Abstract
Summary
Hip fractures are a serious public health issue with major consequences, especially for frail community dwellers. This study found a poor prognosis at 6 months post-trauma with regard to life expectancy and rehabilitation to pre-fracture independency levels. It should be realized that recovery to pre-trauma functioning is not a certainty for frail community-dwelling patients.
Introduction
Proximal femoral fractures are a serious public health issue in the older patient. Although a significant rise in frail community-dwelling elderly is expected because of progressive aging, a clear overview of the outcomes in these patients sustaining a proximal femoral fracture is lacking. This study assessed the prognosis of frail community-dwelling patients who sustained a proximal femoral fracture.
Methods
A multicenter retrospective cohort study was performed on frail community-dwelling patients with a proximal femoral fracture who aged over 70 years. Patients were considered frail if they were classified as American Society of Anesthesiologists score ≥ 4 and/or a BMI < 18.5 kg/m2 and/or Functional Ambulation Category ≤ 2 pre-trauma. The primary outcome was 6-month mortality. Secondary outcomes were adverse events, health care consumption, rate of institutionalization, and functional recovery.
Results
A total of 140 out of 2045 patients matched the inclusion criteria with a median age of 85 (P25–P75 80–89) years. The 6-month mortality was 58 out of 140 patients (41%). A total of 102 (73%) patients experienced adverse events. At 6 months post-trauma, 29 out of 120 (24%) were readmitted to the hospital. Out of the 82 surviving patients after 6 months, 41 (50%) were unable the return to their home, and only 32 (39%) were able to achieve outdoor ambulation.
Conclusion
Frail community-dwelling older patients with a proximal femoral fracture have a high risk of death, adverse events, and institutionalization and often do not reobtain their pre-trauma level of independence. Foremost, the results can be used for realistic expectation management.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Proximal femoral fractures are a serious public health issue in the older patient. The injury has major consequences with regard to mortality, morbidity, and health-related quality of life (HRQoL) [1,2,3,4,5]. Furthermore, recovery to pre-fracture functioning is lengthy and often unsuccessful [6, 7]. Mortality rates for the frailest patients with a proximal femoral fracture are as high as 36–55% after 6 months, and recovery to pre-trauma mobility is as low as 10–20% [7,8,9,10].
The degree of frailty greatly determines the prognosis [11, 12].
In the Netherlands, 92% of the adults aged over 75 years and 65% of adults aged over 90 years are community-dwelling, but while they live independently, it is estimated that up to one-third can be considered frail [13]. Due to progressive aging, the number of proximal femoral fractures in patients aged over 65 years is expected to rise with another 69% between 2012 and 2040 [14]. With 75% of the patients sustaining a proximal femoral fracture being community-dwelling, a stark rise in frail community-dwelling patients is to be expected [15].
Remarkably, the prognosis of frail community-dwelling patients is relatively unknown. Current studies addressing the prognosis of patients with a proximal femoral fracture do not separately address frail community-dwelling older patients but focus on institutionalized patients or highly heterogenic study populations which include high proportions of non-frail patients [16]. In addition, these studies mostly focus on patients aged over 65 years old without addressing the effect of frailty and, in case they do account for frailty, they do not address the specific prognosis of community-dwelling patients [12, 17,18,19,20,21,22,23]. It has been suggested previously that future studies on older patients with a proximal femoral fracture should focus on certain subpopulations to further elucidate the relation between certain demographic factors and functional and survival outcomes [24].
A clear overview of the specific prognosis on frail community-dwelling older patients is needed to properly inform patients and their relatives of the often challenging recovery period ahead. Detailed knowledge on the prognosis will aid in realistic expectation management, better informed decision making, health care planning, and advance care planning in the community and create more awareness about the significant impact of the injury for this patient population.
This multicenter retrospective cohort study assessed the prognosis of a specific group of frail community-dwelling older patients who sustained a proximal femoral fracture with regard to mortality, adverse events, health care consumption, and functional outcome.
