Abstract
Introduction and hypothesis
Pelvic organ prolapse (POP) is a common medical condition universally. In addition to physical examination, experts have increasingly turned their attention to ultrasound in diagnosing POP for its low cost and dynamic imaging. The aim of this paper is to provide an overview of the methods of pelvic floor ultrasound in diagnosing POP, which has been lacking up till now.
Methods
We included original papers comparing the outcome of the Pelvic Organ Prolapse Quantification system and ultrasound, published from 2008 to present in English, using electronic databases (MEDLINE, EMBASE, CENTRAL, PUBMED). All stages of the review were conducted in parallel by two reviewers.
Results
Fifteen papers were included. We found that current methods have advantages and limitations. The main methods are to measure levator hiatus-related parameters and distances between the lowest point of the pelvic organs and reference lines during Valsalva maneuver, contraction, and at rest.
Conclusions
Pelvic floor ultrasound is valuable in diagnosing POP, yet suffers from a weakness in precision compared with physical examination. From the existing research, we found that the differences in baseline data such as weight, height, ethnicity, etc., may affect the cutoffs of the above-mentioned parameters. Further research is required to find one appropriate cutoff for each parameter, even if it is necessary to set group values for every parameter according to varying situations.








Similar content being viewed by others
References
Haylen BT, Maher CF, Barber MD, Camargo S, Dandolu V, Digesu A, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic organ prolapse (POP). Int Urogynecol J. 2016;27(4):655–84. https://doi.org/10.1007/s00192-016-3003-y.
Cooper J, Annappa M, Dracocardos D, Cooper W, Muller S, Mallen C. Prevalence of genital prolapse symptoms in primary care: a cross-sectional survey. Int Urogynecol J. 2015;26(4):505–10. https://doi.org/10.1007/s00192-014-2556-x.
Smith FJ, Holman CD, Moorin RE, Tsokos N. Lifetime risk of undergoing surgery for pelvic organ prolapse. Obstet Gynecol. 2010;116(5):1096–100. https://doi.org/10.1097/AOG.0b013e3181f73729.
Wu JM, Vaughan CP, Goode PS, Redden DT, Burgio KL, Richter HE, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8. https://doi.org/10.1097/aog.0000000000000057.
Yuk JS, Lee JH, Hur JY, Shin JH. The prevalence and treatment pattern of clinically diagnosed pelvic organ prolapse: a Korean National Health Insurance Database-based cross-sectional study 2009-2015. Sci Rep. 2018;8(1):1334. https://doi.org/10.1038/s41598-018-19692-5.
Wilkins MF, Wu JM. Lifetime risk of surgery for stress urinary incontinence or pelvic organ prolapse. Minerva Ginecol. 2017;69(2):171–7. https://doi.org/10.23736/s0026-4784.16.04011-9.
Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in U.S. Women: 2010 to 2050. Obstet Gynecol. 2009;114(6):1278–83. https://doi.org/10.1097/AOG.0b013e3181c2ce96.
Barber MD. Symptoms and outcome measures of pelvic organ prolapse. Clin Obstet Gynecol. 2005;48(3):648–61.
Barber MD. Pelvic organ prolapse. BMJ. 2016;354:i3853. https://doi.org/10.1136/bmj.i3853.
Manonai J, Wattanayingcharoenchai R. Relationship between pelvic floor symptoms and POP-Q measurements. Neurourol Urodyn. 2016;35(6):724–7. https://doi.org/10.1002/nau.22786.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Madhu C, Swift S, Moloney-Geany S, Drake MJ. How to use the pelvic organ prolapse quantification (POP-Q) system? Neurourol Urodyn. 2018;37(S6):S39–s43. https://doi.org/10.1002/nau.23740.
Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P. Pelvic organ prolapse quantification system (POP-Q)—a new era in pelvic prolapse staging. J Med Life. 2011;4(1):75–81.
