Abstract
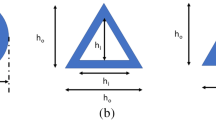
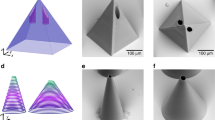
Hollow microneedles (HMNs) are minimally invasive needle-like microfeatures usually arranged in arrays designed for drug delivery and body fluid collection in a painless manner. In a recent work, we demonstrated a novel methodology to mass produce hollow polymer microneedles at a low cost. This methodology combines ultrashort pulse laser ablation to create inverse needle shapes in moulds and replication through polymer injection moulding. For a HMN to be functional, it should effectively pierce the skin at a low force and enable fluidic passage through the skin without leakage. This study investigates the impact of different laser scanning strategies on the cavity morphology and analyses how the various geometrical characteristics of the needle influence the penetration efficacy. To assess the penetration behaviour of the replicated HMNs, a combination of agarose gel and Parafilm® is employed as an in vitro testing platform. Furthermore, a correlation between HMN geometry, penetration performance, and modification of polymer material and holding pressure during injection moulding is established. The results indicate that a certain needle length is essential for effective penetration. Moreover, minimising the tip area, a factor significantly affecting penetration force, can be achieved by increasing the eccentricity of the scan-free area and expanding the scanning diameter. However, it is important to consider other functional needle features such as the ridge height or full lumen, which come at a cost to the tip sharpness. This work highlights the multiple interactions between the scanning strategy, the injection moulding process parameters, the needle geometry, and the penetration force. This study provides insights into optimization of the HMN design and the fabrication for enhanced penetration efficacy of functional injection-moulded polymeric HMNs.
























Similar content being viewed by others
References
Menon I, Bagwe P, Gomes KB et al (2021) Microneedles: a new generation vaccine delivery system. Micromachines 12:4. https://doi.org/10.3390/MI12040435
Miller PR, Taylor RM, Tran BQ et al (2018) Extraction and biomolecular analysis of dermal interstitial fluid collected with hollow microneedles. Commun Biol 1:173. https://doi.org/10.1038/s42003-018-0170-z
Meng F, Hasan A, Mahdi Nejadi Babadaei M et al (2020) Polymeric-based microneedle arrays as potential platforms in the development of drugs delivery systems. J Adv Res 26:137–147. https://doi.org/10.1016/j.jare.2020.07.017
Li Y, Zhang H, Yang R et al (2019) Fabrication of sharp silicon hollow microneedles by deep-reactive ion etching towards minimally invasive diagnostics. Microsyst Nanoeng 5:1–11. https://doi.org/10.1038/s41378-019-0077-y
Van Hileghem L, Kushwaha S, Piovesan A et al (2023) Innovative fabrication of hollow microneedle arrays enabling blood sampling with a self-powered microfluidic patch. Micromachines 14:615. https://doi.org/10.3390/MI14030615/S1
Bystrova S, Luttge R (2011) Micromolding for ceramic microneedle arrays. Microelectron Eng 88:1681–1684. https://doi.org/10.1016/J.MEE.2010.12.067
Evens T, Van Hileghem L, Dal Dosso F et al (2021) Producing hollow polymer microneedles using laser ablated molds in an injection molding process. J Micro Nanomanuf 9:1–9. https://doi.org/10.1115/1.4051456
Makvandi P, Kirkby M, Hutton ARJ et al (2021) Engineering microneedle patches for improved penetration: analysis, skin models and factors affecting needle insertion. Nanomicro Lett 13:93. https://doi.org/10.1007/S40820-021-00611-9
Permana AD, Mir M, Utomo E, Donnelly RF (2020) Bacterially sensitive nanoparticle-based dissolving microneedles of doxycycline for enhanced treatment of bacterial biofilm skin infection: a proof of concept study. Int J Pharm X 2:100047. https://doi.org/10.1016/J.IJPX.2020.100047
Permana AD, Paredes AJ, Volpe-Zanutto F et al (2020) Dissolving microneedle-mediated dermal delivery of itraconazole nanocrystals for improved treatment of cutaneous candidiasis. Eur J Pharm Biopharm 154:50–61. https://doi.org/10.1016/J.EJPB.2020.06.025
Koelmans WW, Krishnamoorthy G, Heskamp A et al (2013) Microneedle characterization using a double-layer skin simulant. Mech Eng Res 3:51. https://doi.org/10.5539/MER.V3N2P51
Wang QL, Zhu DD, Chen Y, Guo D (2016) A fabrication method of microneedle molds with controlled microstructures. Mater Sci Eng C 65:135–142. https://doi.org/10.1016/j.msec.2016.03.097