Method and materials
A multicenter retrospective analysis of frail community-dwelling older patients who sustained a proximal femoral fracture that were presented to three large teaching hospitals (Northwest Clinics, St. Antonius Ziekenhuis, or Ziekenhuisgroep Twente) between January 1, 2018 and September 30, 2019 was performed. Patients were identified based on diagnosis-related group (DRG; in Dutch DBC 218; hip fracture).
Patients were eligible for inclusion if they were aged ≥ 70 years old, sustained a proximal femur fracture after a low-impact injury, and were considered frail. The term frail implied that at least 1 of the following characteristics was present: classified as American Society of Anesthesiologists (ASA) score ≥ 4 and/or a body mass index (BMI) < 18.5 kg/m2 and/or Functional Ambulation Category (FAC) of ≤ 2 pre-trauma (meaning that they require (intermittent) assistance of a person for safe ambulation) [25]. We choose to define patients that could be considered frail based on the mentioned criteria because of the retrospective nature of the study and other forms of established frailty assessments could not be performed. Comorbidities [26, 27], decreased BMI [28], and decreased mobility [29] have been described in previous literature as predictors for adverse outcomes after surgery.
Patients with fractures due to metastasis, periprosthetic fractures, and concomitant proximal femoral, pelvic, or other low extremity fractures in the previous 3 months prior to the injury or with a delayed presentation to the ED of ≥ 7 days post-trauma were excluded.
Outcome measures and data collection
All outcomes were ascertained via retrospective hospital chart reviewing in combination with data from the Dutch Hip Fracture Audit (DHFA) from the participating centers. The DHFA is a nationwide permanent hip fracture registry with a 3-month follow-up. Data were collected according to a pre-defined case report form.
The primary outcome measure was the 6-month mortality rate post-trauma. Secondary outcome measures were adverse events, health care, readmission, residency, functional outcome, and activities of daily living (ADL) dependency during the 6-month follow-up period. Health care consumption was measured by length of stay, number of (para)medic consultations, the requirement of intensive care admission, readmissions, and outpatient clinic follow-up. Furthermore, the use of antipsychotic drugs, the use of physical restraints to prevent adverse events, and the number of blood transfusions were recorded. Functional outcome was measured with the pre-fracture mobility score (PMS) and was measured at admission, at hospital discharge, and at 3 months and 6 months post-trauma. ADL dependency was measured via the Katz Index of Independence in Activities of Daily Living (Katz ADL) score at admission and after 3 months.
The following patient, fracture, and treatment characteristics were collected: age, sex, BMI, ASA grade, Charlson comorbidity index (CCI) [30], FAC score pre-trauma, PMS, Katz ADL score, pre-trauma level of home care assistance with ADL, nutritional assessment (Short Nutritional Assessment Questionnaire (SNAQ) or Malnutrition Universal Screening Tool (MUST) score), fracture types, additional injuries, time to surgery, type of treatment, and type of anesthesia. These characteristics were also used to identify risk factors for mortality, inability to return to their own home, and unsuccessful rehabilitation (not regaining pre-fracture PMS) after 6 months. Death before regaining previous mobility or returning to home was regarded as not regaining pre-trauma PMS or institutionalization at the 6-month follow-up. No data was gathered for excluded patients in this study as no consent or waiver was provided to allow analysis of these patients.
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS), version 24.0 (SPSS, Chicago, IL, USA). The results were reported according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [31]. No data imputation was used to replace missing values. Normality of continuous data was tested with the Shapiro–Wilk test. Continuous data, which were all non-parametric, were shown as median and quartiles. Categorical data were reported as numbers and frequencies. Univariate comparison was done using the Mann–Whitney U test or chi-square test or Fisher’s exact test, as applicable. Risk factors for mortality, institutionalization, and unsuccessful rehabilitation after 6 months were performed using logistic regression analysis and reported as OR with corresponding 95% confidence interval. As it is important to predict these factors early in the process, only patient characteristics and fracture type were considered in this analysis. Since the level of home care and the Katz ADL score are closely related, as is facture type and surgical treatment, only the level of home care and fracture type were included in the analysis. Parameters that showed a p value < 0.10 in the univariate logistic analysis were included in a multiple logistic regression model with backward selection to identify predictors. The p value for statistical significance was set at p < 0.05.