Pham T, Burgart A, Kenton K, Mueller ER, Brubaker L. Current use of pelvic organ prolapse quantification by AUGS and ICS members. Female Pelvic Med Reconstr Surg. 2011;17(2):67–9. https://doi.org/10.1097/SPV.0b013e318207c904.
Wiegersma M, Panman CM, Kollen BJ, Berger MY, Lisman-van Leeuwen Y, Dekker JH. Is the hymen a suitable cut-off point for clinically relevant pelvic organ prolapse? Maturitas. 2017;99:86–91. https://doi.org/10.1016/j.maturitas.2017.02.012.
Dietz HP, Mann KP. What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J. 2014;25(4):451–5. https://doi.org/10.1007/s00192-013-2307-4.
Dietz HP, Haylen BT, Broome J. Ultrasound in the quantification of female pelvic organ prolapse. Ultrasound Obstet Gynecol. 2001;18(5):511–4. https://doi.org/10.1046/j.0960-7692.2001.00494.x.
Iglesia CB, Smithling KR. Pelvic organ prolapse. Am Fam Physician. 2017;96(3):179–85.
Nyhus MO, Salvesen KA, Volloyhaug I. Association between pelvic floor muscle trauma and contraction in parous women from a general population—a cross sectional study. Ultrasound Obstet Gynecol. 2019;53(2):262–8. https://doi.org/10.1002/uog.19195.
Delancey JO, Hurd WW. Size of the urogenital hiatus in the levator ani muscles in normal women and women with pelvic organ prolapse. Obstet Gynecol. 1998;91(3):364–8.
Majida M, Braekken I, Bo K, Benth J, Engh M. Anterior but not posterior compartment prolapse is associated with levator hiatus area: a three- and four-dimensional transperineal ultrasound study. BJOG. 2011;118(3):329–37. https://doi.org/10.1111/j.1471-0528.2010.02784.x.
Ying T, Li Q, Xu L, Liu F, Hu B. Three-dimensional ultrasound appearance of pelvic floor in nulliparous women and pelvic organ prolapse women. Int J Med Sci. 2012;9(10):894–900. https://doi.org/10.7150/ijms.4829.
Wen L, Zhou Q. Can we evaluate hiatal ballooning by measuring the anteroposterior diameter with 2-dimensional translabial ultrasonography? J Ultrasound Med. 2018;37(4):1001–6. https://doi.org/10.1002/jum.14445.
Albrich SB, Welker K, Wolpert B, Steetskamp J, Porta S, Hasenburg A, et al. How common is ballooning? Hiatal area on 3D transperineal ultrasound in urogynecological patients and its association with lower urinary tract symptoms. Arch Gynecol Obstet. 2017;295(1):103–9. https://doi.org/10.1007/s00404-016-4200-0.
Dou C, Li Q, Ying T, Yan Y, Wang X, Hu B. Determining “abnormal” levator hiatus distensibility using three-dimensional transperineal ultrasound in Chinese women. Front Med. 2018;12(5):572–9. https://doi.org/10.1007/s11684-017-0561-4.
Wen L, Zhang J, Zeng S, Zhou Q. Using Z-scores to evaluate levator hiatal dimensions with four-dimensional translabial ultrasound. J Obstet Gynaecol Res. 2017;43(12):1840–7. https://doi.org/10.1111/jog.13454.
Wen L, Liu M, Zhao B, Qing Z. Evaluating Z scores to quantify levator hiatal distensibility by 3-dimensional ultrasonography in nulliparas and women with pelvic organ prolapse. J Ultrasound Med. 2018;37(10):2363–9. https://doi.org/10.1002/jum.14590.
Lakeman MM, Zijta FM, Peringa J, Nederveen AJ, Stoker J, Roovers JP. Dynamic magnetic resonance imaging to quantify pelvic organ prolapse: reliability of assessment and correlation with clinical findings and pelvic floor symptoms. Int Urogynecol J. 2012;23(11):1547–54. https://doi.org/10.1007/s00192-012-1772-5.
