Abstract
Purpose
Minced cartilage is a one-step, autologous procedure with promising short-term results. The aim of the present study was to evaluate mid-term results in a patient cohort with chondral and osteochondral lesions in the knee joint treated with minced cartilage.
Methods
From 2015 through 2016, a total of 34 consecutive patients were treated with a single-step, autologous minced cartilage for knee chondral and osteochondral lesions. Numeric analogue scale (NAS) for pain and knee function were obtained prior to surgery and at 12, 24 and 60 months postoperatively. Secondary outcomes, including Lysholm score, Tegner activity score, and the International Knee Documentation Committee (IKDC) score, were recorded at final follow-up. MRI examinations of patients with unplanned radiological follow-up were analysed using the MOCART (Magnetic Resonance Observation of Cartilage Repair Tissue) score.
Results
A total of 28 patients (44.1% females, age at surgery: 29.5 ± 11.5 years) were available at a mean follow-up of 65.5 ± 4.1 months. Mean defect size was 3.5 ± 1.8 cm2. NAS for pain decreased from a median of 7 (range: 2–10) preoperatively to 2 (0–8) postoperatively. NAS knee function improved from a median of 7 (range: 2–10) to 3 (0–7) after five years, respectively. Satisfactory Lysholm (76.5 ± 12.5), IKDC (71.6 ± 14.8) and Tegner activity (4, range 3–9) scores were reported at final follow-up. Of all patients, 21(75%) and 19 (67.9%) reached or exceeded the PASS for the IKDC- and Lysholm score at final follow-up, respectively. The average overall MOCART 2.0 scores for all postoperatively performed MRIs (n = 23) was 62.3 ± 17.4. Four (14.2%) postoperative complications were directly linked to minced cartilage, one (3.5%) of which required revision surgery.
Conclusion
One-step, autologous minced cartilage repair of chondral and osteochondral lesions of the knee without the necessity for subchondral bone treatment demonstrated good patient-reported outcomes, low complication rates, and graft longevity at mid-term follow-up. Minced cartilage represents a viable treatment option to more traditional cartilage repair techniques even in mid-term.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of chondral and osteochondral lesions of the knee is increasing, but treatment remains challenging [13, 52]. Several different cartilage repair techniques have been described, each one aiming to maximize the amount of mature and organized hyaline or hyaline-like cartilage [7, 19]. However, so far, no technique has been able to regenerate normal hyaline cartilage in adults on a regularly basis and no technique has been proven to be superior. Osteochondral autograft transfer system (OATS), autologous chondrocyte implantation (ACI), matrix-assisted chondrocyte implantation (MACI) or several cartilage repair techniques using scaffolds (natural or synthetic) are contemporarily the most commonly therapies for medium to large defects [7, 22]. ACI and MACI are purported to generate hyaline or hyaline-like cartilage, with low associated reoperation rates and favourable clinical outcomes even in complex cases [5, 7, 18, 29, 49]. However, the two-step approach of ACI and MACI, which requires laboratory cell cultivation, results in a high financial and clinical burden. OATS results are reported to be similar to MACI, but allografts availability may be limited and cost intensive.
Recently, the minced cartilage procedure, a technique in which viable autologous cartilage is collected, sliced into small pieces, and reimplanted, has undergone renewed interest [51, 55]. Autologous thrombin and PRP, fibrin glue or a membrane might be additionally used for fragment fixation [42, 50,51,52]. Short-term outcomes in literature have been promising, but mid- and long-term results are lacking but urgently needed [8, 10, 42].
The aim of the present single-cohort study is to demonstrate minimum five-year outcome data of a cohort that underwent minced cartilage for the treatment of chondral and osteochondral lesions in the knee. It has been hypothesized that minced cartilage may maintain favourable clinical results over longer term follow-up, both in terms of patient-reported outcome measures and reoperation rates.
Materials and methods
Local ethical committee of the Canton of Zurich (KEK-ZH-Nr. 2015–0258) approval was obtained prior to study initiation. Informed consent was signed by all participants. The first 34 consecutive patients who underwent minced cartilage knee surgery between 2015 and 2016 were retrospectively analysed from a prospectively maintained database that routinely collected patient-related outcome data.
All patients were contacted personally by telephone for an interview and questionnaires were collected by mail. Electronic medical records were reviewed to obtain patient demographic, surgical, and imaging data.