Results
In total, 140 out of 2045 (7%) patients with a proximal femoral fracture who were admitted within the study period matched the inclusion criteria. The median age at trauma was 85 (P25–P75 80–89) years. Eighty-seven (62%) patients were female. Baseline characteristics are summarized in Table 1. Half of the patients received home care for support for performing ADL, with a median of daily visits of home care of 2 (P25–P75 2–3). Most falls occurred in the domestic setting (n = 125; 89%).
Facture and treatment characteristics
Displaced femoral neck fractures were the most frequent fracture type (Table 2). In 26 (19%) patients, there were concomitant traumatic injuries or clinical abnormalities in the pre-operative screening (such as urinary tract infections and electrolyte abnormalities). Initially, 132 patients opted for surgical management. Non-operative management (NOM) was primarily opted for by eight (6%) patients due to the high perioperative risks of mortality related to cardiac comorbidities or poor health status. Due to clinical deterioration during the pre-operative waiting period, 6 additional patients (5%) who primarily opted for surgery (n = 132) were no longer considered suitable candidates for operative treatment.
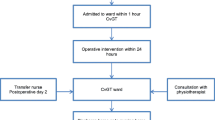
In total, 126 (90%) patients were treated surgically and 14 (10%) were managed non-operatively. Seventy-four (59%) patients were operated on within 24 h after ED admission. The median time to surgery was 21 h (P25–P75 15–32). Spinal anesthesia was performed in 54 (43%) patients.
Mortality
Within 6 months post-trauma, 58 (41%) patients died. Twenty (14%) patients died during the index hospital stay. For operatively treated patients (n = 126), the 30-day, 3-month, and 6-month mortality rates were 15% (n = 19), 27% (n = 34), and 35% (n = 44), respectively, with a median time to death of 39 days (P25–P75 15–73). All patients who were eventually managed non-operatively died within 30 days (n = 14) with a median time to death of 5 days (P25–P75 3–8). Ten non-operatively treated patients (71%) died during the hospital stay.
Adverse events
A total of 216 adverse events occurred in 102 patients (73% of total) during the study period. Table 3 shows an overview of adverse events. In total, 25 surgery-related adverse events occurred in 20 (14%) patients. Nine reoperations were registered in 6 patients (4% of total) within the study period. Delirium (n = 34; 24%), pneumonia (n = 34; 24%), pressure ulcers (n = 23; 17%), and urinary tract infections (n = 24; 17%) were the most common adverse events. Three-quarters of the adverse events occurred during the primary hospital stay. In addition, 7 (5%) patients required physical restraints to prevent adverse events and 54 (39%) patients had a blood transfusion. Forty-six (33%) patients were given antipsychotic drugs during admission. Significantly more patients required transfusion in the pertrochanteric/subtrochanteric fracture group than in the femoral neck fracture group (49% vs 30%, p = 0.025).
Health care consumption
The median length of stay was 9 days (IQR 6–14). Patients were often managed by multiple disciplines. A total of 578 (para)medic specialisms other than the primary treating (orthopedic) trauma surgeon were consulted during the index admission (median of 4 consultations per patient (IQR 3–5)). Patients were comanaged by geriatricians in all but two patients. In total, 36% of the patients were screened and/or treated by a cardiologist, 21% by internists, 18% by an anesthesiologist (for judgment if patients were operable), 13% by a pulmonologist, 10% by a neurologist, 10% by an intensive care physician, and 7% by a urologist. A physical therapist was involved in 92% of the patients, a dietitian in 61%, occupational therapist in 9%, speech therapists in 9%, and spiritual caregivers in 13%. The palliative care team was involved in 15% of the cases of which 13 out of 21 consults were requested in surgically treated patients. In total, 17 (12%) patients required admittance in the post-anesthesia care unit, intensive care unit, or cardiac care unit.