Singh Kochhar J, Quek TC, Soon WJ et al (2013) Effect of microneedle geometry and supporting substrate on microneedle array penetration into skin. J Pharm Sci 102:4100–4108. https://doi.org/10.1002/jps.23724
Flaten GE, Palac Z, Engesland A et al (2015) In vitro skin models as a tool in optimization of drug formulation. Eur J Pharm Sci 75:10–24. https://doi.org/10.1016/J.EJPS.2015.02.018
Yadav PR, Han T, Olatunji O et al (2020) Mathematical modelling, simulation and optimisation of microneedles for transdermal drug delivery: trends and progress. Pharmaceutics 12:1–31. https://doi.org/10.3390/PHARMACEUTICS12080693
Han J, Malek O, Vleugels J et al (2022) Ultrashort pulsed laser ablation of zirconia-alumina composites for implant applications. J Mater Process Technol 299:117335. https://doi.org/10.1016/J.JMATPROTEC.2021.117335
Evens T, Castagne S, Seveno D, Van Bael A (2022) Comparing the replication fidelity of solid microneedles using injection compression moulding and conventional injection moulding. Micromachines 13:1280. https://doi.org/10.3390/MI13081280
Larrañeta E, Moore J, Vicente-Pérez EM et al (2014) A proposed model membrane and test method for microneedle insertion studies. Int J Pharm 472:65–73. https://doi.org/10.1016/j.ijpharm.2014.05.042
Præstmark KA, Jensen ML, Madsen NB et al (2016) Pen needle design influences ease of insertion, pain, and skin trauma in subjects with type 2 diabetes. BMJ Open Diabetes Res Care 4:e000266. https://doi.org/10.1136/bmjdrc-2016-000266
Evens T, Malek O, Castagne S et al (2021) Controlling the geometry of laser ablated microneedle cavities in different mould materials and assessing the replication fidelity within polymer injection moulding. J Manuf Process 62:535–545. https://doi.org/10.1016/j.jmapro.2020.12.035
Penchev P, Dimov S, Bhaduri D et al (2017) Generic software tool for counteracting the dynamics effects of optical beam delivery systems. Proc Inst Mech Eng, Part B 231:48–64. https://doi.org/10.1177/0954405414565379
Evens T, Castagne S, Seveno D, Van Bael A (2022) Predicting the replication fidelity of injection molded solid polymer microneedles. Int Polym Process 37:237–254. https://doi.org/10.1515/ipp-2021-4207
Khanna P, Luongo K, Strom JA, Bhansali S (2010) Sharpening of hollow silicon microneedles to reduce skin penetration force. J Micromech Microeng 20:4. https://doi.org/10.1088/0960-1317/20/4/045011
Kong XQ, Zhou P, Wu CW (2011) Numerical simulation of microneedles’ insertion into skin. Comput Methods Biomech Biomed Engin 14:827–835. https://doi.org/10.1080/10255842.2010.497144
Kim YC, Park JH, Prausnitz MR (2012) Microneedles for drug and vaccine delivery. Adv Drug Deliv Rev 64:1547. https://doi.org/10.1016/J.ADDR.2012.04.005
Tuan-Mahmood T-M, McCrudden MTC, Torrisi BM et al (2013) Microneedles for intradermal and transdermal drug delivery. Eur J Pharm Sci 50:623–637. https://doi.org/10.1016/j.ejps.2013.05.005
Xiu X, Gao G, Liu Y, Ma F (2022) Drug delivery with dissolving microneedles: skin puncture, its influencing factors and improvement strategies. J Drug Deliv Sci Technol 76:103653. https://doi.org/10.1016/j.jddst.2022.103653
Shu W, Heimark H, Bertollo N et al (2021) Insights into the mechanics of solid conical microneedle array insertion into skin using the finite element method. Acta Biomater 135:403–413. https://doi.org/10.1016/J.ACTBIO.2021.08.045
Acknowledgements
The authors would like to thank Olivier Malek from Sirris (department of Precision Manufacturing) for the laser ablation of the microneedle cavities. The KU Leuven XCT Core facility is acknowledged for the 3D image acquisition and quantitative post-processing tools (https://xct.kuleuven.be/).
Funding
This work was funded by the KU Leuven Interdisciplinary Network project IDN/20/011 MIRACLE: Autonomous microfluidic patch for plasmid-based vaccine, as well as the Fonds Wetenschappelijk Onderzoek (FWO)–Vlaanderen SBO project S003923N and SB fellowship 1S31022N. The FWO large infrastructure I013518N project is acknowledged for their financial support of the X-ray infrastructure.
Author information
Authors and Affiliations
Contributions
Conceptualization, methodology, and investigation were performed by Pol Vanwersch and Tim Evens. The first draft of the manuscript was written by Pol Vanwersch and all authors commented on previous versions of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Vanwersch, P., Evens, T., Van Bael, A. et al. Design, fabrication, and penetration assessment of polymeric hollow microneedles with different geometries. Int J Adv Manuf Technol 132, 533–551 (2024). https://doi.org/10.1007/s00170-024-13344-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00170-024-13344-x