Abstract
Introduction and hypothesis
The objective was to determine the mean morphometric characteristics of the rectovaginal septum (RVS) and its variations in correlation with the number of pregnancies, method of delivery, parity, and estrogenic exposure.
Methods
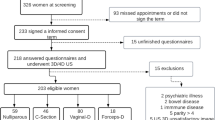
An observational, cross-sectional, retrospective, descriptive, and comparative study was carried out. Pelvic MRI of Hispanic women (≥15 years of age) from the northeast of Mexico were obtained. Age and obstetric and gynecological history were registered and the sample women were categorized by their variables. Length and thickness measurements were standardized.
Results
A total of 102 MRI studies were included, with a mean age of 41; 24.5% were nulligravida, the rest primi- or multigravida. Vaginal delivery was the most common type (49.35%), 16.88% had a cesarean section, and 31.17% had mixed delivery. 74.5% of the women were premenopausal. The mean RVS length was 73.2 ± 15.3 mm, with a thickness of 2.8 ± 1.7, 2.2 ± 1.2, and 2.5 ± 1.3 mm for the upper, middle, and lower thirds respectively. There were tendencies to increase the length of the RVS, and the thickness of the upper and middle thirds in the non-pregnancy and the at-least-one-pregnancy groups; to increase the length and middle-third thickness in those with mixed delivery, and increased upper- and lower-third thickness in those with only a cesarean section. Multiparous women with vaginal delivery had significantly longer and thicker RVS than primiparous. Premenopausal women had significantly longer RVS with a tendency to lose thickness toward postmenopause.
Conclusions
The morphology of RVS can be modified by different factors such as age, number of pregnancies, number of births, and estrogenic exposure. This structure should be evaluated and taken into account in preoperative management and surgical technique planning.

Similar content being viewed by others
References
Uhlenhuth E, Wolfe WM, Smith EM, Middleton EB. The rectogenital septum. Surg Gynecol Obstet. 1948;86(2):148–63.
Milley PS, Nichols DH. A correlative investigation of the human rectovaginal septum. Anat Rec. 1969;163(3):443–51. https://doi.org/10.1002/ar.1091630307.
Baggish MS, Karram MM (2015) Atlas of pelvic anatomy and gynecologic surgery. Amsterdam: Elsevier.
Rosenshein NB, Genadry RR, Woodruff JD. An anatomic classification of rectovaginal septal defects. Am J Obstet Gynecol. 1980;137(4):439–42. https://doi.org/10.1016/0002-9378(80)91124-2.
Aigner F, Zbar AP, Ludwikowski B, Kreczy A, Kovacs P, Fritsch H. The rectogenital septum: morphology, function, and clinical relevance. Dis Colon Rectum. 2004;47(2):131–40. https://doi.org/10.1007/s10350-003-0031-8.
Dietz HP. Can the rectovaginal septum be visualized by transvaginal three-dimensional ultrasound? Ultrasound Obstet Gynecol. 2011;37(3):348–52. https://doi.org/10.1002/uog.8896.
Dariane C, Moszkowicz D, Peschaud F. Concepts of the rectovaginal septum: implications for function and surgery. Int Urogynecol J. 2016;27(6):839–48. https://doi.org/10.1007/s00192-015-2878-3.
Nichols DH, Milley PS. Surgical significance of the rectovaginal septum. Am J Obstet Gynecol. 1970;108(2):215–20. https://doi.org/10.1016/0002-9378(70)90299-1.
Ludwikowski B, Hayward IO, Fritsch H. Rectovaginal fascia: an important structure in pelvic visceral surgery? About its development, structure, and function. J Pediatr Surg. 2002;37(4):634–8. https://doi.org/10.1053/jpsu.2002.31624.
Zhai LD, Liu J, Li YS, Yuan W, He L. Denonvilliers’ fascia in women and its relationship with the fascia propria of the rectum examined by successive slices of celloidin-embedded pelvic viscera. Dis Colon Rectum. 2009;52(9):1564–71. https://doi.org/10.1007/DCR.0b013e3181a8f75c.
Leffler KS, Thompson JR, Cundiff GW, Buller JL, Burrows LJ, Schön Ybarra MA. Attachment of the rectovaginal septum to the pelvic sidewall. Am J Obstet Gynecol. 2001;185(1):41–3. https://doi.org/10.1067/mob.2001.116366.
Baader B, Herrmann M. Topography of the pelvic autonomic nervous system and its potential impact on surgical intervention in the pelvis. Clin Anat. 2003;16(2):119–30. https://doi.org/10.1002/ca.10105.
Geynisman-Tan J, Kenton K. Surgical updates in the treatment of pelvic organ prolapse. Rambam Maimonides Med J. 2017;8(2):e0017. https://doi.org/10.5041/RMMJ.10294.