Hospital care use post-discharge
Out of the 120 patients who survived to discharge, 33 (28%) were readmitted to the ED, and 29 (24%) were readmitted to the hospital during the study period. Reasons for hospital readmission are displayed in Table 3.
Sixty of the 120 (50%) patients revisited to the hospital for an outpatient follow-up. In 41 (68%) patients, this was for a regular follow-up with the surgeon, in 10 (17%) patients because of adverse symptoms or follow-up of adverse events, and in 9 (15%) patients for a combination of both.
Residency
Table 4 provides an overview of the residency, ADL (in)dependency, and mobility. Out of the 120 patients who survived the index submission, 105 (87%) were institutionalized at discharge. Most patients were discharged to a rehabilitation center (73% of the cases). Seven (8%) patients were discharged to a hospice and one patient with palliative care to his own home. At 3 months and 6 months post-trauma, one-third (n = 29) and 50% (n = 41) of the patients returned to their community home after hospital discharge, respectively. In total, 59 out of the 120 (49%) patients returned to their own home at any time during the 6-month study period.
Mobility and ADL (in)dependency
At hospital discharge, 42 (35%) patients were unable to ambulate. At 6 months post-trauma, 32 (39%) patients were able to achieve outdoor mobilization with or without aids versus 111 (79%) in the pre-fracture situation.
At discharge, only 14% (n = 17/120) regained their previous level of mobility. After 3 months, this was 39% (n = 35/89). After 6 months, only 29% (n = 24/82) of the patients still alive achieved a recovery to their pre-trauma PMS. In total, 39 out of the 140 patients (28%) regained their pre-trauma level of mobility at any time during the study period.
With regard to ADL, 36% of the patients who survived to 3 months regained their previous level of ADL (in)dependency. At 3 months, only 26 (30%) of the surviving patients lived completely ADL independent, compared to 70 (50%) at the pre-fracture level.
Predictors for mortality, institutionalization, and not regaining pre-fracture mobility
Univariate logistic regression showed that age (OR 1.07; 95% CI 1.01–1.12), ASA score of 4 (OR 3.47; 95% CI 1.65–7.27), PMS (mobile with aids [OR 2.04; 95% CI 0.88–4.71] and indoor confined [OR 2.73; 95% CI 1.00–7.48]), and patients who received home care prior to the trauma (OR 2.14; 95% CI 1.08–4.26) were predictive for death within 6 months post-trauma with a p value < 0.10 (Table 5). Multivariable analysis only identified ASA class 4 (OR 4.27; 95% CI 1.90–9.61) and age (OR 1.07; 95% CI 1.00–1.14) as significant predictors for death within 6 months. With regard to extrinsic factors, the type of implant (p = 0.095) and the type of anesthesia (p = 0.483) were not associated with an increased risk of mortality within 6 months. Time to surgery ≥ 48 h was significantly associated with mortality compared to surgery < 48 h (67% [n = 7/11] vs 32% [n = 36/114], p = 0.024). However, three out of the 7 patients that had delayed surgery ≥ 48 h were found to have infectious disease during pre-operative screening. When these patients were excluded, the effect of delayed surgery was no longer found to be statistically significant (p = 0.574).
With regard to institutionalization at 6 months, univariate logistic regression showed that age (OR 1.13; 95% CI 1.07–1.20), pre-fracture PMS (mobile with aids [OR 4.50; 95% CI 1.95–10.40] and indoors confined [OR 5.91; 95% CI 2.04–16.06]), and patients who received home care prior to the trauma (OR 5.09; 95% CI 2.44–10.60) were predictive factors (Table 5). Multivariate analysis only identified age (OR 1.09; 95% CI 1.02–1.16) and patients receiving home care for ADL prior to trauma (OR 2.60; 95% CI 1.01–6.68) as significant predictors for failing to return to their previous residency.
