as formal evaluation.
Key messages
Preoperative care:
-
1.
Multi-disciplinary care in the preoperative setting allows for rapid medical optimization and potentially reduces delays to surgery with prompt management of co-morbidities.
-
2.
For surgical candidates, hip fracture patients should undergo surgical intervention within 24 h of diagnosis, and those on pre-injury oral anti-coagulation should undergo surgical treatment within 48 h of diagnosis. If surgery is delayed for more than 12 h from the time of hospital admission, it is recommended that thromboprophylaxis be started pre-operatively.
-
3.
Regional nerve blocks are a safe adjunctive method to improve pain management in patients with hip fractures, leading to decreased opioid use, reduced rate and length of delirium, and decreased length of hospital stay.
Surgical care:
-
4.
Sliding hip screws and cephalomedullary nails are both acceptable treatment options for stable intertrochanteric hip fractures, with sliding hip screws being the more cost-effective implant of choice.
-
5.
Patients with a sub-trochanteric or reverse obliquity intertrochanteric fracture should be treated surgically with intramedullary nails to reduce complication rates. Patients with unstable intertrochanteric fractures who are higher demand (living independently and/or ambulating without assistive devices) should be treated surgically with intramedullary nails.
-
6.
Arthroplasty is preferable over fixation for displaced femoral neck fractures in the elderly population because of the high incidence of avascular, nonunion necrosis, and femoral neck shortening, resulting in the need for revision surgery and/or limitations in function.
-
7.
Whenever possible, hip fracture patients should be allowed to bear weight as tolerated after surgery in order to facilitate early mobilization.
Postoperative care:
-
8.
Individuals who are over 75 years, those with dementia, vision impairment, and dehydration are at high risk for delirium—avoid physical restraints and psychoactive drugs.
-
9.
Inter-disciplinary orthogeriatric care is recommended to optimize patient outcomes and care.
-
10.
Rehabilitation is necessary acutely, post-acutely, and in the community after discharge. It should include progressive resistance, weight-bearing impact, and functional balance training.
-
11.
A low trauma hip fracture denotes a high fracture risk regardless of bone mineral density (BMD) and requires aggressive medical therapy.
-
12.
Home assessment post-discharge by an occupational/physical therapist and exercise should be focused on balance and resistance training.
-
13.
Avoid prolonged nil-by-mouth fasting (no food or fluids orally). Early post-operative nutritional supplements reduce mortality and morbidity (medical complications, wound, respiratory, and urinary infections), especially when combined with rehabilitation.
In patients undergoing hip fracture surgery, pharmacologic thromboprophylaxis is recommended for a minimum of 10 days and up to 35 days post-operatively.
Osteoporosis management and fracture prevention:
-
14.
It is important to initiate pharmacologic therapy for osteoporosis to prevent fractures both in acute and long-term care as well as post-discharge.
-
15.
Hip and vertebral fractures confer a very high fracture risk and require pharmacologic therapy, preferably with an anabolic agent followed by anti-resorptive therapy.
Data Availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- ACTIVE:
-
Abaloparatide Comparator Trial in Vertebral Endpoints
- ARCH:
-
Active-Controlled Fracture Study in Postmenopausal Women with Osteoporosis at High Risk
- ADL:
-
Activities of daily living
- AHS:
-
Alberta Health Services
- ALP:
-
Alkaline phosphatase
- CHEST:
-
American College of Chest Physicians
- ASBMR:
-
American Society For Bone And Mineral Research
- AUC:
-
Area under the curve
- ASA:
-
Aspirin
- AFF:
-
Atypical femoral fracture
- AVN:
-
Avascular necrosis
- BMI:
-
Body mass index
- BMD:
-
Bone mineral density
- CAROC:
-
Canadian Association of Radiologists and Osteoporosis Canada
- CSHA-CFS:
-
Canadian Study of Health and Aging-Clinical Frailty Scale
- CHS:
-
Cardiovascular Health Study
- CKD:
-
Chronic kidney disease
- CCPs:
-
Clinical care pathways
- CBC:
-
Complete blood count
- CI:
-
Confidence interval
- CAM:
-
Confusion Assessment Method
- DVT:
-
Deep venous thrombosis
- DSM-V:
-
Diagnostic And Statistical Manual of Mental Disorders Fifth Edition
- DOACs:
-
Direct oral anti-coagulants
- EKG:
-
Electrocardiogram
- eGFR:
-
Estimated glomerular filtration rate
- FES-I:
-
Falls Efficacy Scale-International
- FRIDs:
-
Fall risk inducing drugs
- FICB:
-
Fascia iliaca compartment block
- FN:
-
Femoral neck
- FGF-23:
-
Fibroblast growth factor-23
- FSH:
-
Follicle stimulating hormone
- FDA:
-
Food And Drug Administration
- FRAX:
-
Fracture Risk Assessment Tool Frax
- FRAME:
-
Fracture study in postmenopausal women with osteoporosis
- FFN:
-
Fragility Fracture Network
- FI:
-
Frailty Index
- GERD:
-
Gastroesophageal reflux disease
- GIM:
-
General internal medicine
- GLIM:
-
Global Leadership Initiative on Malnutrition
- HR:
-
Hazard ratio
- HQO:
-
Health Quality Ontario
- HRQoL:
-
Health-related quality of life
- HELP:
-
Hospital Elder Life Program
- Hrs:
-
Hours
- HIV:
-
Human immunodeficiency viruses
- ICU:
-
Intensive care unit
- IOF:
-
International Osteoporosis Foundation
- IV:
-
Intravenous
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- LAST:
-
Local systemic anesthetic toxicity
- LMWH:
-
Low molecular weight heparin
- LS:
-
Lumbar spine
- LH:
-
Luteinizing hormone
- MOF:
-
Major osteoporotic fracture
- MUST:
-
Malnutrition Universal Screening Tool
- MHT:
-
Menopausal hormonal therapy
- MMSE:
-
Mini-Mental State Examination
- MNA-SF:
-
Mini-Nutritional Assessment-Short Form
- MO:
-
Month
- MoCA:
-
Montreal Cognitive Assessment
- MI:
-
Myocardial infarction
- NHS:
-
National Health Service
- NICE:
-
National Institute for Health and Care Excellence
- OR:
-
Odds ratio
- ONJ:
-