Surgical procedure
Indication and detailed surgical treatment regimen was described previously [42]. All surgical interventions were performed by a single specialized and fellowship-trained orthopaedic surgeon (G.M.S.). All patients obtained a preoperative Magnetic Resonance Imaging (MRI) and conventional knee joint radiographs for diagnostic and surgical planning purposes. Patients with chondral or osteochondral lesions of the knee, who did not require any subchondral bone treatment were included in this study. Additionally, those with osteochondritis dissecans lesions not amenable to primary fixation, with otherwise healthy-appearing cartilage in the remaining compartments were included.
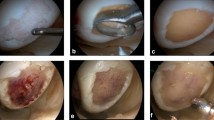
Final indication for performing a minced cartilage procedure was made following routine arthroscopy. In all cases, the second-generation repair technique was used as described previously [42, 50]. In brief, depending on the location of the chondral defect, a medial or lateral mini arthrotomy approach was performed and the lesion was inspected and measured. The defect was then debrided with a curette until a stable healthy cartilage rim was obtained. The healthy hyaline cartilage obtained from the debridement was collected and subsequently minced into small fragments of approximately 1 mm until a paste-like consistency was achieved. If an insufficient amount of cartilage was obtained, additional healthy cartilage was harvested from intercondylar notch using osteochondral cylindrical harvesters. Finally, minced cartilage was placed into the defect and sealed with fibrin glue or a combination of fibrin glue and membrane (Chondro-Gide, Geistlich Pharma).
Rehabilitation
An identical postoperative rehabilitation protocol was used in all patients with initial bed rest in a straight knee brace for 24 h. Continuous passive motion machine was started on the first postoperative day. For the first six weeks, partial weight-bearing was permitted with crutches and range of motion was limited to 0 to 90 degrees. After six weeks, a gradual increase in weight-bearing and range of motion was permitted, with full weight-bearing and unrestricted range of motion achieved at approximately nine weeks postoperatively.
Patient-reported outcome measures
Primary patient-reported outcome measures (PROMs), obtained preoperatively and at 12, 24 and 60 months of follow-up, were the numeric analogue scale (NAS) for pain and subjective knee function (0 = no pain/best function, 10 = worst pain/worst function). Secondary PROMs, including Lysholm, IKDC (International Knee Documentation Committee), COMI (Core Outcome Measurement Index) and Tegner activity score, were obtained at final follow-up only, as they were not routinely captured preoperatively from the patient-reported outcome data system. All postoperative complications and reoperations were recorded.
Radiological outcome measures
Preoperative 3-T MRI scans obtained at our institution were evaluated by a trained and blinded examiner using the AMADEUS (Area Measurement and Depth and Underlying Structures) score in order to quantify the severity of chondral and osteochondral defects prior to cartilage repair [33]. Intraoperative grading was performed according to the ICRS (International Cartilage Repair Society) grading system [3]. Hyaline cartilage or repair tissue were analysed using the MOCART (magnetic resonance observation of cartilage repair tissue, 0 = worst, 100 = best) score in all patients at 6 month postoperatively [40]. Preoperative and six-month postoperative outcomes have been published previously and are therefore not reported in the present study [42]. In addition to the planned study MRIs, all subsequent, unscheduled MRI examinations were captured as part of this study and analysed using MOCART 2.0 score by a single investigator who was blinded to the clinical outcome of the patients. The MOCART 2.0 score has been shown to have excellent interrater and intrarater reliability [53].
Statistical analysis
Statistical analysis was performed using SPSS (Version 28, IBM) and Microsoft Excel (Version 16). Normal distribution of the data was tested using the Kolmogorov–Smirnov test. Friedman test for dependent samples with Dunn-Bonferroni post-hoc test was used to compare NAS values at different study time points. Student’s t test or Mann–Whitney U test was applied to determine differences between groups. The patient-acceptable symptomatic state (PASS) threshold was employed as a tool to assess the minimum scores associated with patient satisfaction [30]. In cartilage repair, a final IKDC score of 62.1 and a Lysholm score of 70 have been reported to correspond with the PASS [6]. A difference between IKDC- and Lysholm score values greater than 9.2 and 13.0, respectively, was considered a clinically important difference (CID) [6]. Using G*Power (Version 3.1), the Wilcoxon signed-rank test for matched pairs with maximum correlation between the pre- and postoperative groups was used for a-priori sample size calculation. With α-level set to 0.05, β to 0.80, and assuming a one-tailed analysis, a total of 28 patients were deemed necessary to detect a one-point difference with two points standard deviation in the NAS for pain score. One-point difference in NAS for pain is within the reported minimal clinically important difference (MCID) of 2.7 points for cartilage procedures [32]. With an expected loss to follow-up rate of 20% at mid- to long-term, the first 34 consecutive patients were included in the study.