With regard to not regaining pre-fracture PMS, univariate logistic regression showed that only age (OR 1.06; 95% CI 1.01–1.13) and ASA class 4 (OR 2.72; 95% CI 1.12–5.95) were predictive factors (Table 5). In multivariate analysis, age (OR 1.06; 95% CI 1.01–1.13) and ASA class 4 (OR 2.72; 95% CI 1.25–5.95) remained to be significant predictors.
Discussion
The results of this study show that the prognosis of frail community-dwelling older patients with a proximal femoral fracture is generally poor. Despite multidisciplinary efforts of rehabilitation and significant health care consumption, one-third of the patients do not recover with regard to their pre-trauma PMS, high mortality rates are found, and only half of the patients who survived till hospital discharge returned home within 6 months post-trauma.
This suggests that these community-dwelling patients are at a crossroads; they either make a timely recovery to their pre-trauma functioning or are able to return to home or they experience progressive clinical deterioration with unsuccessful rehabilitation with a high risk of mortality. Presumably, for those patients who are physically frail, a proximal femoral fracture disturbs the delicate equilibrium of their residual-independent mobility and could provoke a downwards spiral.
This study corroborates and extends the current increasing evidence of the poor prognosis of frail older patients with a proximal femoral fracture, whereas previous studies describing mortality in Dutch patients with a proximal femoral fracture aged over 65 years have shown mortality rates of 17.7% after 1 year, 23% for patients aged between 65 and 89, and 43% of patients aged ≥ 90 after 1 year; the mortality rate for this specific study was much higher (44% at 6 months) [19, 32]. This excess mortality is most likely attributable due to the frailty of the patient population as previous studies have already shown an increased risk of adverse outcomes in frail patients [11, 12, 21,22,23]. In addition, the risk of mortality of the average 84-year-old resident in 2020 in the Netherlands is about 7.6% per year, reiterating the significant effect of a proximal femoral fracture and frailty on the prognosis [33].
The treatment of patients with a proximal femoral fracture typically entails hospitalization followed by an often lengthy rehabilitation period [34]. However, this rehabilitation period can be intensive while a return to previous levels of functioning is not a certainty. In addition, (temporary) institutionalization for community reintegration is often required. This pattern was also the case in our study, as the rate of institutionalization at discharge was almost 90%. Similar rates of institutionalization of approximately 70% and 85% in community-dwelling patients were found by previous studies in their cohorts [35, 36]. Despite the attempts of institutionalized rehabilitation, return to previous levels of functioning is not a given fact as results showed that approximately one-third did not return to their pre-trauma level of mobility and approximately 25% of the surviving patients were not mobile outdoors at 6 months post-trauma. Among others, Mariconda et al. [37] reported unsuccessful recovery of 43% after 1 year. These data and our key findings are in concordance with other current literatures [20, 32, 38].
As reported by Brown et al. [39], improvement of functioning following a proximal femoral fracture mainly occurs within the first 3 months. After this period, only minimal improvements can be expected [39]. This timeframe of recovery was also reflected in the data in our study. This stresses the importance of early mobilization and an early start of the rehabilitation process which mainly entails adequate pain control and the prevention of postoperative adverse events that hamper mobilization.
This retrospective study had some limitations. Important factors such as (HR)QoL, self-perceived level of recovery, pain, fear of falling, and other dimensions (e.g., social support) were not assessed. Furthermore, due to the retrospective nature of this study, no information on mobility and residence was available if patients did not revisit the hospital, died in the follow-up period, or had missing data in the 3-month dataset in the DHFA. In addition, frailty criteria based on validated frailty scales or indices could not be used to identify frail patients within the study period due to the retrospective nature of this study. Although the described cohort formally cannot be described as frail, only a specific subset of community-dwelling older patients was included that represented only 7% of the total patient population with a proximal femoral fracture within the study period. The poor outcomes of this specific group were poor, and therefore, the described cohort is very likely to feature a high degree of frailty and was therefore labeled as frail. In addition, the separate indicators for frailty (comorbidities, BMI, and decreased mobility) have been described as separate risk factors for poor outcomes and are easily reproducible and quantifiable.