Osteonecrosis of the jaw
- PTH:
-
Parathyroid hormone
- PE:
-
Pulmonary embolism
- RCT:
-
Randomized control trials
- rPTH:
-
Recombinant human parathyroid hormone
- RR:
-
Relative risk
- SERMS:
-
Selective estrogen receptor modulators
- SPMSQ:
-
Short portable mental status questionnaire
- SC:
-
Subcutaneous
- SGA:
-
Subjective Global Assessment
- ICD-10:
-
Tenth International Classification of Diseases
- OTA:
-
The Orthopedic Trauma Association
- TSH:
-
Thyroid-stimulating hormone
- TTG:
-
Tissue transglutaminase
- UK:
-
United Kingdom
- VERO:
-
Vertebral fracture treatment comparisons in osteoporotic women
- 25 OH D 25:
-
Hydroxyvitamin D
References
ASBMR initiates call to action to address the crisis in the treatment of osteoporosis - American Society for Bone and Mineral Research. https://www.asbmr.org/about/news-release-detail/asbmr-initiates-call-to-action-to-address-crisis-i. Accessed 18 Jul 2022
Health Quality Ontario (2017) Hip fracture: care for people with fragility fractures. Health QualOnt 1–49. https://www.hqontario.ca/portals/0/documents/evidence/quality-standards/qs-hip-fracture-clinical-guideen.pdf
International Osteoporosis Foundation | IOF. https://www.osteoporosis.foundation/. Accessed 18 Jul 2022
Home | Capture the fracture. https://www.capturethefracture.org/. Accessed 18 Jul 2022
Fragility Fracture Network (FFN). https://fragilityfracturenetwork.org/. Accessed 18 Jul 2022
Health Services A (2019) Optimizing the post-acute continuum of care following a hip fracture a knowledge synthesis of clinical research interventions for post-acute care of hip fracture initiated within 14 days of surgical repair: A White Paper An Alberta Health Services (AHS) a. https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-bjh-hip-whitepaper.pdf
Larsson G, Holgers KM (2011) Fast-track care for patients with suspected hip fracture. Injury 42:1257–1261. https://doi.org/10.1016/j.injury.2011.01.001
Tosun B, Aslan O, Tunay S (2018) Preoperative position splint versus skin traction in patients with hip fracture: an experimental study. Int J Orthop Trauma Nurs 28:8–15. https://doi.org/10.1016/J.IJOTN.2017.07.002
Forni S, Pieralli F, Sergi A et al (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66:13–17. https://doi.org/10.1016/j.archger.2016.04.014
Flikweert ER, Izaks GJ, Knobben BAS et al (2014) The development of a comprehensive multidisciplinary care pathway for patients with a hip fracture: design and results of a clinical trial. BMC Musculoskelet Disord 15:188. https://doi.org/10.1186/1471-2474-15-188
Folbert EC, Hegeman JH, Vermeer M et al (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28:269–277. https://doi.org/10.1007/S00198-016-3711-7
Grigoryan KV, Javedan H, Rudolph JL (2014) Orthogeriatric care models and outcomes in hip fracture patients: a systematic review and meta-analysis. J Orthop Trauma 28:e49
Leung AHC, Lam TP, Cheung WH et al (2011) An orthogeriatric collaborative intervention program for fragility fractures: a retrospective cohort study. J Trauma Inj Infect Crit Care 71:1390–1394. https://doi.org/10.1097/TA.0b013e31821f7e60
Casey SD, Stevenson DE, Mumma BE et al (2017) Emergency department pain management following implementation of a geriatric hip fracture program. West J Emerg Med 18:585–591. https://doi.org/10.5811/WESTJEM.2017.3.32853
British Geriatric Society (2007) Orthogeriatric models of care. Care Patients Fragility Fract. 7–36. https://www.bgs.org.uk/sites/default/files/content/attachment/2018-05-02/Blue%20Book%20on%20fragility%20fracture%20care.pdf
Chuang D, Power SE, Dunbar PR, Hill AG (2005) Central nervous system interleukin-8 production following neck of femur fracture. ANZ J Surg 75:813–816. https://doi.org/10.1111/j.1445-2197.2005.03530.x
Beloosesky Y, Hendel D, Weiss A et al (2007) Cytokines and C-reactive protein production in hip-fracture-operated elderly patients. J Gerontol Ser A Biol Sci Med Sci 62:420–426. https://doi.org/10.1093/gerona/62.4.420
You D, Skeith L, Korley R et al (2021) Identification of hypercoagulability with thrombelastography in patients with hip fracture receiving thromboprophylaxis. Can J Surg 64:E324–E329. https://doi.org/10.1503/CJS.021019
Pincus D, Ravi B, Wasserstein D et al (2017) Association between wait time and 30-day mortality in adults undergoing hip fracture surgery. JAMA J Am Med Assoc 318:1994–2003. https://doi.org/10.1001/jama.2017.17606
Borges FK, Bhandari M, Guerra-Farfan E et al (2020) Accelerated surgery versus standard care in hip fracture (HIP ATTACK): an international, randomised, controlled trial. The Lancet 395:698–708
Falck-Ytter Y, Francis CW, Johanson NA et al (2012) Prevention of VTE in orthopedic surgery patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 141:e278S-e325S. https://doi.org/10.1378/CHEST.11-2404
Schermann H, Gurel R, Gold A et al (2019) Safety of urgent hip fracture surgery protocol under influence of direct oral anticoagulation medications. Injury 50:398–402. https://doi.org/10.1016/j.injury.2018.10.033
Frenkel Rutenberg T, Velkes S, Vitenberg M et al (2018) Morbidity and mortality after fragility hip fracture surgery in patients receiving vitamin K antagonists and direct oral anticoagulants. Thromb Res 166:106–112. https://doi.org/10.1016/j.thromres.2018.04.022
Xu Y, You D, Krzyzaniak H et al (2020) Effect of oral anticoagulants on hemostatic and thromboembolic complications in hip fracture: a systematic review and meta-analysis. J Thromb Haemost 18:2566–2581. https://doi.org/10.1111/jth.14977
You D, Xu Y, Ponich B et al (2021) Effect of oral anticoagulant use on surgical delay and mortality in hip fracture a systematic review and meta-analysis. Bone Joint J 103 B:222–233. https://doi.org/10.1302/0301-620X.103B2.BJJ-2020-0583.R2
You D, Xu Y, Krzyzaniak H et al (n.d.) Safety of expedited surgical protocols in anticoagulated patients with hip fracture: a systematic review and meta-analysis. In: Can J Surg. https://www.orthomedia.org.uk/Title/da5c6371-eb29-46c7-b1cb-c2bd741f5618. (in press).