Results
A total of 34 consecutive patients treated with minced cartilage were included in the study. A detailed overview of patient characteristics and concomitant procedures is shown in Table 1. Cartilage defect characteristics are displayed in Table 2. The final follow-up after a mean of 65.5 ± 4.1 months was 82.4% (n = 28). Patients lost to follow-up did not differ in baseline characteristics or in intraoperative findings to those with complete mid-term follow-up.
Patient-reported outcome measurements
Overall, a statistically significant decrease in NAS for pain with a medium to strong effect size and a statistically significant (p < 0.001) increase in knee function with a medium to strong effect size were observed throughout the study period (Fig. 1). There was no statistically significant increase in postoperative pain or worsening of knee function at any of the three postoperative follow-up time points (Fig. 1).
Numeric analogue scale (NAS) for pain and knee function preoperative and one, two and five years postoperative. The asterisk marks a significant difference to the preoperative state: ***p < 0.001; **p < 0.01. No significant differences were observed between 1, 2 and 5 year postoperative follow-up. MCID: NAS for pain: 2.7
Gender, defect localization, concomitant interventions, defect characteristics as well as fixation techniques for minced cartilage seem to have little influence on postoperative outcomes with similar PROMs reported (Table 3). Statistical subgroup analysis was not performed because of missing power.
Of all patients 75% (n = 21) and 68% (n = 19) reached or exceeded the PASS for the IKDC- and Lysholm score at final follow-up, respectively.
Surgery-related complications and revision surgery
A total of four (14.2%) surgery-related complications were related directly to minced cartilage, one (3.5%) of which required revision surgery whereas the others (10.7%) resolved without surgical intervention. Five (17.8%) adverse events were related to the additional performed procedures (e.g. ACL reconstruction, MPFL reconstruction, etc.) and one (3.5%) event was linked to a traumatic accident (Table 4). If the assumption is made that all patients lost to follow-up had complications, the total complication rate would be 47.0%.
Radiological outcomes
Nineteen (67.8%) patients obtained a total of 23 unscheduled MRI at a mean of 41.8 ± 22.0 month after surgical intervention. Reasons for MRI included trauma, revision surgery, or pain (Table 5). The average overall MOCART 2.0 score including all examined patients and all anatomical sites (retropatellar, femoral condyle, trochlea) was 62.3 ± 17.4. MOCART 2.0 results including detailed information about all variables for each anatomical site and follow-up time point are shown in Table 5.
Discussion
The primary finding of the study was that second-generation minced cartilage procedure for the treatment of chondral and osteochondral lesions of the knee without the necessity for subchondral bone treatment is an effective and safe procedure with good mid-term results in terms of pain and knee function. The present 5-year data demonstrated no significant worsening of pain and function at mid-term compared to short-term follow-up.
The primary aim of minced cartilage is to recapitulate hyaline or hyaline-like cartilage at site of implantation from cell outgrowth, proliferation, and differentiation without the need for a two-step surgical process. Fragmentation of healthy cartilage has been shown to “activate” chondrocytes by increasing tissue surface and therefore promoting outgrowth [37, 51]. Outgrowth of chondrocytes results in proliferation and matrix production. This process is believed to be positively influenced by native joint physical-biomechanical inputs and the osteochondral microenvironment, as mechanical and biological stimuli have been shown to promote proliferation and chondrogenic differentiation [51, 56]. Several animal models have demonstrated the feasibility of minced cartilage showing better results compared to microfracturing, while demonstrating similar outcomes to two-stage autologous chondrocyte implantation [1, 9, 15, 26, 38, 41].