Even though this cohort is one of the larger cohorts featuring frail community-dwelling patients, multivariable logistic regression analysis was limited due to sample size and by the fact that only the frailest patients were included in this analysis. The multivariable analysis should therefore be interpreted with caution. Prediction of definitive institutionalization remains difficult. Previous data from the DHFA in the Netherlands showed that age, pre-fracture PMS, pre-morbid Katz ADL score, surgical treatment, ASA score, type of anesthesia, history of dementia, and cotreatment by a geriatrician were early independent predictors for institutionalization [40].
Despite these limitations, this study is unique in the way that it addresses a specific subpopulation of frail community-dwelling patients with a worse prognosis than described in previous studies addressing community-dwelling patients based on age or other frailty indicators [5, 11, 12].
The findings have several implications. First, the results of this study can be used especially for realistic expectation management and aid in better decision making, since there is a high chance of unfavorable outcomes in this patient group. Realistic expectations by patients or caregivers will most likely result in higher treatment satisfaction and clearer goals of care. It must be made clear that recovery to previous levels of functioning is often not likely. Second, it is very important to identify those patients who are unlikely to (re)obtain mobility and survive to a longer term, not only to provide realistic expectations but also to timely engage in end-of-life conversation. Treatment options should be openly discussed for those at high risk of not regaining mobility with consequent institutionalization and for those at high risk of adverse events with the reduced quality of life, ADL dependence, and the discomfort that it presumably results in. In this small subgroup within an already selected patient population, it should be questioned if surgery, or in case of postoperative clinical deterioration an intensive rehabilitation program, is the best treatment option depending on their goals of care and motivation. However, this only accounts for a very small subset of patients as a significant proportion of the surviving patients make a clinical recovery. Lastly, because of the high rate of institutionalization at discharge, requests for a transfer to a rehabilitation setting or ADL assistance should be timely arranged in this specific patient group to prevent unnecessary delays in transfers and unnecessary occupation of hospital beds.
Conclusion
Frail community-dwelling older patients with a proximal femoral fracture have a high risk of death, adverse events, and institutionalization and often do not reobtain their pre-trauma level of mobility and independence at 6 months post-trauma. Foremost, the results can be used for realistic expectation management, improved shared decision making, advance care planning in the community, and health care planning.
Data Availability
Relevant anonymized data on individual patients for meta-analysis purposes can be provided upon reasonable request to the corresponding author.
References
Peeters CM, Visser E, Van de Ree CL, Gosens T, Den Oudsten BL, De Vries J (2016) Quality of life after hip fracture in the elderly: a systematic literature review. Injury 47(7):1369–1382
Marottoli RA, Berkman LF, Cooney LM Jr (1992) Decline in physical function following hip fracture. J Am Geriatr Soc 40(9):861–866
Magaziner J, Hawkes W, Hebel JR, Zimmerman SI, Fox KM, Dolan M et al (2000) Recovery from hip fracture in eight areas of function. J Gerontol A Biol Sci Med Sci 55(9):M498-507
Dyer SM, Crotty M, Fairhall N, Magaziner J, Beaupre LA, Cameron ID et al (2016) A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr 16:158
van de Ree CLP, Landers MJF, Kruithof N, de Munter L, Slaets JPJ, Gosens T, et al. Effect of frailty on quality of life in elderly patients after hip fracture: a longitudinal study. BMJ Open. 2019;9(7):e025941.