Morrison RS, Dickman E, Hwang U, Akhtar S, Ferguson T, Huang J, Jeng CL, Nelson BP, Rosenblatt MA, Silverstein JH, Strayer RJ, Torrillo TM, Todd KH (2016) Regional nerve blocks improve pain and functional outcomes in hip fracture: a randomized controlled trial. J Am Geriatr Soc 64(12):2433–2439. https://doi.org/10.1111/jgs.14386
Ritcey B, Pageau P, Woo MY, Perry JJ (2016) Regional nerve blocks for hip and femoral neck fractures in the emergency department: a systematic review. Can J Emerg Med 18:37–47. https://doi.org/10.1017/cem.2015.75
Mouzopoulos G, Vasiliadis G, Lasanianos N et al (2009) Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol 10:127–133. https://doi.org/10.1007/s10195-009-0062-6
Joubert F, Gillois P, Bouaziz H et al (2019) Bleeding complications following peripheral regional anaesthesia in patients treated with anticoagulants or antiplatelet agents: a systematic review. Anaesth Crit Care Pain Med 38:507–516. https://doi.org/10.1016/j.accpm.2018.12.009
Tawari AA, Kempegowda H, Suk M, Horwitz DS (2015) What makes an intertrochanteric fracture unstable in 2015? Does the lateral wall play a role in the decision matrix? J Orthop Trauma 29:S4–S9. https://doi.org/10.1097/BOT.0000000000000284
Singh NK, Sharma V, Trikha V et al (2019) Is PFNA-II a better implant for stable intertrochanteric fractures in elderly population ? A prospective randomized study. J Clin Orthop Trauma 10:S71–S76. https://doi.org/10.1016/j.jcot.2019.02.004
Parker MJ, Bowers TR, Pryor GA (2012) Sliding hip screw versus the Targon PF nail in the treatment of trochanteric fractures of the hip: a randomised trial of 600 fractures. J Bone Joint Surg Ser B 94 B:391–397. https://doi.org/10.1302/0301-620X.94B3.28406
Swart E, Makhni EC, Macaulay W et al (2014) Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. J Bone Joint Surg Am 96:1612–1620. https://doi.org/10.2106/JBJS.M.00603
Haidukewych GJ (2010) Intertrochanteric fractures: ten tips to improve results. Instr Course Lect 59:503–509
Reindl R, Harvey EJ, Berry GK, Rahme E (2014) Intramedullary versus extramedullary fixation for unstable intertrochanteric fractures: a prospective randomized controlled trial. J Bone Joint Surg Am 97:1905–1912. https://doi.org/10.2106/JBJS.N.01007
Sanders D, Bryant D, Tieszer C et al (2017) A multicenter randomized control trial comparing a novel intramedullary device (InterTAN) versus conventional treatment (sliding hip screw) of geriatric hip fractures. J Orthop Trauma 31:1–8. https://doi.org/10.1097/BOT.0000000000000713
Marmor M, Guenthner G, Rezaei A et al (2021) Reporting on quality of reduction and fixation of intertrochanteric fractures-a systematic review. Injury 52:324–329. https://doi.org/10.1016/J.INJURY.2021.02.014
Sellan M, Bryant D, Tieszer C et al (2019) Short versus long InterTAN fixation for geriatric intertrochanteric hip fractures: a multicentre head-to-head comparison. J Orthop Trauma 33:169–174. https://doi.org/10.1097/BOT.0000000000001409
Shannon SF, Yuan BJ, Cross WW et al (2019) Short versus long cephalomedullary nails for pertrochanteric hip fractures: a randomized prospective study. J Orthop Trauma 33:480–486. https://doi.org/10.1097/BOT.0000000000001553
Gjertsen JE, Vinje T, Engesæter LB et al (2010) Internal screw fixation compared with bipolar hemiarthroplasty for treatment of displaced femoral neck fractures in elderly patients. J Bone Joint Surg 92:619–628. https://doi.org/10.2106/JBJS.H.01750
Chan DS (2019) Femoral neck fractures in young patients: state of the art. J Orthop Trauma 33:S7–S11. https://doi.org/10.1097/BOT.0000000000001366
Xu JL, Liang ZR, Xiong BL et al (2019) Risk factors associated with osteonecrosis of femoral head after internal fixation of femoral neck fracture:a systematic review and meta-analysis. BMC Musculoskelet Disord 20:20. https://doi.org/10.1186/s12891-019-2990-5
Investigators H, Bhandari M, Einhorn TA et al (2019) Total hip arthroplasty or hemiarthroplasty for hip fracture. N Engl J Med 381:2199–2208
Warren J, Sundaram K, Anis H et al (2019) The association between weight-bearing status and early complications in hip fractures. Eur J Orthop Surg Traumatol 29:1419–1427. https://doi.org/10.1007/s00590-019-02453-z
Siu AL, Penrod JD, Boockvar KS et al (2006) Early ambulation after hip fracture: effects on function and mortality. Arch Intern Med 166:766–771. https://doi.org/10.1001/archinte.166.7.766
Kammerlander C, Pfeufer D, Lisitano LA et al (2018) Inability of older adult patients with hip fracture to maintain postoperative weight-bearing restrictions. J Bone Joint Surg Am 100:936–941. https://doi.org/10.2106/JBJS.17.01222
Pfeufer D, Zeller A, Mehaffey S et al (2019) Weight-bearing restrictions reduce postoperative mobility in elderly hip fracture patients. Arch Orthop Trauma Surg 139:1253–1259. https://doi.org/10.1007/s00402-019-03193-9
Koval KJ, Friend KD, Aharonoff GB, Zuckerman JD (1996) Weight bearing after hip fracture: a prospective series of 596 geriatric hip fracture patients. J Orthop Trauma 10:526–530. https://doi.org/10.1097/00005131-199611000-00003
Turgut A, Kalenderer Ö, Karapınar L, Kumbaracı M, Akkan HA, Ağuş H (2016) Which factor is most important for occurrence of cutout complications in patients treated with proximal femoral nail antirotation? Retrospective analysis of 298 patients. Arch Orthop Trauma Surg 136(5):623–30. https://doi.org/10.1007/s00402-016-2410-3
DSM-V (2013) Diagnostic and statistical manual of Dsm-5 TM. Am Psychiatric Assoc 992. https://www.psychiatry.org/psychiatrists/practice/dsm
Wilson JE, Mart MF, Cunningham C et al () Delirium. Nat Rev Dis Primers 6:90. https://doi.org/10.1038/s41572-020-00223-4. https://www.nature.com/articles/s41572-020-00223-4#citeas
Mosk CA, Mus M, Vroemen JPAM et al (2017) Dementia and delirium, the outcomes in elderly hip fracture patients. Clin Interv Aging 12:421–430. https://doi.org/10.2147/CIA.S115945
Marcantonio ER, Flacker JM, Michaels M, Resnick NM (2000) Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc 48:618–624. https://doi.org/10.1111/j.1532-5415.2000.tb04718.x
Kat MG, de Jonghe JFM, Vreeswijk R et al (2011) Mortality associated with delirium after hip-surgery: a 2-year follow-up study. Age Ageing 40:312–318. https://doi.org/10.1093/AGEING/AFR014
Yang Y, Zhao X, Dong T et al (2017) Risk factors for postoperative delirium following hip fracture repair in elderly patients: a systematic review and meta-analysis. Aging Clin Exp Res 29:115–126. https://doi.org/10.1007/s40520-016-0541-6
