Abstract
Introduction and Hypothesis
Obstetric anal sphincter injury (OASI) is a major complication associated with vacuum-assisted vaginal delivery (VAVD). The aim of this study was to evaluate risk factors related to vacuum extraction that are associated with OASI.
Methods
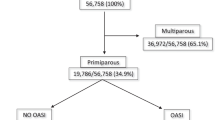
This was a case–control study performed at a tertiary university teaching hospital. Included were patients aged 18–45 years who had a singleton pregnancy resulting in a live, term, VAVD. The study group consisted of women diagnosed with OASI following vacuum extraction. The control group included women following VAVD without OASI. Matching at a ratio of 1:2 was performed. Groups were compared regarding demographic, obstetric. and labor-related parameters, specifically focusing on variables related to the vacuum procedure itself.
Results
One hundred and ten patients within the study group and 212 within the control group were included in the final analysis. Patients in the OASI group were more likely to undergo induction of labor, use of oxytocin during labor, increased second stage of labor, higher likelihood of the operator being a resident, increased number of pulls, procedure lasting under 10 min, occipito-posterior head position at vacuum initiation, episiotomy, increased neonatal head circumference, and birthweight. Multivariate logistic regression analysis revealed that increased week of gestation (OR 1.67, 95% CI 1.25–2.22, p < 0.001), unsupervised resident performing the procedure (OR 4.63, 95% CI 2.17–9.90), p < 0.001), indication of VAVD being fetal distress (OR 2.72, 95% CI 1.04–7.10, p = 0.041), and length of procedure under 10 min (OR 4.75, 95% CI 1.53–14.68, p = 0.007) were associated with OASI. Increased maternal age was associated with lower risk of OASI (OR 0.9, 95% CI 0.84–0.98, p = 0.012).
Conclusions
When performing VAVD, increased week of gestation, unsupervised resident performing the procedure, fetal distress as vacuum indication, and vacuum procedure under 10 min were associated with OASI. In contrast, increased maternal age was shown to be a protective factor.

Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Poignant M, Hjelmstedt A, Ekeus C. Indications for operative delivery between 1999–2010 and induction of labor and epidural analgesia on the risk of operative delivery—a population based Swedish register study. Sex Reprod Health. 2012;3:129–34.
Mola GD, Kuk J. Operative vaginal delivery at Port Moresby General Hospital from 1977 to 2010. P N G Med J. 2011;54(3–4):174–84.
Cammu H, Martens G, Keirse MJ. Mothers’ level of education and childbirth interventions: a population-based study in Flanders, Northern Belgium. Birth. 2011;38(3):191–9.
Kramer MS, Berg C, Abenhaim H, et al. Incidence, risk factors, and temporal trends in severe postpartum hemorrhage. Am J Obstet Gynecol. 2013;209(5):449.e1–7.
Sheiner E, Sarid L, Levy A, Seidman DS, Hallak M. Obstetric risk factors and outcome of pregnancies complicated with early postpartum hemorrhage: a population-based study. J Matern Fetal Neonatal Med. 2005;18:149–54.
Hildingsson I, Karlstrom A, Nystedt A. Parents’ experiences of an instrumental vaginal birth findings from a regional survey in Sweden. Sex Reprod Healthc. 2013;4:3–8.
Ekéus C, Nilsson E, Gottvall K. Increasing incidence of anal sphincter tears among primiparas in Sweden: a population-based register study. Acta Obstet Gynecol Scand. 2008;87:564–73.
De Leeuw JW, Struijk PC, Vierhout ME, Wallenburg HC. Risk factors for third degree perineal ruptures during delivery. BJOG. 2001;108:383–7.
Handa VL, Danielsen BH, Gilbert WM. Obstetric anal sphincter lacerations. Obstet Gynecol. 2001;98:225–30.
Christianson LM, Bovbjerg VE, McDavitt EC, Hullfish KL. Risk factors for perineal injury during delivery. Am J Obstet Gynecol. 2003;189:255–60.
Jango H, Langhoff-Roos J, Rosthoj S, Sakse A. Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol. 2013;210(1):59.e1–6.
