Abstract
Introduction and hypothesis
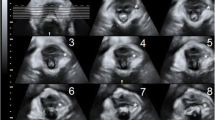
The objectives were to evaluate clinical and anatomical parameters assessed by three-dimensional pelvic floor ultrasound (3D ultrasound) in parous and nulliparous women of childbearing age and to assess underreported symptoms of sexual dysfunction (SD), urinary incontinence (UI) and flatus incontinence (FI).
Methods
Women without complaints of pelvic floor dysfunction, aged 20–50 years, were eligible for this prospective cross-sectional study. They completed the King’s Health Questionnaire, Female Sexual Function Index and St Mark’s Incontinence Score adapted for this study. Next, a physical examination and 3D ultrasound were performed. The scores obtained in the questionnaires were compared with the 3D ultrasound data.
Results
In total, 326 women were invited to participate. Of these, 203 women met the inclusion criteria, and their cases were classified as nulliparity (NU, 59), vaginal delivery (VD, 80), forceps delivery (FD, 18) and caesarean section (CS, 48). These groups were homogeneous regarding age (p=0.096), parity (p=0.051) and body mass index (p=0.06). The hiatal dimension (HD; p=0.003) and transverse diameter (TD) (p=0.001) were significantly different among the groups. Compared with the NU and CS groups, the VD and FD groups had an increased HD and TD. The frequencies of underreported symptoms identified by questionnaires were as follows: SD (46.3%), UI (35%) and FI (28%). After VD and FD, women were more likely to present UI (p<0.001), FI (p<0.001) and SD (p=0.002) than the women with NU and those who had undergone a CS. UI was related to a greater HD (p=0.002) and anteroposterior diameter (p=0.022), FI was associated with a thinner left pubovisceral muscle (p=0.013), and SD was related to a greater HD (p=0.026).
Conclusions
Three-dimensional ultrasound can identify mild morphological changes in young women with apparently normal physical examinations, mainly after VD and FD. In such individuals, these findings are associated with higher incidences of underreported sexual, urinary and anal symptoms.


Similar content being viewed by others
References
Corton MM. Anatomy of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 2009;36:401–19.
Rossetti SR. Functional anatomy of pelvic floor. Arch Ital Urol Androl. 2016;88:28–37.
Novo R, Perez-Rios M, Santiago-Pérez MI, Butler H, Malvar A, Hervada X. Prevalence and associated risk factors of urinary incontinence and dyspareunia during pregnancy and after delivery. Eur J Obstet Gynecol Reprod Biol. 2020;245:45–50. https://doi.org/10.1016/j.ejogrb.2019.10.020.
Larsson C, Hedberg CL, Lundgren E, Söderström L, TunÓn K, Nordin P. Anal incontinence after caesarean and vaginal delivery in Sweden: a national population-based study. Lancet. 2019;393(10177):1233–9.
Lipschuetz M, Cohen SM, Liebergall-Wischnitzer M, Zbedat K, Hochner-Celnikier D, Lavy Y, et al. Degree of bother from pelvic floor dysfunction in women one year after first delivery. Eur J Obstet Gynecol Reprod Biol. 2015;191:90–4.
Chamié LP, Ribeiro DMFR, Caiado AHM, Warmbrand G, Serafini PC. Translabial US and dynamic MR imaging of the pelvic floor: normal anatomy and dysfunction. Radiographics. 2018;38(1):287–308.
Dietz HP. Pelvic floor ultrasound. A review. Clin Obstet Gynecol. 2016;60(1):58–81. https://doi.org/10.1097/GRF.000000000000026.
Fonseca ESM, Camargo ALM, de Castro RA, MGF S, MCM F, de Lima GR, et al. Validação do questionário de qualidade de vida (King’s Health Questionnaire) em mulheres brasileiras com incontinência urinária. Rev Bras Ginecol Obstet. 2005;27(5):235–42.
Hebbar S, Pandey H, Chawla A. Understanding King’s Health Questionnaire (KHQ) in assessment of female urinary incontinence. Int J Res Med Sci. 2015;4(3):177–87.
Hentschel H, Alberton DL, Capp E, Goldim JR, Passos EP. Validação do female sexual function index (FSFI) para uso em língua portuguesa. Rev HCPA Porto Alegre. 2007;27(1):10–4.
Neijenhuijs KI, Hooghiemstra N, Holtmaat K, Aaronson NK, Groenvold M, Holzner B, et al. The Female Sexual Function Index (FSFI)—a systematic review of measurement properties. J Sex Med. 2019;16(5):640–60.
Dietz HP. Pelvic floor ultrasound. Curr Surg Rep. 2013;1(3):167–81.
Dietz HP, Shek C, Clarke B. Biometry of the pubovisceral muscle and levator hiatus by three-dimensional pelvic floor ultrasound. Ultrasound Obstet Gynecol. 2005;25(6):580–5.