As it currently stands, there is only one prospective randomized clinical trial for single-stage autologous cartilage fragments procedure (CAIS, Cartilage Autograft Implantation System) [10] and three trials involving use of autologous minced cartilage with clinical follow-up of up to 24 months. [8, 12, 42]. Comparing two-year outcomes of patients randomly treated with either microfracturing (MFX) or CAIS shows significantly higher PROMs for CAIS [10]. There was no difference in the number of surgery-related complications, but a higher number of intralesional osteophyte formation in patients treated with MFX [10]. A statistical significant increase in MOCART scores and PROMs were also reported in eight patients with osteochondrosis dissecans treated with a combination of autologous bone and cartilage chips (ADTT, autologous dual-tissue transplantation) [8]. Similar, a statistically significant improvement between pre- and postoperative PROMs values were reported in fifteen patients treated with a novel autologous-made matrix, hyaline cartilage chips and platelet-rich growth factors [12]. In the present study, five-year outcomes indicate maintained low pain scores and knee function which are not statistically different from one- and two-year postoperative outcomes. Despite a slight increase in pain compared to one- and two-year results, the NAS pain values were within the limits of the minimal clinically important difference (MCID) and not statistically significantly different. Further long-term data are needed to assess the postoperative progression over time.
When comparing outcomes of different studies it is important to keep in mind, that several factors including surgical techniques, patient characteristics [48], previous or subsequent surgical interventions [48], defect size and location [23] as well as rehabilitation [20] have an influence on the postoperative outcome and limit therefore the direct comparability. Recently two-stage autologous chondrocyte implantation or osteochondral allograft transplantation (OATS), research showed promising mid-term results after MACI for medium to large defects [20, 24, 31]. A recent prospective randomized controlled trial (RCT) comparing MFX (61.8 ± 21.5) to MACI (68.5 ± 21.2) reported significant higher IKDC scores for the latter [4]. These findings are supported by recent meta-analysis showing no increased risk of clinical failure but superior improvements in PROMs for MACT compared to MFx at short- to mid-term [14] [20]. Contrary, other studies question the superiority of MACI over MFX [34, 35] or even report superiority of MFX especially in patients with only small chondral defects [47]. A prospective, controlled clinical trial studying the safety and efficacy of MACI with spheroid technology reported good and stable improvement of IKDC (74.6 ± 18.7) and KOOS (77.1 ± 18.6) scores after 48 months [46]. This is in accordance with several other mid- to long-term studies reporting stable improvements after ACI [2, 4, 11, 24, 36, 45, 57] When directly comparing ACI to OATS [43] fair to good mid-term IKDC outcomes (IKDC: 50 – 80) were reported [21]. Similarly, no significant differences at mid-term were found in PROM regarding outcomes between ACI and AMIC with VAS for pain scores ranging between 2.3 – 3- two years postoperative [25, 27, 54]. Patient-reported outcomes of the present study (IKDC: 71.6 ± 17.8) are comparable to MACI, OATS and AMIC results of the above-mentioned studies but appear to be higher than those reported for MFX [4]. Gender, concomitant injuries, defect localization, defect characteristics as well as fixation techniques for minced cartilage seem to have little influence on postoperative outcomes. Patients treated with one-staged minced cartilage for chondral and osteochondral knee defects can expect similar postoperative outcomes in the mid-term as compared to other established procedures.
Overall surgery-related complications and revision surgery are relatively low and comparable between different chondral regenerative techniques [18, 28, 44, 46]. Graft hypertrophy after MACI was reported in 12% of the patients after five years with a need for revision surgery in 8% [16]. Similar revision surgery rates were reported after five years in a prospective RCT rates comparing MACI (10.8%) and MFX (9.5%) [4]. In contrast, no graft hypertrophy was observed in a study using ACI (Spherox™, CO.DON AG, Germany; formerly known as chondrosphere) [45]. Mid-term outcome analysis of OATS revealed an 87% graft survival rate at 5 years with a 37% reoperation rate. These results were supported by a recent systematic review reporting similar survival rates (87%) and reoperation rates (30%) at mid- to long-term. In the present study, a total of four (14.2%) complications were primarily related to the minced cartilage procedure, one of which required revision surgery whereas the others resolved without surgical intervention. No revision operation was necessary due to graft hypertrophy or mechanical symptoms related to the chondral graft, although one patient reported still of occasional joint locking at 5 years, possibly related to graft hypertrophy. Altogether, this makes minced cartilage comparable to MFX and ACI in terms of surgery-related complication and revision surgery, and overall a safe and efficient procedure.