Cognitive G-EM impairment- causes of delirium. Available here https://geriem.com/cognitive-impairment/causes-of-delirium/
Grover S, Avasthi A (2018) Clinical practice guidelines for management of delirium in elderly. Indian J Psychiatry 60:S329. https://doi.org/10.4103/0019-5545.224473
Waszynski C (2002) The Confusion Assessment Method (CAM). Hartford Inst Geriatr Nurs 13:1–2
Inouye SK, Van Dyck CH, Alessi CA et al (1990) Clarifying confusion: the confusion assessment method. A new method for detection of delirium. Ann Intern Med 113:941–948. https://doi.org/10.7326/0003-4819-113-12-941
Wei LA, Fearing MA, Sternberg EJ, Inouye SK (2008) The Confusion Assessment Method: a systematic review of current usage. J Am Geriatr Soc 56:823–830. https://doi.org/10.1111/J.1532-5415.2008.01674.X
Kyziridis TC (2006) Post-operative delirium after hip fracture treatment - a review of the current literature. Psychosoc Med 3:Doc01
Koskderelioglu A, Onder O, Gucuyener M et al (2017) Screening for postoperative delirium in patients with acute hip fracture: assessment of predictive factors. Geriatr Gerontol Int 17:919–924. https://doi.org/10.1111/ggi.12806
Molloy DW, Standish TIM (1997) A guide to the standardized Mini-Mental State Examination. Int Psychogeriatr 9(Suppl 1):87–94. https://doi.org/10.1017/S1041610297004754
MoCA - cognitive assessment. https://www.mocatest.org/. Accessed 19 Jul 2022
Mini-Cog© – quick screening for early dementia detection. https://mini-cog.com/. Accessed 19 Jul 2022
The short portable mental status questionnaire (SPMSQ). https://geriatrics.stanford.edu/culturemed/overview/assessment/assessment_toolkit/spmsq.html. Accessed 19 Jul 2022
Tuch G, Soo WK, Luo KY et al (2021) Cognitive assessment tools recommended in geriatric oncology guidelines: a rapid review. Curr Oncol 28:3987–4003. https://doi.org/10.3390/curroncol28050339
Wong CL, Holroyd-Leduc J, Simel DL, Straus SE (2010) Does this patient have delirium?: Value of bedside instruments. JAMA J Am Med Assoc 304:779–786. https://doi.org/10.1001/jama.2010.1182
Flaherty JH, Gonzales JP, Dong B (2011) Antipsychotics in the treatment of delirium in older hospitalized adults: a systematic review. J Am Geriatr Soc 59(s2):S269–S276. https://doi.org/10.1111/j.1532-5415.2011.03675.x
Hshieh TT, Yue J, Oh E et al (2015) Effectiveness of multicomponent nonpharmacological delirium interventions: a meta-analysis. JAMA Intern Med 175:512–520. https://doi.org/10.1001/jamainternmed.2014.7779
Inouye SK, Bogardus ST, Baker DI et al (2000) The hospital elder life program: a model of care to prevent cognitive and functional decline in older hospitalized patients. J Am Geriatr Soc 48:1697–1706. https://doi.org/10.1111/j.1532-5415.2000.tb03885.x
Leslie DL, Zhang Y, Bogardus ST et al (2005) Consequences of preventing delirium in hospitalized older adults on nursing home costs. J Am Geriatr Soc 53:405–409. https://doi.org/10.1111/J.1532-5415.2005.53156.X
Marcantonio ER, Kiely DK, Simon SE et al (2005) Outcomes of older people admitted to postacute facilities with delirium. J Am Geriatr Soc 53:963–969. https://doi.org/10.1111/J.1532-5415.2005.53305.X
Shields L, Henderson V, Caslake R (2017) Comprehensive geriatric assessment for prevention of delirium after hip fracture: a systematic review of randomized controlled trials. J Am Geriatr Soc 65:1559–1565. https://doi.org/10.1111/jgs.14846
Haley MN, Casey P, Kane RY et al (2019) Delirium management: let’s get physical? A systematic review and meta-analysis. Australas J Ageing 38:231–241. https://doi.org/10.1111/AJAG.12636
Siddiqi N, Harrison JK, Clegg A et al (2016) Interventions for preventing delirium in hospitalised non-ICU patients. Cochrane Database Syst Rev 11:3
Gual N, García-Salmones M, Brítez L et al (2020) The role of physical exercise and rehabilitation in delirium. Eur Geriatr Med 11:83–93. https://doi.org/10.1007/s41999-020-00290-6
Fried LP, Tangen CM, Walston J et al (2001) McBurnie MA; Cardiovascular Health Study Collaborative Research Group. Frailty in older adults: evidence for a phenotype 56:M146-56
Gandossi CM, Zambon A, Oliveri G et al (2021) Frailty, post-operative delirium and functional status at discharge in patients with hip fracture. Int J Geriatr Psychiatry 36:1524–1530. https://doi.org/10.1002/gps.5561
The frailty index - geriatric medicine research - Dalhousie University. https://www.dal.ca/sites/gmr/our-tools/the-frailty-index.html. Accessed 19 Jul 2022
Clinical frailty scale - geriatric medicine research - Dalhousie University. https://www.dal.ca/sites/gmr/our-tools/clinical-frailty-scale.html. Accessed 18 Jul 2022
Witlox J, Eurelings LSM, De Jonghe JFM et al (2010) Delirium in elderly patients and the risk of postdischarge mortality, institutionalization, and dementia: a meta-analysis. JAMA J Am Med Assoc 304:443–451. https://doi.org/10.1001/jama.2010.1013
Inouye SK, Westendorp RG, Saczynski JS (2014) Delirium in elderly people. Lancet 383:911–922
Roche JJW, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. Br Med J 331:1374–1376. https://doi.org/10.1136/bmj.38643.663843.55
Marcantonio ER, Flacker JM, John Wright R, Resnick NM (2001) Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc 49:516–522. https://doi.org/10.1046/j.1532-5415.2001.49108.x
Falaschi P, Marsh D (eds) (2021) Orthogeriatrics: the management of older patients with fragility fractures [Internet], 2nd edn. Cham (CH): Springer. Available from:https://www.ncbi.nlm.nih.gov/books/NBK565581/. https://doi.org/10.1007/978-3-030-48126-1
Kua J, Ramason R, Rajamoney G, Chong MS (2016) Which frailty measure is a good predictor of early post-operative complications in elderly hip fracture patients? Arch Orthop Trauma Surg 136:639–647. https://doi.org/10.1007/s00402-016-2435-7
Ftouh S, Morga A (2011) Swift C; Guideline Development Group. Management of hip fracture in adults: summary of NICE guidance 342
Australian and New Zealand Hip Fracture Registry (ANZHFR) Steering Group (2014) Australian and New Zealand guideline for hip fracture care improving outcomes in hip fracture management of adults. https://anzhfr.org/wp-content/uploads/sites/1164/2021/12/ANZ-Guideline-for-Hip-Fracture-Care.pdf
Murphy MC, Brooks CN, New SA, Lumbers ML (2000) The use of the Mini-Nutritional Assessment (MNA) tool in elderly orthopaedic patients. Eur J Clin Nutr 54:555–562
Stratton RJ, King CL, Stroud MA et al (2009) Malnutrition Universal Screening Tool (MUST). Oxf Handb Adult Nursing 95:325–330. https://doi.org/10.1093/med/9780199231355.005.0013