Alexiou KI, Roushias A, Varitimidis SE, Malizos KN (2018) Quality of life and psychological consequences in elderly patients after a hip fracture: a review. Clin Interv Aging 13:143–150
Beaupre LA, Jones CA, Johnston DW, Wilson DM, Majumdar SR (2012) Recovery of function following a hip fracture in geriatric ambulatory persons living in nursing homes: prospective cohort study. J Am Geriatr Soc 60(7):1268–1273
Neuman MD, Silber JH, Magaziner JS, Passarella MA, Mehta S, Werner RM (2014) Survival and functional outcomes after hip fracture among nursing home residents. JAMA Intern Med 174(8):1273–1280
Morrison RS, Siu AL (2000) Survival in end-stage dementia following acute illness. JAMA 284(1):47–52
Berry SD, Rothbaum RR, Kiel DP, Lee Y, Mitchell SL (2018) Association of clinical outcomes with surgical repair of hip fracture vs nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med 178(6):774–780
Jorissen RN, Lang C, Visvanathan R, Crotty M, Inacio MC. The effect of frailty on outcomes of surgically treated hip fractures in older people. Bone. 2020;136:115327.
Krishnan M, Beck S, Havelock W, Eeles E, Hubbard RE, Johansen A (2014) Predicting outcome after hip fracture: using a frailty index to integrate comprehensive geriatric assessment results. Age Ageing 43(1):122–126
Ministerie van Volksgezondheid WeSMoH, wellbeing and sports. 18–06–2018 [Available from: ttps://www.programmalangerthuis.nl/binaries/programmalangerthuis/documenten/rapporten/2018/06/18/programmaplan-langer-thuis/programma-langer-thuis.pdf.
Landelijk Netwerk Acute Zorg. LTR factsheet 2012. Acute ziekenhuisopnames voor heupfracturen. 2013 [Available from: http://www.lnaz.nl/cms/LTR_2012_Factsheetheupfracturen_140611.pdf.
Dutch Hip Fracture Audit. jaarrapportage 2019 [Available from: https://dica.nl/jaarrapportage-2019/dhfa].
Ouellet JA, Ouellet GM, Romegialli AM, Hirsch M, Berardi L, Ramsey CM et al (2019) Functional outcomes after hip fracture in independent community-dwelling patients. J Am Geriatr Soc 67(7):1386–1392
Aboelmagd T, Dainty JR, MacGregor A, Smith TO (2018) Trajectory of physical activity after hip fracture: an analysis of community-dwelling individuals from the English Longitudinal Study of Ageing. Injury 49(3):697–701
Finsterwald M, Sidelnikov E, Orav EJ, Dawson-Hughes B, Theiler R, Egli A et al (2014) Gender-specific hip fracture risk in community-dwelling and institutionalized seniors age 65 years and older. Osteoporos Int 25(1):167–176
Kanters TA, van de Ree CLP, de Jongh MAC, Gosens T, Hakkaart-van RL (2020) Burden of illness of hip fractures in elderly Dutch patients. Arch Osteoporos 15(1):11
Salpakoski A, Tormakangas T, Edgren J, Sihvonen S, Pekkonen M, Heinonen A, et al. Walking recovery after a hip fracture: a prospective follow-up study among community-dwelling over 60-year old men and women. Biomed Res Int. 2014;2014:289549.
Winters AM, Hartog LC, Roijen H, Brohet RM, Kamper AM (2018) Relationship between clinical outcomes and Dutch frailty score among elderly patients who underwent surgery for hip fracture. Clin Interv Aging 13:2481–2486
Patel KV, Brennan KL, Brennan ML, Jupiter DC, Shar A, Davis ML (2014) Association of a modified frailty index with mortality after femoral neck fracture in patients aged 60 years and older. Clin Orthop Relat Res 472(3):1010–1017
Morri M, Ambrosi E, Chiari P, Orlandi Magli A, Gazineo D, F DA, et al. One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. 2019;9(1):18718.