Despite the well-known lack of correlation between postoperative radiological outcomes and PROMs, radiological scoring remains relevant as a measure of structural change over time [17]. Two prospective randomized controlled trials reported mean MOCART scores of 76 ± 16 at two years and 75.5 ± 13.1 after 4 years, respectively [45, 46]. When comparing patellar and femoral condyle defects similar MOCART scores were observed [39, 58]. In the present study, only unscheduled follow-up MRIs within two and five years postoperatively were included, that were obtained for re-presentation due to recent trauma, pain, or revision surgery. Naturally, slightly lower MOCART 2.0 scores were therefore observed compared to the above-mentioned studies. Due to the nature of follow-up MRI indications in the present study, it can be assumed that MOCART 2.0 scores would be higher if the whole study cohort was included.
This work has some limitations. First, this study presents mid-term outcomes of the first series of patients undergoing minced cartilage of a single surgeon and therefore lacks a comparative group of patients treated with alternative osteochondral procedures such as ACI, OATS or MTX. Second, as consecutive patients were included and inclusion criteria were not limited to isolated cartilage defects, the heterogeneity of the study population might pose a limitation. However, a recent systematic review demonstrated good clinical outcomes after cartilage repair at the patellofemoral joint even in complex cases [5]. Third, the majority of the cartilage defects were located at the patella or femoral condyle and only a few at the trochlea or tibia. Therefore, the present results may not be applied without restriction to all cartilage defect locations in the knee joint. Moreover, overall outcomes might be lower, as less satisfactory results are for patients affected by cartilage lesions of the patella compared to other sides [23]. Due to the small sample size, statistical subgroup analyses were not possible, but the descriptive statistics appear to be comparable between the different defect localizations. Finally, while all patients obtained a preoperative and a six-month postoperative MRI scan, an additional, mid-term radiological examination for all patients would have been desirable; however, this was beyond the scope of the present work.
Minced cartilage procedure for the treatment of medium to large chondral and osteochondral defects of the knee, show good and promising results at mid-term. Minced cartilage procedure seems to be a viable treatment alternative in patients where a two-staged approach is not desired.
Conclusion
Patients treated with autologous minced cartilage procedure for medium to large chondral and osteochondral lesions of the knee without the necessity for subchondral bone treatment report good mid-term results in pain and knee function and low rates of postoperative adverse events. Pain and functional levels remain stable and within the MCID at mid-term.
Data availability
Not applicable.
References
Albrecht F, Roessner A (1978) Zimmermann E (1983) Closure of osteochondral lesions using chondral fragments and fibrin adhesive. Arch Orthop Trauma Surg 101(3):213–217
Barie A, Kruck P, Sorbi R, Rehnitz C, Oberle D, Walker T, Zeifang F, Moradi B (2020) Prospective long-term follow-up of autologous chondrocyte implantation with periosteum versus matrix-associated autologous chondrocyte implantation: a randomized clinical trial. Am J Sports Med 48(9):2230–2241
Brittberg M, Peterson L. Introduction to an articular cartilage classification. ICRS Cartilage Injury Evaluation Package. 1998; www.cartilage.org.
Brittberg M, Recker D, Ilgenfritz J, Saris DBF, Group SES (2018) Matrix-applied characterized autologous cultured chondrocytes versus microfracture: five-year follow-up of a prospective randomized trial. Am J Sports Med 46(6):1343–1351
Burger D, Feucht M, Muench LN, Forkel P, Imhoff AB, Mehl J (2022) Good clinical outcomes after patellar cartilage repair with no evidence for inferior results in complex cases with the need for additional patellofemoral realignment procedures: a systematic review. Knee Surg Sports Traumatol Arthrosc 30(5):1752–1768
