Abstract
Introduction and hypothesis
Deficient perineum is a disruption of the perineal body and distal rectovaginal septum presenting with anal incontinence and a range of urogenital symptoms. There is scarce reported outcome of this condition with management often delayed and with a variety of surgical alternatives. This study aims to determine faecal continence outcomes after long-term surgical repair.
Methods
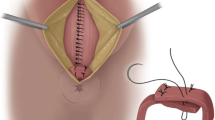
Patients were included for analysis after surgical repair between 1989 and 2012. Cases were preoperatively assessed by endosonography and anorectal manometry with a record of their continence with the Cleveland Clinic Incontinence Score (CCIS). Surgical repair comprised an overlapping repair of the external anal sphincter (EAS) with levatorplasty. There was selective use of internal anal sphincter (IAS) suture and/or advancement perineoplasty for soft tissue reconstruction. Patients were clinically evaluated for functional outcomes with comparison of their postoperative CCIS.
Results
There were 20 patients (median age 55.5 years; range 29–81 years) with a median duration of incontinence symptoms of 174 (range 1–540) months. All patients had an EAS and IAS defect with 14 (70%) undergoing an IAS suture and 10 (50%) a Corman-style anoplasty. Over a median follow-up of 137.2 (range 13–322) months, there was a significant decrease in the recorded median preoperative vs. postoperative CCIS 18, range 13–20 vs. 2, range 0–10, respectively; p < 0.001) with 18 (90%) satisfied with the functional outcome. Faecal diversion was not used in any of the patients.
Conclusions
Experienced delayed repair of a traumatic cloaca is associated with an acceptable functional outcome at medium- to long-term follow-up.




Similar content being viewed by others
References
Block IR, Rodriguez S, Olivares AL. The Warren operation for anal incontinence caused by disruption of the anterior segment of the anal sphincter, perineal body and rectovaginal septum: report of five cases. Dis Colon Rectum. 1975;18:28–34.
Abcarian H, Orsay CP, Pearl RK, Nelson RL, Briley SC. Traumatic cloaca. Dis Colon Rectum. 1989;32:783–7.
Goh J, Romanzi L, Elneil S, et al. An international continence society (ICS) report on the terminology for female pelvic floor fistulas. Neurourol Urodyn. 2020;39:2040–71.
Venkatesh KS, Ramanujam PS, Larson DM, Haywood MA. Anorectal complications of vaginal delivery. Dis Colon Rectum. 1989;32:1039–41.
Goh JTW, Tan SBM, Natukunda H, Singasi I, Krause HG. Outcomes following surgical repair using layered closure of unrepaired 4th degree perineal tear in rural western Uganda. Int Urogynecol J. 2016;27:1661–6.
Sultan AH, Kamm MA, Hudson CN, Bartram CI. Third degree obstetric anal sphincter tears: risk factors and outcome of primary repair. BMJ. 1994;308:887–91.
Lewicky-Gaupp C, Leader-Cramer A, Johnson LL, Kenton K, Gossett DR. Wound complications after obstetric anal sphincter injuries. Obstet Gynecol. 2015;125:1088–93.
Barbosa M, Glavind-Kristensen M, Christensen P. Early secondary repair of obstetric anal sphincter injury: postoperative complications, long-term functional outcomes and impact on quality of life. Tech Coloproctol. 2020;24:221–9.
Corman ML. Anal incontinence following obstetric injury. Dis Colon Rectum. 1985;28:86–9.
Kaiser AM. Cloaca-like deformity with faecal incontinence after severe obstetric injury – technique and functional outcome of ano-vaginal and perineal reconstruction with X-flaps and sphincteroplasty. Color Dis. 2008;10:827–32.
Zhou X, Chen W, Lin J, Xu J, Zheng S. Surgical repair of traumatic cloaca: a modified technique. Color Dis. 2019;21:1026–10.
Hollingshead JRF, Warusavitarne J, Vaizey CJ, Northover JMA. Outcomes following repair of traumatic claocal deformities. Br J Surg. 2009;96:1082–5.
Valente MA, Khanduja KS. Layered surgical repair of traumatic cloacal deformities: technical details and functional outcomes. Tech Coloproctol. 2012;16:153–6.
Maldonado PA, Mcintire D, Corton MM. Long-term outcomes after overlapping sphincteroplasty for cloacal-like deformities. Female Pelvic Med Reconstr Surg. 2019;25:271–8.
Venkatesh KS, Ramanujam P. Surgical treatment of traumatic cloaca. Dis Colon Rectum. 1996;39:811–6.