Gurol-Urganci I, Cromwell DA, Edozien LC, et al. Third- and fourth-degree perineal tears among primiparous women in England between 2000 and 2012: time trends and risk factors. BJOG. 2013;120:1516–25.
Bergendahl S, Lindberg P, Brismar WS. Operator experience affects the risk of obstetric anal sphincter injury in vacuum extraction deliveries. Acta Obstet Gynecol Scand. 2019;98:787–94.
Ryman P, Ahlberg M, Ekeus C. Risk factors for anal sphincter tears in vacuum-assisted delivery. Sex Reprod Healthc. 2015;6(3):151–6.
Waldman R. ACOG practice bulletin No. 198: prevention and management of obstetric lacerations at vaginal delivery. Obstet Gynecol. 2019;133(1):185.
Chill HH, Guedalia J, Lipschuetz M, et al. Prediction model for obstetric anal sphincter injury using machine learning. Int Urogynecol J. 2021;32(9):2393–9.
Nakai A, Yoshida A, Yamaguchi S, et al. Incidence and risk factors for severe perineal laceration after vaginal delivery in Japanese patients. Arch Gynecol Obstet. 2006;274(4):222–6.
Meister MR, Cahill AG, Conner SN, et al. Predicting obstetric anal sphincter injuries in a modern obstetric population. Am J Obstet Gynecol. 2016;215(3):310.e1–7.
Segal D, Baumfeld Y, Yahav L, et al. Risk factors for obstetric anal sphincter injuries (OASIS) during vacuum extraction delivery in a university affiliated maternity hospital. J Matern Fetal Neonatal Med. 2020;33(6):999–1003.
Levin G, Friedman T, Shai D, Alcalay M, Ram E, Meyer R. The association between vacuum-assisted vaginal delivery and anal sphincter injury. Int Urogynecol J. 2021;32(7):1771–7.
Bligard KH, Lipsey KL, Young OM. Simulation training for operative vaginal delivery among obstetrics and gynecology residents: a systematic review. Obstet Gynecol. 2019;134(Suppl 1):16S–21S.
Mannella P, Giordano M, Guevara MMM, et al. Simulation training program for vacuum application to improve technical skills in vacuum-assisted vaginal delivery. BMC Pregnancy Childbirth. 2021;21(1):338.
Celentano C, Prefumo F, Matarrelli B, Mastracchio J, Mauri S, Rosati M. Comparison of practice vs theory model training for vacuum-assisted delivery: a randomized controlled trial. Eur J Obstet Gynecol Reprod Biol. 2023;290:109–14.
Chill HH, Lipschuetz M, Atias E, et al. Obstetric anal sphincter injury in adolescent mothers. BMC Pregnancy Childbirth. 2021;21(1):564.
Levin G, Rottenstreich A, Tsur A, et al. Risk factors for obstetric anal sphincter injury among parous women. Arch Gynecol Obstet. 2021;303(3):709–14.
Dey T, Mukherjee A, Chakraborty S. A practical overview of case-control studies in clinical practice. Chest. 2020;158(1S):S57–64.
Author information
Authors and Affiliations
Contributions
H.H.C.: project development, data collection, data analysis, manuscript writing and editing; A.D.: data collection, data analysis, manuscript writing, and editing; W.Z.: data collection, data analysis, manuscript editing; N.V.A.: data collection, data analysis; J.I.R.: data analysis, manuscript writing, and editing; D.S.: project development, data analysis, manuscript writing, and editing; G.K.: project development, data collection, data analysis, manuscript writing, and editing.
Corresponding author
Ethics declarations
Financial Support
None.
Ethics Statement
This study was approved by the Human Investigation Review Board of Hadassah Medical Center, Hebrew University of Jerusalem (IRB# 0586-22-HMO).
Conflicts of Interest
None.
Additional information
Handling Editor: Gin-Den Chen
Editor in Chief: Maria A. Bortolini
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chill, H.H., Dick, A., Zarka, W. et al. Factors Associated with Obstetric Anal Sphincter Injury During Vacuum-Assisted Vaginal Delivery. Int Urogynecol J (2024). https://doi.org/10.1007/s00192-024-05785-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00192-024-05785-5