Kuhn RJ, Hollyock VE. Observations on the anatomy of the rectovaginal pouch and septum. Obstet Gynecol. 1982;59(4):445–7.
D’Hoore A, Vanbeckevoort D, Penninckx F. Clinical, physiological and radiological assessment of rectovaginal septum reinforcement with mesh for complex rectocele. Br J Surg. 2008;95(10):1264–72. https://doi.org/10.1002/bjs.6322.
Singh N. Development and anatomy: disorders of development. In: Brown L, editor. Pathology of the vulva and vagina. London: Springer. 2013.
Nagata I, Murakami G, Suzuki D, Furuya K, Koyama M, Ohtsuka A. Histological features of the rectovaginal septum in elderly women and a proposal for posterior vaginal defect repair. Int Urogynecol J. 2007;18(8):863–8. https://doi.org/10.1007/s00192-006-0249-9.
Shobeiri SA, White D, Quiroz LH, Nihira MA. Anterior and posterior compartment 3D endovaginal ultrasound anatomy based on direct histologic comparison. Int Urogynecol J. 2012;23(8):1047–53. https://doi.org/10.1007/s00192-012-1721-3.
Haylen BT, Naidoo S, Kerr SJ, Yong CH, Birrell W. Posterior vaginal compartment repairs: where are the main anatomical defects? Int Urogynecol J. 2016;27(5):741–5. https://doi.org/10.1007/s00192-015-2874-7.
Lopez C, Balogun M, Ganesan R, Olliff JF. MRI of vaginal conditions. Clin Radiol. 2005;60(6):648–62. https://doi.org/10.1016/j.crad.2005.02.010.
Paramasivam S, Proietto A, Puvaneswary M. Pelvic anatomy and MRI. Best Pract Res Clin Obstet Gynaecol. 2006;20(1):3–22. https://doi.org/10.1016/j.bpobgyn.2005.09.001.
Hsu Y, Lewicky-Gaupp C, DeLancey JO. Posterior compartment anatomy as seen in magnetic resonance imaging and 3-dimensional reconstruction from asymptomatic nulliparas. Am J Obstet Gynecol. 2008;198(6):651–e1. https://doi.org/10.1016/j.ajog.2007.11.032.
Wasnik AP, Mazza MB, Liu PS. Normal and variant pelvic anatomy on MRI. Magn Reson Imaging Clin N Am. 2011;19(3):547–66. https://doi.org/10.1016/j.mric.2011.05.001.
Salinas-Alvarez Y, Rodriguez-Abarca MA, Quiroga-Garza A, Guzman-Lopez S, Elizondo-Omaña RE, Jacobo-Baca G, et al. Rectovaginal septum and influencing factors in its morphology. FASEB J. 2020;34(S1):1–1. https://doi.org/10.1096/fasebj.2020.34.s1.06241.
Huebner M, Rall K, Brucker SY, Reisenauer C, Siegmann-Luz KC, DeLancey JO. The rectovaginal septum: visible on magnetic resonance images of women with Mayer-Rokitansky-Küster-Hauser syndrome (Müllerian agenesis). Int Urogynecol J. 2014;25(3):323–7. https://doi.org/10.1007/s00192-013-2214-8.
Vázquez-Barragán MÁ, Garza-Báez A, Morales-Avalos R, Martínez-González B, Jacobo-Baca G, Pinales-Razo R, et al. Pelvimetry by reformatted computed tomography in 290 female pelvis: morphometric variations regarding age. Int J Morphol. 2016;34(1):298–304. https://doi.org/10.4067/S0717-95022016000100043.
Acknowledgements
The authors thank Armando Franco for his help in the editing of the figure in this manuscript.
Funding
There was no external funding; resources were provided by the Department of Human Anatomy, UANL.
Author information
Authors and Affiliations
Contributions
M.A. Rodríguez-Abarca: methodology, data collection, validation, writing (review and editing); Edgar Guillermo Hernández-Grimaldo: methodology, data collection, validation, writing (review and editing); D. De la Fuente-Villarreal: methodology, validation, writing (review), supervision, project administration; G. Jacobo-Baca: conceptualization, methodology, validation, writing (review), supervision, project administration; A. Quiroga-Garza: conceptualization, methodology, data collection, validation, writing (review and editing), supervision, project administration; R. Pinales-Razo: methodology, writing (review), supervision, project administration; R.E. Elizondo-Omaña: methodology, writing (review and editing), supervision, project administration; S. Guzman-Lopez: methodology, writing (review), supervision, project administration.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rodríguez-Abarca, M.A., Hernández-Grimaldo, E.G., De la Fuente-Villarreal, D. et al. Gynecological influencing factors on the rectovaginal septum’s morphology. Int Urogynecol J 32, 1427–1432 (2021). https://doi.org/10.1007/s00192-020-04376-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-020-04376-4