Baumgarten M, Margolis DJ, Orwig DL et al (2009) Pressure ulcers in elderly patients with hip fracture across the continuum of care: clinical investigations. J Am Geriatr Soc 57:863–870. https://doi.org/10.1111/j.1532-5415.2009.02245.x
Barrois B, Labalette C, Rousseau P et al (2008) A national prevalence study of pressure ulcers in French hospital inpatients. J Wound Care 17:378–379. https://doi.org/10.12968/jowc.2008.17.9.30934
Bergstrom N, Braden BJ, Lacuzza A, Holman V (1987) The braden scale for predicting pressure sore risk. Nurs Res 36:205–210. https://doi.org/10.1097/00006199-198707000-00002
National Guideline Centre (UK) (2018) Venous thromboembolism in over 16s: reducing the risk of hospital acquired deep vein thrombosis or pulmonary embolism. London: National Institute for Health and Care Excellence (NICE). https://pubmed.ncbi.nlm.nih.gov/29697228/
(2020) Thromboprophylaxis: orthopedic surgery. https://thrombosiscanada.ca/wp-uploads/uploads/2021/01/9.-Thromboprophylaxis-Orthopedic-Surgery_11May2020.pdf
Afshari A, Ageno W, Ahmed A et al (2018) European guidelines on perioperative venous thromboembolism prophylaxis. Eur J Anaesthesiol 35:77–83. https://doi.org/10.1097/EJA.0000000000000729
Ricci WM, Broekhuyse H, Keating JF et al (2019) Thromboprophylaxis an update of current practice. OTA Int 2:e027. https://doi.org/10.1097/OI9.0000000000000027
Nederpelt CJ, Bijman Q, Krijnen P, Schipper IB (2022) Equivalence of DOACS and LMWH for thromboprophylaxis after hip fracture surgery: systematic review and meta-analysis. Injury 53:1169–1176. https://doi.org/10.1016/j.injury.2021.11.052
Wæver D, Lewis D, Saksø H et al (2021) The effectiveness and safety of direct oral anticoagulants following lower limb fracture surgery: a systematic review and meta-analysis. J Orthop Trauma 35:217–224. https://doi.org/10.1097/BOT.0000000000001962
Anderson DR, Morgano GP, Bennett C et al (2019) American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv 3:3898–3944. https://doi.org/10.1182/BLOODADVANCES.2019000975
Drootin M (2011) Summary of the Updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc 59:148–157. https://doi.org/10.1111/J.1532-5415.2010.03234.X
Lee J, Negm A, Peters R et al (2021) Deprescribing fall-risk increasing drugs (FRIDs) for the prevention of falls and fall-related complications: a systematic review and meta-analysis. BMJ Open 11:e035978. https://doi.org/10.1136/BMJOPEN-2019-035978
Johnell O, Kanis JA, Odén A et al (2004) Mortality after osteoporotic fractures. Osteoporos Int 15:38–42. https://doi.org/10.1007/s00198-003-1490-4
Tang VL, Sudore R, Cenzer IS et al (2017) Rates of recovery to pre-fracture function in older persons with hip fracture: an observational study. J Gen Intern Med 32:153–158. https://doi.org/10.1007/s11606-016-3848-2
Mitchell R, Fajardo Pulido D, Ryder T et al (2021) Access to rehabilitation services for older adults living with dementia or in a residential aged care facility following a hip fracture: healthcare professionals’ views. Disabil Rehabil 43:834–845. https://doi.org/10.1080/09638288.2019.1643418
Frenkel Rutenberg T, Vitenberg M, Haviv B, Velkes S (2018) Timing of physiotherapy following fragility hip fracture: delays cost lives. Arch Orthop Trauma Surg 138:1519–1524. https://doi.org/10.1007/s00402-018-3010-1
Pinto D, Alshahrani M, Chapurlat R et al (2022) Bruyere O; Rehabilitation Working Group of IOF Committee of Scientific Advisors. The global approach to rehabilitation following an osteoporotic fragility fracture: a review of the rehabilitation working group of the International Osteoporosis Foundation (IOF) committee of scientific advisors 33:527–540
Rehabilitative Care Alliance (2017) Rehabilitative care best practices for patients with hip fracture. https://doi.org/10.1002/14651858.CD007125.pub2
Daly RM, Dalla Via J, Duckham RL et al (2019) Exercise for the prevention of osteoporosis in postmenopausal women: an evidence-based guide to the optimal prescription. Braz J Phys Ther 23:170–180. https://doi.org/10.1016/j.bjpt.2018.11.011
Singh NA, Quine S, Clemson LM et al (2012) Effects of high-intensity progressive resistance training and targeted multidisciplinary treatment of frailty on mortality and nursing home admissions after hip fracture: a randomized controlled trial. J Am Med Dir Assoc 13:24–30. https://doi.org/10.1016/j.jamda.2011.08.005
Sheehan KJ, Smith TO, Martin FC et al (2019) Conceptual framework for an episode of rehabilitative care after surgical repair of hip fracture. Phys Ther 99:276–285. https://doi.org/10.1093/ptj/pzy145
Wu JQ, Mao LB, Wu J (2019) Efficacy of balance training for hip fracture patients: a meta-analysis of randomized controlled trials. J Orthop Surg Res 14:1. https://doi.org/10.1186/s13018-019-1125-x
Min K, Beom J, Kim BR et al (2021) Clinical practice guideline for postoperative rehabilitation in older patients with hip fractures. Ann Rehabil Med 45:225–259. https://doi.org/10.5535/ARM.21110
Handoll HHG, Cameron ID, Mak JCS et al (2021) Multidisciplinary rehabilitation for older people with hip fractures. Cochrane Database Syst Rev 2021:11. https://doi.org/10.1002/14651858.CD007125.pub3
Karlsson Å, Lindelöf N, Olofsson B et al (2020) Effects of geriatric interdisciplinary home rehabilitation on independence in activities of daily living in older people with hip fracture: a randomized controlled trial. Arch Phys Med Rehabil 101:571–578. https://doi.org/10.1016/j.apmr.2019.12.007
Levi Y, Punchik B, Zikrin E, Shacham D, Katz D, Makulin E, Freud T, Press Y (2020) Intensive inpatient vs. home-based rehabilitation after hip fracture in the elderly population. Front Med (Lausanne) 7:592693. https://doi.org/10.3389/fmed.2020.592693
Beaupre LA, Lier D, Magaziner JS et al (2020) An outreach rehabilitation program for nursing home residents after hip fracture may be cost-saving. J Gerontol Ser A Biol Sci Med Sci 75:E159–E165. https://doi.org/10.1093/gerona/glaa074
Talevski J, Sanders KM, Duque G et al (2019) Effect of clinical care pathways on quality of life and physical function after fragility fracture: a meta-analysis. J Am Med Dir Assoc 20:926.e1-926.e11. https://doi.org/10.1016/j.jamda.2019.02.022
Beaupre LA, Magaziner JS, Jones CA et al (2019) Rehabilitation after hip fracture for nursing home residents: a controlled feasibility trial. J Gerontol A Biol Sci Med Sci 74:1518–1525. https://doi.org/10.1093/GERONA/GLZ031
