Abstract
Introduction and hypothesis
The objective was to investigate the rate of adherence to pessary treatment for pelvic organ prolapse (POP), to identify factors associated with long-term (longer than 1 year) use of vaginal pessaries in Brazilian women with POP and its impact on quality of life (QoL).
Methods
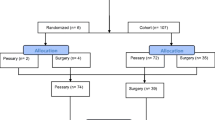
A prospective observational study assessed 247 consecutive women candidates for a pessary to manage symptomatic POP. Patients were fitted with a ring pessary and follow-up visits were performed at 1, 6, and 12 months. Pessary complications and reasons for discontinuation were recorded. Prolapse Quality of Life Questionnaire (P-QoL) was applied at baseline and after 1 year of treatment. We used a logistic regression model for the analyses, with p < 0.05 for significance.
Results
A total of 236 women were included in the study, of whom 110 (46.6%) maintained the pessary treatment for longer than 12 months. The main reason for pessary discontinuation was the patient opting for surgery (50.8%). Vulvovaginitis was the main long-term complication (44.5%), followed by vaginal ulceration (16.4%) and urinary urgency (10%). No prior hysterectomy (OR = 2.26; 95% CI 1.19–4.31), vaginal estrogen use (OR = 1.94; 95% CI 1.06–3.52), and mean age (OR = 1.03; 95% CI 1.01–1.06) were variables associated with long-term use of vaginal pessary (p < 0.05 for all). Total P-QoL score significantly changed with pessary use (519.1 at baseline and 260 after 12-month treatment, p < 0.00).
Conclusions
Our study suggests that no prior hysterectomy, the local estrogen therapy, and age might be factors associated with use of a ring vaginal pessary for longer than 1 year. Long-term pessary users had a significant improvement in their quality of life.

Similar content being viewed by others
Abbreviations
- BMI:
-
Body mass index
- OD:
-
Odds ratio
- POP:
-
Pelvic organ prolapse
- POP-Q:
-
Pelvic Organ Prolapse Quantification
- P-QoL:
-
Prolapse Quality of Life Questionnaire
- QoL:
-
Quality of life
- SD:
-
Standard deviation
- SPSS:
-
Statistical Package for Social Sciences
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
References
Nygaard I, Barber MD, Burgio KL, et al. Pelvic floor disorders network. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008;300(11):1311–6. https://doi.org/10.1001/jama.300.11.1311.
AUGS Best Practice Statement. Evaluation and counseling of patients with pelvic organ prolapse. Female Pelvic Med Reconstr Surg. 2018;24(3):256. https://doi.org/10.1097/SPV.0000000000000566.
Thakar R, Stanton S. Management of genital prolapse. BMJ. 2002;324(7348):1258–62. https://doi.org/10.1136/bmj.324.7348.1258.
Pelvic Organ Prolapse. ACOG practice bulletin, number 214. Obstet Gynecol. 2019;134(5):e126–42. https://doi.org/10.1097/AOG.0000000000003519.
NICE Guidance—urinary incontinence and pelvic organ prolapse in women: management: © NICE (2019) Urinary incontinence and pelvic organ prolapse in women: management. BJU Int. 2019;123(5):777–803. https://doi.org/10.1111/bju.14763.
Kapoor DS, Nemcova M, Pantazis K, Brockman P, Bombieri L, Freeman RM. Reoperation rate for traditional anterior vaginal repair: analysis of 207 cases with a median 4-year follow-up. Int Urogynecol J. 2010;21(1):27–31. https://doi.org/10.1007/s00192-009-0991-x.
Cundiff GW, Weidner AC, Visco AG, Bump RC, Addison WA. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95(6 Pt 1):931–5. https://doi.org/10.1016/s0029-7844(00)00788-2.
De Albuquerque Coelho SC, de Castro EB, Juliato CR. Female pelvic organ prolapse using pessaries: systematic review. Int Urogynecol J. 2016;27(12):1797–803. https://doi.org/10.1007/s00192-016-2991-y.
Ramsay S, Tu le M, Tannenbaum C. Natural history of pessary use in women aged 65–74 versus 75 years and older with pelvic organ prolapse: a 12-year study. Int Urogynecol J. 2016;27(8):1201–7. https://doi.org/10.1007/s00192-016-2970-3.
Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG. 2009;116(13):1715–21. https://doi.org/10.1111/j.1471-0528.2009.02380.x.
Lone F, Thakar R, Sultan AH, Karamalis G. A 5-year prospective study of vaginal pessary use for pelvic organ prolapse. Int J Gynaecol Obstet. 2011;114(1):56–9. https://doi.org/10.1016/j.ijgo.2011.02.006.
Ma C, Zhou Y, Kang J, et al. Vaginal pessary treatment in women with symptomatic pelvic organ prolapse: a long-term prospective study. Menopause. 2021;28(5):538–45. https://doi.org/10.1097/GME.0000000000001751.
De Albuquerque Coelho SC, Brito LGO, de Araujo CC, Juliato CRT. Factors associated with unsuccessful pessary fitting in women with symptomatic pelvic organ prolapse: systematic review and metanalysis. Neurourol Urodyn. 2020;39(7):1912–21. https://doi.org/10.1002/nau.24458.
Bugge C, Adams EJ, Gopinath D, et al. Pessaries (mechanical devices) for managing pelvic organ prolapse in women. Cochrane Database Syst Rev. 2020;11(11):CD004010. https://doi.org/10.1002/14651858.CD004010.pub4.
Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Epidemiology. 2007;18(6):800–4. https://doi.org/10.1097/EDE.0b013e3181577654.