Volloyhaug I, Rojas RG, Morkved S, Salvesen KA. Comparison of transperineal ultrasound with POP-Q for assessing symptoms of prolapse. Int Urogynecol J. 2019;30(4):595–602. https://doi.org/10.1007/s00192-018-3722-3.
Dietz HP, Kamisan Atan I, Salita A. Association between ICS POP-Q coordinates and translabial ultrasound findings: implications for definition of ‘normal pelvic organ support’. Ultrasound Obstet Gynecol. 2016;47(3):363–8. https://doi.org/10.1002/uog.14872.
Lone F, Sultan AH, Stankiewicz A, Thakar R. The value of pre-operative multicompartment pelvic floor ultrasonography: a 1-year prospective study. Br J Radiol. 2014;87(1040):20140145. https://doi.org/10.1259/bjr.20140145.
Najjari L, Hennemann J, Larscheid P, Papathemelis T, Maass N. Perineal ultrasound as a complement to POP-Q in the assessment of cystoceles. Biomed Res Int. 2014;2014:740925. https://doi.org/10.1155/2014/740925.
Arian A, Ghanbari Z, Chegini N, Hosseiny M. Agreement of ultrasound measures with POP-Q in patients with pelvic organ prolapse. Iran J Radiol. 2018;15(4):6. https://doi.org/10.5812/iranjradiol.68461.
Lone FW, Thakar R, Sultan AH, Stankiewicz A. Accuracy of assessing pelvic organ prolapse quantification points using dynamic 2D transperineal ultrasound in women with pelvic organ prolapse. Int Urogynecol J. 2012;23(11):1555–60. https://doi.org/10.1007/s00192-012-1779-y.
Broekhuis SR, Kluivers KB, Hendriks JC, Futterer JJ, Barentsz JO, Vierhout ME. POP-Q, dynamic MR imaging, and perineal ultrasonography: do they agree in the quantification of female pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(5):541–9. https://doi.org/10.1007/s00192-009-0821-1.
Bray R, Derpapas A, Fernando R, Khullar V, Panayi DC. Does the vaginal wall become thinner as prolapse grade increases? Int Urogynecol J. 2017;28(3):397–402. https://doi.org/10.1007/s00192-016-3150-1.
Wen L, Li Y, Qing Z, Liu M. Detection of concealed uterine prolapse in the volume-rendering mode of 4-dimensional translabial ultrasound: a retrospective observational study. J Ultrasound Med. 2019;38(7):1705–11. https://doi.org/10.1002/jum.14855.
Dietz HP. Clinical consequences of levator trauma. Ultrasound Obstet Gynecol. 2012;39(4):367–71. https://doi.org/10.1002/uog.11141.
Dietz HP, Franco AV, Shek KL, Kirby A. Avulsion injury and levator hiatal ballooning: two independent risk factors for prolapse? An observational study. Acta Obstet Gynecol Scand. 2012;91(2):211–4. https://doi.org/10.1111/j.1600-0412.2011.01315.x.
Rostaminia G, Peck JD, Quiroz LH, Shobeiri SA. Characteristics associated with pelvic organ prolapse in women with significant levator ani muscle deficiency. Int Urogynecol J. 2016;27(2):261–7. https://doi.org/10.1007/s00192-015-2827-1.
Vergeldt TF, Notten KJ, Weemhoff M, van Kuijk SM, Mulder FE, Beets-Tan RG, et al. Levator hiatal area as a risk factor for cystocele recurrence after surgery: a prospective study. BJOG. 2015;122(8):1130–7. https://doi.org/10.1111/1471-0528.13340.
Holland EL, Cran GW, Elwood JH, Pinkerton JH, Thompson W. Associations between pelvic anatomy, height and year of birth of men and women in Belfast. Ann Hum Biol. 1982;9(2):113–20.
Munabi IG, Mirembe F, Luboga IG. Human pelvis height is associated with other pelvis measurements of obstetric value. Anat J Afr. 2015;4(1):457–65.