Vacouver Coastal Health (2018) Fresh Start Toolkit. Fracture recovery for seniors at home: a hip fracture recovery guide for patients & families. https://vch.eduhealth.ca/media/vch/FB/FB.863.F73.pdf
Schnell S, Friedman SM, Mendelson DA et al (2010) The 1-year mortality of patients treated in a hip fracture program for elders. Geriatr Orthop Surg Rehabil 1:6. https://doi.org/10.1177/2151458510378105
Khan AA, AbuAlrob H, Tariq F, Tauqir M, Zalzal P, M'Hiri I, Khan M, Ginty M, Weening B (2021) Osteoporosis treatment rate following hip fracture in a community hospital. Arch Osteoporos 16(1):8. https://doi.org/10.1007/s11657-020-00861-x
Khosla S, Cauley JA, Compston J et al (2017) Addressing the crisis in the treatment of osteoporosis: a path forward. J Bone Miner Res 32:424–430. https://doi.org/10.1002/JBMR.3074
Lyles KW, Colón-Emeric CS, Magaziner JS et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357:1799–1809. https://doi.org/10.1056/NEJMOA074941
Khan AA, Alrob HA, Ali DS et al (2022) Guideline no. 422 g: menopause and osteoporosis. J Obstet Gynaecol Can 44:527–536.e5. https://doi.org/10.1016/J.JOGC.2021.09.013
Shoback D, Rosen CJ, Black DM, Cheung AM, Murad MH, Eastell R (2020) Pharmacological management of osteoporosis in postmenopausal women: an endocrine society guideline update. J Clin Endocrinol Metab 105(3):587–594. https://doi.org/10.1210/clinem/dgaa048
Balasubramanian A, Zhang J, Chen L et al (2019) Risk of subsequent fracture after prior fracture among older women. Osteoporos Int 30:79–92. https://doi.org/10.1007/S00198-018-4732-1
Schnell AD, Curtis JR, Saag KG (2018) Importance of recent fracture as predictor of imminent fracture risk. Curr Osteoporos Rep 16:738–745. https://doi.org/10.1007/S11914-018-0487-Z
Kanis JA, McCloskey EV (1998) Risk factors in osteoporosis. Maturitas 30:229–233. https://doi.org/10.1016/S0378-5122(98)00090-5
Khan AA, Hodsman AB, Papaioannou A et al (2007) Management of osteoporosis in men: an update and case example. CMAJ 176:345–348. https://doi.org/10.1503/CMAJ.050816
Lan G bin, Xie XB, Peng LK et al (2015) Current status of research on osteoporosis after solid organ transplantation: pathogenesis and management. Biomed Res Int 2015:413169. https://doi.org/10.1155/2015/413169
Ebeling PR (2008) Clinical practice. Osteoporosis in men. N Engl J Med 358:1474–1482. https://doi.org/10.1056/NEJMCP0707217
Sozen T, Ozisik L, Calik Basaran N (2017) An overview and management of osteoporosis. Eur J Rheumatol 4:46–56. https://doi.org/10.5152/EURJRHEUM.2016.048
KDIGO (2017) Clinical Practice Guideline Update for the Diagnosis, evaluation, prevention, and treatment of chronic kidney disease-mineral and bone disorder (CKD-MBD). Kidney Int Suppl 2011(7):1–59. https://doi.org/10.1016/J.KISU.2017.04.001
Kanis JA, McCloskey E, Johansson H et al (2012) FRAX(®) with and without bone mineral density. Calcif Tissue Int 90:1–13. https://doi.org/10.1007/S00223-011-9544-7
Kanis JA, Johansson H, Oden A, Cooper C, McCloskey EV (2014) Epidemiology and quality of life working group of iof. worldwide uptake of FRAX. Arch Osteoporos 9:166. https://doi.org/10.1007/s11657-013-0166-8
Leslie WD, Majumdar SR, Lix LM et al (2012) High fracture probability with FRAX usually indicates densitometric osteoporosis: implications for clinical practice. Osteoporos Int 23:391–397. https://doi.org/10.1007/S00198-011-1592-3
Leslie WD, Lix LM (2010) Simplified 10-year absolute fracture risk assessment: a comparison of men and women. J Clin Densitom 13:141–146. https://doi.org/10.1016/J.JOCD.2010.02.002
Kanis JA, Harvey NC, Johansson H et al (2020) A decade of FRAX: how has it changed the management of osteoporosis? Aging Clin Exp Res 32:187–196. https://doi.org/10.1007/S40520-019-01432-Y
Hoff M, Meyer HE, Skurtveit S et al (2017) Validation of FRAX and the impact of self-reported falls among elderly in a general population: the HUNT study, Norway. Osteoporos Int 28:2935–2944. https://doi.org/10.1007/S00198-017-4134-9
Sundh V, Hange D, Ahlqwist M et al (2017) FRAX and mandibular sparse trabeculation as fracture predictors: a longitudinal study from 1980 to 2002. Eur J Oral Sci 125:135–140. https://doi.org/10.1111/EOS.12341
Beaudoin C, Moore L, Gagné M et al (2019) Performance of predictive tools to identify individuals at risk of non-traumatic fracture: a systematic review, meta-analysis, and meta-regression. Osteoporos Int 30:721–740. https://doi.org/10.1007/s00198-019-04919-6
Harvey NC, Odén A, Orwoll E et al (2018) Falls predict fractures independently of FRAX probability: a meta-analysis of the osteoporotic fractures in men (MrOS) study. J Bone Miner Res 33:510–516. https://doi.org/10.1002/JBMR.3331
Ross AC, Manson JAE, Abrams SA et al (2011) The 2011 report on dietary reference intakes for calcium and vitamin D from the Institute of Medicine: what clinicians need to know. J Clin Endocrinol Metab 96:53–58. https://doi.org/10.1210/JC.2010-2704
Bolland MJ, Grey A, Avenell A, Gamble GD, Reid IR (2011) Calcium supplements with or without vitamin D and risk of cardiovascular events: reanalysis of the Women's Health Initiative limited access dataset and meta-analysis. BMJ 342:d2040. https://doi.org/10.1136/bmj.d2040
Jackson RD, LaCroix AZ, Gass M et al (2006) Calcium plus vitamin D supplementation and the risk of fractures. N Engl J Med 354:669–683. https://doi.org/10.1056/NEJMOA055218
Calcium Calculator | Osteoporosis Canada. https://osteoporosis.ca/calcium-calculator/. Accessed 28 Nov 2022
Pfeifer M, Begerow B, Minne HW et al (2009) Effects of a long-term vitamin D and calcium supplementation on falls and parameters of muscle function in community-dwelling older individuals. Osteoporos Int 20:315–322. https://doi.org/10.1007/S00198-008-0662-7
Bischoff-Ferrari HA, Willett WC, Wong JB et al (2005) Fracture prevention with vitamin D supplementation: a meta-analysis of randomized controlled trials. JAMA 293:2257–2264. https://doi.org/10.1001/JAMA.293.18.2257
Minisola S, Colangelo L, Pepe J, Diacinti D, Cipriani C, Rao SD (2020) Osteomalacia and vitamin D status: a clinical update 2020. JBMR Plus 5(1):e10447. https://doi.org/10.1002/jbm4.10447
Kelley GA, Kelley KS, Kohrt WM (2012) Effects of ground and joint reaction force exercise on lumbar spine and femoral neck bone mineral density in postmenopausal women: a meta-analysis of randomized controlled trials. BMC Musculoskelet Disord 13:177. https://doi.org/10.1186/1471-2474-13-177