Scarlato A, Souza CC, Fonseca ES, Sartori MG, Girão MJ, Castro RA. Validation, reliability, and responsiveness of prolapse quality of life questionnaire (P-QOL) in a Brazilian population. Int Urogynecol J. 2011;22(6):751–5. https://doi.org/10.1007/s00192-010-1354-3.
Yimphong T, Temtanakitpaisan T, Buppasiri P, Chongsomchai C, Kanchaiyaphum S. Discontinuation rate and adverse events after 1 year of vaginal pessary use in women with pelvic organ prolapse. Int Urogynecol J. 2018;29(8):1123–8. https://doi.org/10.1007/s00192-017-3445-x.
Wu V, Farrell SA, Baskett TF, Flowerdew G. A simplified protocol for pessary management. Obstet Gynecol. 1997;90(6):990–4. https://doi.org/10.1016/s0029-7844(97)00481-x.
Li B, Chen Q, Zhang J, Yu C, Zhang L, Chen L. A prospective study of pessary use for severe pelvic organ prolapse: 3-year follow-up outcomes. Arch Gynecol Obstet. 2020;301(5):1213–8. https://doi.org/10.1007/s00404-020-05526-1.
Clemons JL, Aguilar VC, Sokol ER, Jackson ND, Myers DL. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Am J Obstet Gynecol. 2004;191(1):159–64. https://doi.org/10.1016/j.ajog.2004.04.048.
Wolff B, Williams K, Winkler A, Lind L, Shalom D. Pessary types and discontinuation rates in patients with advanced pelvic organ prolapse. Int Urogynecol J. 2017;28(7):993–7. https://doi.org/10.1007/s00192-016-3228-9.
Friedman S, Sandhu KS, Wang C, Mikhail MS, Banks E. Factors influencing long-term pessary use. Int Urogynecol J. 2010;21(6):673–8. https://doi.org/10.1007/s00192-009-1080-x.
Dueñas JL, Miceli A. Effectiveness of a continuous-use ring-shaped vaginal pessary without support for advanced pelvic organ prolapse in postmenopausal women. Int Urogynecol J. 2018;29(11):1629–36. https://doi.org/10.1007/s00192-018-3586-6.
Manonai J, Sarit-Apirak S, Udomsubpayakul U. Vaginal ring pessary use for pelvic organ prolapse: continuation rates and predictors of continued use. Menopause. 2018;26(6):665–9. https://doi.org/10.1097/GME.0000000000001277.
Mao M, Xu T, Kang J, et al. Factors associated with long-term pessary use in women with symptomatic pelvic organ prolapse. Climacteric. 2019;22(5):478–82. https://doi.org/10.1080/13697137.2019.1582623.
Manchana T. Ring pessary for all pelvic organ prolapse. Arch Gynecol Obstet. 2011;284(2):391–5. https://doi.org/10.1007/s00404-010-1675-y.
Geoffrion R, Zhang T, Lee T, Cundiff GW. Clinical characteristics associated with unsuccessful pessary fitting outcomes. Female Pelvic Med Reconstr Surg. 2013;19(6):339–45. https://doi.org/10.1097/SPV.0b013e3182a26174.
Mao M, Ai F, Zhang Y, et al. Predictors for unsuccessful pessary fitting in women with symptomatic pelvic organ prolapse: a prospective study. BJOG. 2018;125(11):1434–40. https://doi.org/10.1111/1471-0528.15260.
Ma C, Kang J, Xu T, et al. Vaginal pessary continuation in symptomatic pelvic organ prolapse patients with prior hysterectomy. Menopause. 2020;27(10):1148–54. https://doi.org/10.1097/GME.0000000000001633.
Mendes LC, Bezerra LRPS, Bilhar APM, et al. Symptomatic and anatomic improvement of pelvic organ prolapse in vaginal pessary users. Int Urogynecol J. 2021;32(4):1023–9. https://doi.org/10.1007/s00192-020-04540-w.
Coelho SCA, Marangoni-Junior M, Brito LGO, Castro EB, Juliato CRT. Quality of life and vaginal symptoms of postmenopausal women using pessary for pelvic organ prolapse: a prospective study. Rev Assoc Med Bras (1992). 2018;64(12):1103–7. https://doi.org/10.1590/1806-9282.64.12.1103.
Manchana T, Bunyavejchevin S. Impact on quality of life after ring pessary use for pelvic organ prolapse. Int Urogynecol J. 2012;23(7):873–7. https://doi.org/10.1007/s00192-011-1634-6.
Author information
Authors and Affiliations
Contributions
D. Niigaki and R.S.P. Silva contributed equally to the manuscript.
Conception and design: M.A.T. Bortolini, R.A. Castro; project development: D. Niigaki, M.A.T. Bortolini, R.A. Castro; data collection: D. Niigaki, R.A. Castro; data analysis and interpretation: D. Niigaki, R.A. Castro; manuscript writing: R.A. Castro, F.F. Fitz, R.S.P. Silva; manuscript editing: F.F. Fitz, M.A.T. Bortolini, R.A. Castro; supervision: R.A. Castro.
Corresponding author
Ethics declarations
Financial disclaimer/conflicts of interest
None.
Ethical approval
Human Research Ethics Committee of the Federal University of Sao Paulo (CAAE 09974412.7.0000.5505).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Niigaki, D.I., Silva, R.S.P., Bortolini, M.A.T. et al. Predictors for long-term adherence to vaginal pessary in pelvic organ prolapse: a prospective study. Int Urogynecol J 33, 3237–3246 (2022). https://doi.org/10.1007/s00192-022-05133-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05133-5