Munabi IG, Byamugisha J, Luboobi L, Luboga SA, Mirembe F. Relationship between maternal pelvis height and other anthropometric measurements in a multisite cohort of Ugandan mothers. Pan Afr Med J. 2016;24:257. https://doi.org/10.11604/pamj.2016.24.257.9889.
Zhu YC, Deng SH, Jiang Q, Zhang Y. Correlation between delivery mode and pelvic organ prolapse evaluated by four-dimensional pelvic floor ultrasonography. Med Sci Monit. 2018;24:7891–7. https://doi.org/10.12659/msm.911343.
Dietz HP, Scoti F, Subramaniam N, Friedman T, Shek KL. Impact of subsequent pregnancies on pelvic floor functional anatomy. Int Urogynecol J. 2018;29(10):1517–22.
Mouritsen L, Larsen JP. Symptoms, bother and POPQ in women referred with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2003;14(2):122–7. https://doi.org/10.1007/s00192-002-1024-1.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7; discussion 1337-1338. https://doi.org/10.1067/mob.2001.119078.
Panman C, Wiegersma M, Kollen BJ, Berger MY, Lisman-Van Leeuwen Y, Vermeulen KM, et al. Two-year effects and cost-effectiveness of pelvic floor muscle training in mild pelvic organ prolapse: a randomised controlled trial in primary care. BJOG. 2017;124(3):511–20. https://doi.org/10.1111/1471-0528.13992.
Rodriguez-Mias NL, Subramaniam N, Friedman T, Shek KL, Dietz HP. Prolapse assessment supine and standing: do we need different cutoffs for “significant prolapse”? Int Urogynecol J. 2018;29(5):685–9. https://doi.org/10.1007/s00192-017-3342-3.
Braverman M, Kamisan Atan I, Turel F, Friedman T, Dietz HP. Does patient posture affect the ultrasound evaluation of pelvic organ prolapse? J Ultrasound Med. 2019;38(1):233–8. https://doi.org/10.1002/jum.14688.
Dietz HP, Rojas RG, Shek KL. Postprocessing of pelvic floor ultrasound data: how repeatable is it? Aust N Z J Obstet Gynaecol. 2014;54(6):553–7. https://doi.org/10.1111/ajo.12250.
Majida M, Braekken IH, Umek W, Bo K, Saltyte Benth J, Ellstrom Engh M. Interobserver repeatability of three- and four-dimensional transperineal ultrasound assessment of pelvic floor muscle anatomy and function. Ultrasound Obstet Gynecol. 2009;33(5):567–73. https://doi.org/10.1002/uog.6351.
Tan L, Shek KL, Atan IK, Rojas RG, Dietz HP. The repeatability of sonographic measures of functional pelvic floor anatomy. Int Urogynecol J. 2015;26(11):1667–72. https://doi.org/10.1007/s00192-015-2759-9.
Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017;217(1):11–26.e13. https://doi.org/10.1016/j.ajog.2017.01.039.
Abdool Z, Dietz HP, Lindeque BG. Ethnic differences in the levator hiatus and pelvic organ descent: a prospective observational study. Ultrasound Obstet Gynecol. 2017;50(2):242–6. https://doi.org/10.1002/uog.17297.
Abdool Z, Dietz HP, Lindeque BG. Interethnic variation in pelvic floor morphology in women with symptomatic pelvic organ prolapse. Int Urogynecol J. 2018;29(5):745–50. https://doi.org/10.1007/s00192-017-3391-7.
Derpapas A, Ahmed S, Vijaya G, Digesu GA, Regan L, Fernando R, et al. Racial differences in female urethral morphology and levator hiatal dimensions: an ultrasound study. Neurourol Urodyn. 2012;31(4):502–7. https://doi.org/10.1002/nau.21181.