Araujo Júnior E, de Freitas RCM, Di Bella ZIK, de Alexandre SMJ, Nakamura MU, Machado Nardozza LM, et al. Assessment of pelvic floor by three-dimensional-ultrasound in primiparous women according to delivery mode: initial experience from a single reference service in Brazil. Rev Bras Ginecol Obstet. 2013;35(3):117–22.
Moossdorff-Steinhauser HFA, Berghmans BCM, Spaanderman MEA, Bols EMJ. Prevalence, incidence and bothersomeness of urinary incontinence between 6 weeks and 1 year post-partum: a systematic review and meta-analysis. Int Urogynecol J. 2021;32:1675–93.
García-Mejido JA, Idoia-Valero I, Aguilar-Gálvez IM, Borrero González C, Fernández-Palacín A, Sainz JA. Association between sexual dysfunction and avulsion of the levator ani muscle after instrumental vaginal delivery. Acta Obstet Gynecol Scand. 2020;99(9):1246–52.
De Parades V, Etienney I, Thabut D, Beaulieu S, Tawk M, Assemekang B, et al. Anal sphincter injury after forceps delivery: myth or reality? A prospective ultrasound study of 93 females. Dis Colon Rectum. 2004;47(1):24–34.
Svare JA, Hansen BB, Lose G. Prevalence of anal incontinence during pregnancy and 1 year after delivery in a cohort of primiparous women and a control group of nulliparous women. Acta Obstet Gynecol Scand. 2016;95(8):920–5.
Speksnijder L, Oom DMJ, de Leeuw J-W, Steensma AB. Which factors are associated with anal incontinence after obstetric anal sphincter injury? Ultrasound Obstet Gynecol. 2021;58(3):476–82.
Webb SS, Sitch A, MacArthur C. The impact of mode of subsequent birth after obstetric anal sphincter injury on bowel function and related quality of life: a cohort study. Int Urogynecol J. 2020;31(11):2237–45.
Dumoulin C, Pazzoto Cacciari L, Mercier J. Keeping the pelvic floor healthy. Climacteric. 2019;22(3):257–262. https://doi.org/10.1080/13697137.2018.1552934.
Nyhus M, Oversand SH, Salvesen SK, Mathew S, Volløyhaug I. Ultrasound assessment of pelvic floor muscle contraction: reliability and development of an ultrasound-based contraction scale. Ultrasound Obstet Gynecol. 2020;55(1):125–31.
Gyhagen M, Bullarbo M, Nielsen TF, Milsom I. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120(2):152–60.
Nelson RL, Go C, Darwish R, Gao J, Parikh R, Kang C, et al. Cesarean delivery to prevent anal incontinence: a systematic review and meta-analysis. Tech Coloproctol. 2019;23(9):809–20.
Gommesen D, Nohr EA, Qvist N, Rasch V. Obstetric perineal ruptures—risk of anal incontinence among primiparous women 12 months postpartum: a prospective cohort study. Am J Obstet Gynecol. 2020;222(2):165.e1–11. https://doi.org/10.1016/j.ajog.2019.08.026.
Hicks TL, Forester Goodall S, Quattrone EM, Lydon-Rochelle MT. Postpartum sexual functioning and method of delivery: summary of the evidence. J Midwifery Womens Health. 2004;49(5):430–6.
Rathfisch G, Dikencik BK, Kizilkaya Beji N, Comert N, Tekirdag AI, Kadioglu A. Effects of perineal trauma on postpartum sexual function. J Adv Nurs. 2010;66(12):2640–9.
Hipp LE, Kane Low L, Van Anders SM. Exploring women’s postpartum sexuality: social, psychological, relational, and birth-related contextual factors. J Sex Med. 2012;9(9):2330–41.
Jármy-Di Bella ZIK, Araujo Júnior E, Rodrigues CA, Torelli L, Martins WP, Moron AF, et al. Reproducibility in pelvic floor biometric parameters of nulliparous women assessed by translabial three-dimensional ultrasound using Omniview reformatting technique. Med Ultrason. 2016;18(3):345–50.
Abdool Z, Dietz HP, Lindeque BG. Ethnic differences in the levator hiatus and pelvic organ descent: a prospective observational study. Ultrasound Obstet Gynecol. 2017;50(2):242–6.
Ramalingam K, Monga A. Obesity and pelvic floor dysfunction. Best Pract Res Clin Obstet Gynaecol. 2015;29(4):541–7.
Author information
Authors and Affiliations
Contributions
Grinbaum, M.L. – Project development, Data collection, Manuscript writing
Bianchi-Ferraro, AMHM – Project development, Manuscript writing
Rodrigues, CA – Data collection
Sartori, MGF – Project development
Jármy-Di Bella, ZKI – Project development, Manuscript writing
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Grinbaum, M.L., Bianchi-Ferraro, A.M.H.M., Rodrigues, C.A. et al. Impact of parity and delivery mode on pelvic floor function in young women: a 3D ultrasound evaluation. Int Urogynecol J 34, 1849–1858 (2023). https://doi.org/10.1007/s00192-022-05440-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05440-x