Ezer A, Parlakgumus A. Delayed reconstruction of a traumatic cloaca following obstetric anal sphincter rupture. J Coll Phys Surg Pak. 2017;27:S82–3.
Mercês RL, Pisi PH, Balestrim Fo A, Braga TA, Rocha JJR, Féres O. Surgical treatment of traumatic cloaca. Acta Cir Bras. 2008;23(Suppl 1):105–7.
Kaiser AM. Anovaginal reconstruction with bilateral X-flaps and sphincteroplasty for cloaca-like deformity after obstetrical injury. Dis Colon Rectum. 2007;50:1707.
Cardon A, Pattyn P, Monstrey S, Hesse U, de Hemptine B. Use of a unilateral pudendal thigh flap in the treatment of complex rectovaginal fistula. Br J Surg. 1999;86:645–6.
Picciariello A, Papagni V, Lambo M, Altomare DF. Surgical repair of traumatic cloacal deformity – a video vignette. Color Dis. 2019;21:611–2.
Hull TL, Bartus C, Bast J, et al. Success of episioproctotomy for cloaca and rectovaginal fistula. Dis Colon Rectum. 2007;50:97–101.
Jorge JM, Wexner SD. Etiology and management of fecal incontinence. Dis Colon Rectum. 1993;36:77–97.
Von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370:1453–7.
Barbosa M, Glavind-Kristensen M, Soerensen MM, Christensen P. Secondary sphincter repair for anal incontinence following obstetric sphincter injury: functional outcome and quality of life at 18 years of follow-up. Color Dis. 2019;22:71–9.
Stock L, Basham E, Gossett DR, Lewicky-Gaupp C. Factors associated with wound complications in women with obstetric anal sphincter injuries (OASIS). Am J Obstet Gynecol. 2013;208:327.e321–6.
Woodman PJ, Graney DO. Anatomy and physiology of the female perineal body with relevance to obstetrical injury and repair. Clin Anat. 2002;15:321–34.
Cichowski SB, Duniva GC, Rogers RG, et al. Patients’ experience compared with physicians’ recommendations for treating fecal incontinence: a qualitative approach. Int Urogynecol J. 2014;25:935–40.
Cerdán Santacruz C, Santos Rancaño R, Vigara García M, Fernández Pérez C, Ortega López M, Cerdán Miguel J. Prevalence of anal incontinence in a working population within a healthcare environment. Scand J Gastroenterol. 2017;52:1340–7.
Patel K, Bliss DZ, Savik K. Health literacy and emotional responses related to fecal incontinence. J Wound Ostomy Continence Nurs. 2010;37:73–9.
Evans C, Davis K y Kumar D (2006) Overlapping anal sphincter repair and anterior levatorplasty: effect of patient’s age and duration of follow-up. Int J Color Dis 21:795–801.
Grey BR, Sheldon RR, Telford KJ, Kiff ES. Anterior anal sphincter repair can be of long term benefit: a 12-year case cohort from a single surgeon. BMC Surg. 2007;11(7):1. https://doi.org/10.1186/1471-2482-7-1.
Malouf AJ, Norton CS, Engel AF, Nicholls RJ, Kamm MA. Long-term results of overlapping anterior anal-sphincter repair for obstetric trauma. Lancet. 2000;355(9200):260–5.
Zorcolo L, Covotta L, Bartolo DC. Outcome of anterior sphincter repair for obstetric injury: comparison of early and late results. Dis Colon Rectum. 2005;48:524–31.
Halverson AL, Hull TL. Long-term outcome of overlapping anal sphincter repair. Dis Colon Rectum. 2002;45:345–8.
Anaraki F, Etemad O. Sphincteroplasty and perineoplasty with skin advancement flap in management of traumatic cloacal defect. J Coloproctol (Rio J). 2017;37:18–24.
Hasegawa H, Yoshioka K, Keighley M. Randomized trial of fecal diversion for sphincter repair. Dis Colon Rectum. 2000;43:961–4.
Acknowledgements
We thank Prof. A.P. Zbar for his critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of the article do not have any commercial association that might pose a conflict of interest in relation to this article.
Ethics approval
The study protocol was approved by the Local Ethics Committee.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cerdán-Santacruz, C., Cano-Valderrama, Ó. & Cerdán-Miguel, J. Traumatic deficient perineum: surgical management and outcome from a single center. Int Urogynecol J 33, 651–658 (2022). https://doi.org/10.1007/s00192-021-04803-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04803-0