Onwude JL. Genital prolapse in women. BMJ Clin Evid. 2012;3:817
Acknowledgements
Foundation of Sichuan Provincial Science and Technology Program (Grant No. 2019YFH0147), Foundation of Chengdu Municipal Science and Technology Program (Grant No. 2018YF0500195SN) and Foundation of West China Second Hospital Program (Grant No. KX111) are acknowledged.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Financial disclaimers
The authors acknowledge the following financial support: Foundation of Sichuan Provincial Science and Technology Program (Grant No. 2019YFH0147); Foundation of Chengdu Municipal Science and Technology Program (Grant No. 2018YF0500195SN); Foundation of West China Second Hospital Program (Grant No. KX111).
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendices
Appendix 1
Appendix 2
Appendix 3
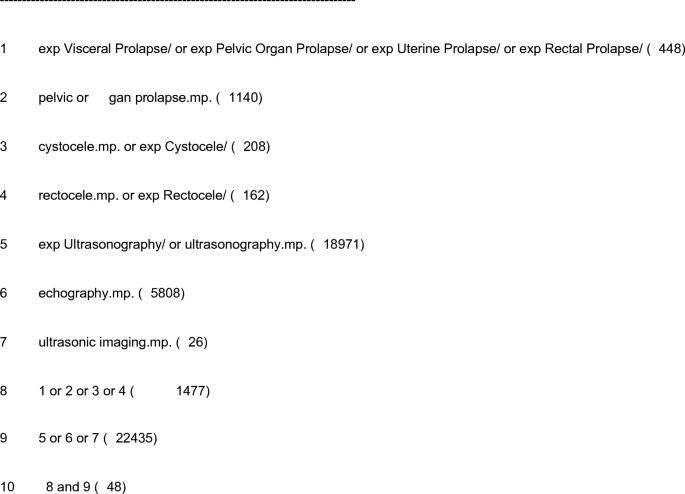
Appendix 4: search strategy
-
a)