Kanis JA, Johnell O, Oden A et al (2005) Smoking and fracture risk: a meta-analysis. Osteoporos Int 16:155–162. https://doi.org/10.1007/S00198-004-1640-3
Kanis JA, Johansson H, Johnell O et al (2005) Alcohol intake as a risk factor for fracture. Osteoporos Int 16:737–742. https://doi.org/10.1007/S00198-004-1734-Y
Tinetti ME, Speechley M, Ginter SF (1988) Risk factors for falls among elderly persons living in the community. N Engl J Med 319:1701–1707. https://doi.org/10.1056/NEJM198812293192604
Choi M, Hector M (2012) Effectiveness of intervention programs in preventing falls: a systematic review of recent 10 years and meta-analysis. J Am Med Dir Assoc 13:188.e13-188.e21. https://doi.org/10.1016/J.JAMDA.2011.04.022
Papaioannou A, Morin S, Cheung AM et al (2010) 2010 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada: summary. CMAJ 182:1864–1873. https://doi.org/10.1503/CMAJ.100771
Camacho PM, Petak SM, Binkley N et al (2020) American Association of Clinical Endocrinologists/American College of Endocrinology clinical practice guidelines for the diagnosis and treatment of postmenopausal osteoporosis-2020 update. Endocr Pract 26:1–46. https://doi.org/10.4158/GL-2020-0524SUPPL
Khan AA, Alrob HA, Ali DS, et al (2022) Guideline no. 422g: menopause and osteoporosis. J Obstet Gynaecol Can 44(5):527–536.e5. https://doi.org/10.1016/j.jogc.2021.09.013
Kendler DL, Marin F, Zerbini CAF et al (2018) Effects of teriparatide and risedronate on new fractures in post-menopausal women with severe osteoporosis (VERO): a multicentre, double-blind, double-dummy, randomised controlled trial. Lancet 391:230–240. https://doi.org/10.1016/S0140-6736(17)32137-2
Saag KG, Petersen J, Brandi ML et al (2017) Romosozumab or alendronate for fracture prevention in women with osteoporosis. N Engl J Med 377:1417–1427. https://doi.org/10.1056/NEJMOA1708322
Cosman F, Crittenden DB, Adachi JD et al (2016) Romosozumab treatment in postmenopausal women with osteoporosis. N Engl J Med 375:1532–1543. https://doi.org/10.1056/NEJMOA1607948
Cosman F, Crittenden DB, Ferrari S et al (2018) FRAME study: the foundation effect of building bone with 1 year of romosozumab leads to continued lower fracture risk after transition to denosumab. J Bone Miner Res 33:1219–1226. https://doi.org/10.1002/JBMR.3427
Miller PD, Hattersley G, Riis BJ et al (2016) Effect of abaloparatide vs placebo on new vertebral fractures in postmenopausal women with osteoporosis: a randomized clinical trial. JAMA 316:722–733. https://doi.org/10.1001/JAMA.2016.11136
Cummings SR, Martin JS, McClung MR et al (2009) Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med 361:756–765. https://doi.org/10.1056/NEJMOA0809493
Everts-Graber J, Reichenbach S, Ziswiler HR et al (2020) A single infusion of zoledronate in postmenopausal women following denosumab discontinuation results in partial conservation of bone mass gains. J Bone Miner Res 35:1207–1215. https://doi.org/10.1002/JBMR.3962
Bone HG, Wagman RB, Brandi ML et al (2017) 10 years of denosumab treatment in postmenopausal women with osteoporosis: results from the phase 3 randomised FREEDOM trial and open-label extension. Lancet Diabetes Endocrinol 5:513–523. https://doi.org/10.1016/S2213-8587(17)30138-9
Tsvetov G, Amitai O, Shochat T et al (2020) Denosumab-induced hypocalcemia in patients with osteoporosis: can you know who will get low? Osteoporos Int 31:655–665. https://doi.org/10.1007/S00198-019-05261-7
Reid IR, Brown JP, Burckhardt P et al (2002) Intravenous zoledronic acid in postmenopausal women with low bone mineral density. N Engl J Med 346:653–661. https://doi.org/10.1056/NEJMOA011807
Adami S, Bhalla AK, Dorizzi R et al (1987) The acute-phase response after bisphosphonate administration. Calcif Tissue Int 41:326–331. https://doi.org/10.1007/BF02556671
Cosman F, Nieves JW, Dempster DW (2017) Treatment sequence matters: anabolic and antiresorptive therapy for osteoporosis. J Bone Miner Res 32:198–202. https://doi.org/10.1002/JBMR.3051
Leder BZ, Tsai JN, Uihlein AV et al (2015) Denosumab and teriparatide transitions in postmenopausal osteoporosis (the DATA-Switch study): extension of a randomised controlled trial. Lancet 386:1147–1155. https://doi.org/10.1016/S0140-6736(15)61120-5
Health Services A (2019) Optimizing the post-acute continuum of care following a hip fracture a knowledge synthesis of clinical research interventions for post-acute care of hip fracture initiated within 14 days of surgical repair: A White Paper An Alberta Health Services (AHS) and Bone and Joint Health Strategic Clinical Network (BJH SCN) and Seniors Strategic Clinical Network (Seniors SCN) Workshop 2 Alberta Health Services BJH SCN Post-Acute Care of Hip Fracture White Paper. https://www.albertahealthservices.ca/assets/about/scn/ahs-scn-bjh-hip-white-paper.pdf
McGlasson R, Zellermeyer V, MacDonald V, Lo Nick, Spafford D, McMullan JL, Beaupre L, Gould JS, Saryeddine T, Scott V (2011) National Hip Fracture Toolkit. The Bone and Joint Decade. https://boneandjointcanada.com/wpcontent/uploads/2014/05/National-hip-fracture-toolkit-June-2011.pdf. Accessed 25 Mar 2022
Kanis JA, Svedbom A, Harvey N, McCloskey EV (2014) The osteoporosis treatment gap. J Bone Miner Res 29:1926–1928. https://doi.org/10.1002/JBMR.2301
McGlasson R, Zellermeyer V, MacDonald V et al (2011) National hip fracture toolkit. Bone Joint Decade
Dewan N, MacDermid JC (2014) Fall efficacy scale - international (FES-I). J Physiother 60:60. https://doi.org/10.1016/j.jphys.2013.12.014
Osteoporosis Canada. https://osteoporosis.ca/. Accessed 28 Nov 2022
Seniors’ Falls in Canada: Second Report - Canada.ca. https://www.canada.ca/en/public-health/services/health-promotion/aging-seniors/publications/publications-general-public/seniors-falls-canada-second-report.html. Accessed 28 Nov 2022
Rizzoli R (2014) Nutritional aspects of bone health. Best Pract Res Clin Endocrinol Metab 28:795–808. https://doi.org/10.1016/J.BEEM.2014.08.003
Lim SL, Ong KCB, Chan YH et al (2012) Malnutrition and its impact on cost of hospitalization, length of stay, readmission and 3-year mortality. Clin Nutr 31:345–350. https://doi.org/10.1016/J.CLNU.2011.11.001
Bell JJ, Pulle RC, Crouch AM et al (2016) Impact of malnutrition on 12-month mortality following acute hip fracture. ANZ J Surg 86:157–161. https://doi.org/10.1111/ANS.13429
Malafarina V, Reginster JY, Cabrerizo S, Bruyère O, Kanis JA, Martinez JA, Zulet MA (2018) Nutritional status and nutritional treatment are related to outcomes and mortality in older adults with hip fracture. Nutrients 10(5):555. https://doi.org/10.3390/nu10050555