Xu BY, Yan S, Low LL, Vasanwala FF, Low SG (2019) Predictors of poor functional outcomes and mortality in patients with hip fracture: a systematic review. BMC Musculoskelet Disord 20(1):568
Holden MK, Gill KM, Magliozzi MR, Nathan J, Piehl-Baker L (1984) Clinical gait assessment in the neurologically impaired. Reliab Meaning Phys Ther 64(1):35–40
Kastanis G, Topalidou A, Alpantaki K, Rosiadis M, Balalis K (2016) Is the ASA score in geriatric hip fractures a predictive factor for complications and readmission? Scientifica (Cairo) 2016:7096245
Wolters U, Wolf T, Stutzer H, Schroder T (1996) ASA classification and perioperative variables as predictors of postoperative outcome. Br J Anaesth 77(2):217–222
Skeie E, Tangvik RJ, Nymo LS, Harthug S, Lassen K, Viste A (2020) Weight loss and BMI criteria in GLIM’s definition of malnutrition is associated with postoperative complications following abdominal resections - results from a National Quality Registry. Clin Nutr 39(5):1593–1599
Smith T, Pelpola K, Ball M, Ong A, Myint PK (2014) Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Age 43(4):464–471
Charlson M, Charlson RE, Briggs W, Hollenberg J (2007) Can disease management target patients most likely to generate high costs? The impact of comorbidity. J Gen Intern Med 22(4):464–469
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457
Vochteloo AJ, Borger van der Burg BL, Tuinebreijer WE, de Vries MR, Niggebrugge AH, Bloem RM, et al. Do clinical characteristics and outcome in nonagenarians with a hip fracture differ from younger patients? Geriatr Gerontol Int. 2013;13(1):190–7.
Central Bureau of Statistics. Life expectancy, gender, age (per year and period of five years, 09–06–2020 [Available from: https://opendata.cbs.nl/#/CBS/nl/dataset/37360ned/table].
Ponten JB, Krug E, van Baardewijk LJ, van der Linden EH, Haas R, Krijnen P et al (2015) Intensive rehabilitation in selected hip fracture patients may optimize care efficiency: a retrospective comparison study. J Rehabil Med 47(3):278–281
Becker DJ, Arora T, Kilgore ML, Curtis JR, Delzell E, Saag KG et al (2014) Trends in the utilization and outcomes of Medicare patients hospitalized for hip fracture, 2000–2008. J Aging Health 26(3):360–379
Beaupre L, Sobolev B, Guy P, Kim JD, Kuramoto L, Sheehan KJ et al (2019) Discharge destination following hip fracture in Canada among previously community-dwelling older adults, 2004–2012: database study. Osteoporos Int 30(7):1383–1394
Mariconda M, Costa GG, Cerbasi S, Recano P, Orabona G, Gambacorta M et al (2016) Factors predicting mobility and the change in activities of daily living after hip fracture: a 1yYear prospective cohort study. J Orthop Trauma 30(2):71–77
Intiso D, Di Rienzo F, Grimaldi G, Lombardi T, Fiore P, Maruzzi G et al (2009) Survival and functional outcome in patients 90 years of age or older after hip fracture. Age Ageing 38(5):619–622
Brown K, Cameron ID, Keay L, Coxon K, Ivers R (2017) Functioning and health-related quality of life following injury in older people: a systematic review. Inj Prev 23(6):403–411
van Dartel D, Vermeer M, Folbert EC, Arends AJ, Vollenbroek-Hutten MMR, Hegeman JH, et al. Early predictors for discharge to geriatric rehabilitation after hip fracture treatment of older patients. J Am Med Dir Assoc. 2021.
Funding
SAIL, MHJV, EMMVL, and PJ received financial support from the Netherlands Organization for Health Research and Development (ZonMw; ref.nr. 843004120) and Osteosynthesis and Trauma Care Foundation (ref.nr. 2019-PJKP) for the submitted work. The authors have no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years and no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study has been exempted by the Medical Research Ethics Committee of VU University Medical Center according to article 7 of the Medical Research Involving Human Subjects Act (ref.no. 2019.578). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Loggers, S.A.I., Nijdam, T.M.P., Folbert, E.C. et al. Prognosis and institutionalization of frail community-dwelling older patients following a proximal femoral fracture: a multicenter retrospective cohort study. Osteoporos Int 33, 1465–1475 (2022). https://doi.org/10.1007/s00198-022-06394-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06394-y