Database: EBM Reviews—Cochrane Central Register of Controlled Trials, May 2019
Search strategy:
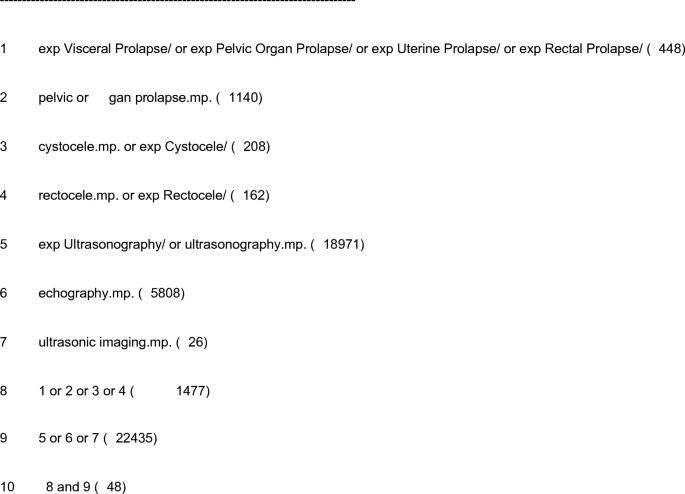
-
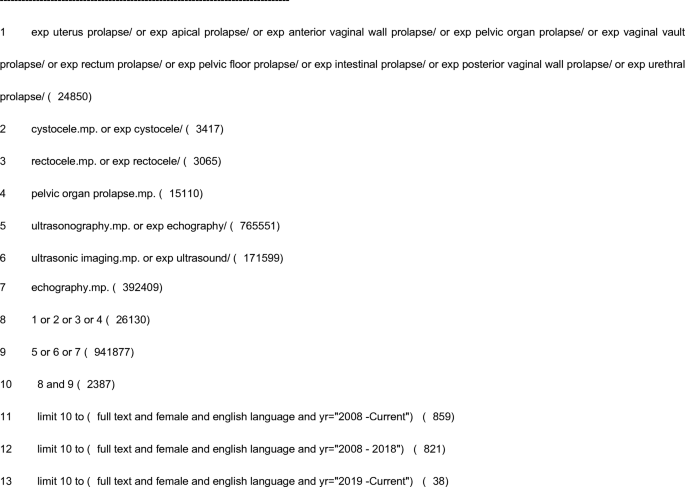
b)
Database: Embase, 1974 to 13 June 2019
Search strategy:
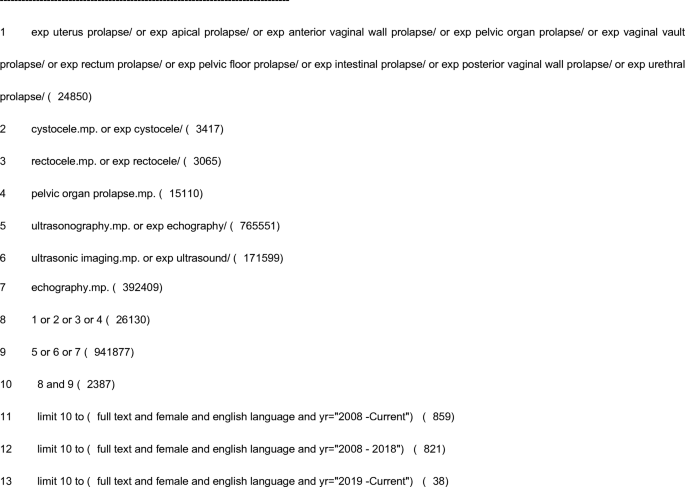
-
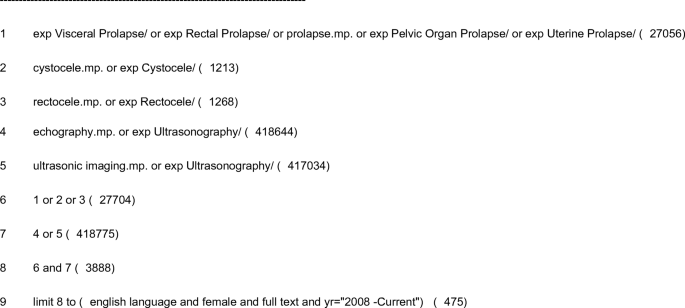
c)
Database: Ovid MEDLINE, 1946 to June week 2 2019
Search strategy:
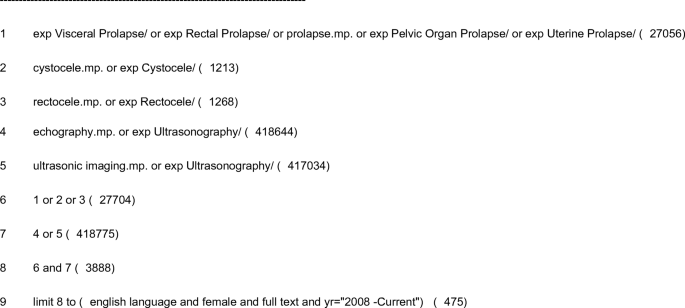
-
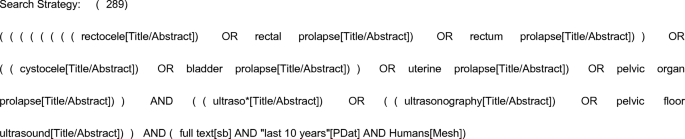
d)
Database: PubMed, 1946 to 14 June 2019
Search strategy:
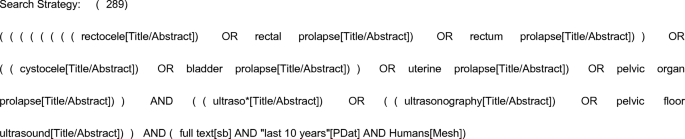
Appendix 5
Rights and permissions
About this article
Cite this article
Gao, Y., Zhao, Z., Yang, Y. et al. Diagnostic value of pelvic floor ultrasonography for diagnosis of pelvic organ prolapse: a systematic review. Int Urogynecol J 31, 15–33 (2020). https://doi.org/10.1007/s00192-019-04066-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-04066-w