Koren-Hakim T, Weiss A, Hershkovitz A et al (2016) Comparing the adequacy of the MNA-SF, NRS-2002 and MUST nutritional tools in assessing malnutrition in hip fracture operated elderly patients. Clin Nutr 35:1053–1058. https://doi.org/10.1016/J.CLNU.2015.07.014
Wong AM, Xu BY, Low LL et al (2021) Impact of malnutrition in surgically repaired hip fracture patients admitted for rehabilitation in a community hospital: a cohort prospective study. Clin Nutr ESPEN 44:188–193. https://doi.org/10.1016/J.CLNESP.2021.06.024
Cederholm T, Jensen GL, Correia MITD et al (2019) GLIM criteria for the diagnosis of malnutrition - a consensus report from the global clinical nutrition community. Clin Nutr 38:1–9. https://doi.org/10.1016/J.CLNU.2018.08.002
Allard JP, Keller H, Gramlich L et al (2020) GLIM criteria has fair sensitivity and specificity for diagnosing malnutrition when using SGA as comparator. Clin Nutr 39:2771–2777. https://doi.org/10.1016/J.CLNU.2019.12.004
Bohl DD, Shen MR, Hannon CP et al (2017) Serum albumin predicts survival and postoperative course following surgery for geriatric hip fracture. J Bone Joint Surg Am 99:2110–2118. https://doi.org/10.2106/JBJS.16.01620
Dixon J, Channell W, Arkley J, Eardley W (2019) Nutrition in Hip Fracture Units: Contemporary Practices in Preoperative Supplementation. Geriatr Orthop Surg Rehabil. https://doi.org/10.1177/2151459319870682
Smith I, Kranke P, Murat I et al (2011) Perioperative fasting in adults and children: guidelines from the European Society of Anaesthesiology. Eur J Anaesthesiol 28:556–569. https://doi.org/10.1097/EJA.0B013E3283495BA1
American Society of Anesthesiologists Committee (2011) Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American society of anesthesiologists committee on standards and practice parameters. Anesthesiology 114(3):495–511
Green CR, Pandit SK, Anthony Schork M (1996) Preoperative fasting time: is the traditional policy changing? Results of a national survey. Anesth Analg 83:123–128. https://doi.org/10.1097/00000539-199607000-00022
HipQIP: scaling up project | RCP London. https://www.rcplondon.ac.uk/projects/outputs/hipqip-scaling-project. Accessed 28 Nov 2022
Lai WY, Chiu YC, Lu KC, Huang IT, Tsai PS, Huang CJ (2021) Beneficial effects of preoperative oral nutrition supplements on postoperative outcomes in geriatric hip fracture patients: a PRISMA-compliant systematic review and meta-analysis of randomized controlled studies. Medicine (Baltimore)100(47):e27755. https://doi.org/10.1097/MD.0000000000027755
Williams DGA, Ohnuma T, Haines KL et al (2021) Association between early postoperative nutritional supplement utilisation and length of stay in malnourished hip fracture patients. Br J Anaesth 126:730–737. https://doi.org/10.1016/J.BJA.2020.12.026
Shi H, Lu JH, Wang SN et al (2020) Effect of early enteral nutrition in elderly patients with hip fracture during the perioperative period. J Back Musculoskelet Rehabil 33:109–117. https://doi.org/10.3233/BMR-181191
Takahashi K, Momosaki R, Yasufuku Y et al (2020) Nutritional therapy in older patients with hip fractures undergoing rehabilitation: a systematic review and meta-analysis. J Am Med Dir Assoc 21:1364-1364.e6. https://doi.org/10.1016/J.JAMDA.2020.07.005
Bauer J, Biolo G, Cederholm T et al (2013) Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc 14:542–559. https://doi.org/10.1016/J.JAMDA.2013.05.021
Yan B, Su X, Xu B, Qiao X, Wang L (2018) Effect of diet protein restriction on progression of chronic kidney disease: A systematic review and meta-analysis. PLoS One 13(11):e0206134. https://doi.org/10.1371/journal.pone.0206134
Scialla JJ, Appel LJ, Wolf M, Yang W, Zhang X, Sozio SM, Miller ER 3rd, Bazzano LA, Cuevas M, Glenn MJ, Lustigova E, Kallem RR, Porter AC, Townsend RR, Weir MR, Anderson CA (2012) Chronic renal insufficiency cohort-cric study group: plant protein intake is associated with fibroblast growth factor 23 and serum bicarbonate levels in patients with chronic kidney disease: the Chronic Renal Insufficiency Cohort study. J Ren Nutr 22(4):379–388.e1. https://doi.org/10.1053/j.jrn.2012.01.026
Liu M, Yang J, Yu X et al (2015) The role of perioperative oral nutritional supplementation in elderly patients after hip surgery. Clin Interv Aging 10:849–858. https://doi.org/10.2147/CIA.S74951
Avenell A, Smith TO, Curtain JP, Mak JC, Myint PK (2016) Nutritional supplementation for hip fracture aftercare in older people. Cochrane Database Syst Rev 11(11):CD001880. https://doi.org/10.1002/14651858.CD001880.pub6
Volkert D, Beck AM, Cederholm T et al (2019) ESPEN guideline on clinical nutrition and hydration in geriatrics. Clin Nutr 38:10–47. https://doi.org/10.1016/J.CLNU.2018.05.024
Funding
We acknowledge unrestricted financial support from Amgen. They had no input into the planning or design of the project, the conduct of the reviews, evaluation of the data, writing or review of the manuscript, its content, conclusions, or recommendations contained herein.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AK has received research grants from Alexion, Amgen, Ascendis, Chugai, Radius, Takeda, and Ultragenyx and is on the advisory board for Amgen, Amolyt, and Takeda. EB has received unrestricted research grant Amgen Canada and is on the advisory Board for Amgen Canada. AGJ is a consultant for Amgen and Paladin Lab and speaker for Amgen. ES has received a research grant from Amgen and is a consultant for Amgen. JT has received research funding and speaker honorarium from Amgen. AP has received grants, honorarium from Amgen and is on the advisory board for Amgen and Paladin Labs. The other authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Endorsement: This position paper has been endorsed by the Fragility Fracture Network and the International Osteoporosis Foundation as well as the Canadian Geriatric Society
This position paper has been endorsed by the Fragility Fracture Network and the International Osteoporosis Foundation as well as the Canadian Geriatric Association.
Aliya A Khan and Hajar AbuAlrob are first authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Khan, A.A., AbuAlrob, H., Al-alwani, H. et al. Post hip fracture orthogeriatric care—a Canadian position paper addressing challenges in care and strategies to meet quality indicators. Osteoporos Int 34, 1011–1035 (2023). https://doi.org/10.1007/s00198-022-06640-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06640-3