Chahal J, Lansdown DA, Davey A, Davis AM, Cole BJ (2021) The clinically important difference and patient acceptable symptomatic state for commonly used patient-reported outcomes after knee cartilage repair. Am J Sports Med 49(1):193–199
Chimutengwende-Gordon M, Donaldson J, Bentley G (2020) Current solutions for the treatment of chronic articular cartilage defects in the knee. EFORT Open Rev 5(3):156–163
Christensen BB, Foldager CB, Jensen J, Lind M (2015) Autologous dual-tissue transplantation for osteochondral repair: early clinical and radiological results. Cartilage 6(3):166–173
Christensen BB, Foldager CB, Olesen ML, Hede KC, Lind M (2016) Implantation of autologous cartilage chips improves cartilage repair tissue quality in osteochondral defects: a study in gottingen minipigs. Am J Sports Med 44(6):1597–1604
Cole BJ, Farr J, Winalski CS, Hosea T, Richmond J, Mandelbaum B, De Deyne PG (2011) Outcomes after a single-stage procedure for cell-based cartilage repair: a prospective clinical safety trial with 2-year follow-up. Am J Sports Med 39(6):1170–1179
Colombini A, Libonati F, Lopa S, Peretti GM, Moretti M, de Girolamo L (2023) Autologous chondrocyte implantation provides good long-term clinical results in the treatment of knee osteoarthritis: a systematic review. Knee Surg Sports Traumatol Arthrosc 31(6):2338–2348
Cugat R, Alentorn-Geli E, Navarro J, Cusco X, Steinbacher G, Seijas R, Alvarez-Diaz P, Barastegui D, Laiz P, Samitier G, Garcia-Balletbo M (2020) A novel autologous-made matrix using hyaline cartilage chips and platelet-rich growth factors for the treatment of full-thickness cartilage or osteochondral defects: preliminary results. J Orthop Surg (Hong Kong) 28(1):2309499019887547
Dekker TJ, Aman ZS, DePhillipo NN, Dickens JF, Anz AW, LaPrade RF (2021) Chondral lesions of the knee: an evidence-based approach. J Bone Joint Surg Am 103(7):629–645
Dhillon J, Decilveo AP, Kraeutler MJ, Belk JW, McCulloch PC, Scillia AJ (2022) Third-generation autologous chondrocyte implantation (cells cultured within collagen membrane) is superior to microfracture for focal chondral defects of the knee joint: systematic review and meta-analysis. Arthroscopy 38(8):2579–2586
Dominguez Perez JM, Fernandez-Sarmiento JA, Aguilar Garcia D, Granados Machuca MDM, Morgaz Rodriguez J, Navarrete Calvo R, Perez Arevalo J, Carrillo Poveda JM, Alentorn-Geli E, Laiz Boada P, Cugat Bertomeu R (2019) Cartilage regeneration using a novel autologous growth factors-based matrix for full-thickness defects in sheep. Knee Surg Sports Traumatol Arthrosc 27(3):950–961
Ebert JR, Robertson WB, Woodhouse J, Fallon M, Zheng MH, Ackland T, Wood DJ (2011) Clinical and magnetic resonance imaging-based outcomes to 5 years after matrix-induced autologous chondrocyte implantation to address articular cartilage defects in the knee. Am J Sports Med 39(4):753–763
Ebert JR, Smith A, Fallon M, Wood DJ, Ackland TR (2014) Correlation between clinical and radiological outcomes after matrix-induced autologous chondrocyte implantation in the femoral condyles. Am J Sports Med 42(8):1857–1864
Ehmann YJ, Esser T, Seyam A, Rupp MC, Mehl J, Siebenlist S, Imhoff AB, Minzlaff P (2023) Low postoperative complication rate with high survival rate and good clinical outcome 9 years after autologous chondrocyte transplantation of the knee joint. Arch Orthop Trauma Surg 143(5):2665–2674
Evenbratt H, Andreasson L, Bicknell V, Brittberg M, Mobini R, Simonsson S (2022) Insights into the present and future of cartilage regeneration and joint repair. Cell Regen 11(1):3
Everhart JS, Jiang EX, Poland SG, Du A, Flanigan DC (2021) Failures, reoperations, and improvement in knee symptoms following matrix-assisted autologous chondrocyte transplantation: a meta-analysis of prospective comparative trials. Cartilage 13(1_suppl):1022S–1035S. https://doi.org/10.1177/1947603519870861
Familiari F, Cinque ME, Chahla J, Godin JA, Olesen ML, Moatshe G, LaPrade RF (2018) Clinical outcomes and failure rates of osteochondral allograft transplantation in the knee: a systematic review. Am J Sports Med 46(14):3541–3549
Filardo G, Andriolo L, Angele P, Berruto M, Brittberg M, Condello V, Chubinskaya S, de Girolamo L, Di Martino A, Di Matteo B, Gille J, Gobbi A, Lattermann C, Nakamura N, Nehrer S, Peretti GM, Shabshin N, Verdonk P, Zaslav K, Kon E (2021) Scaffolds for knee chondral and osteochondral defects: indications for different clinical scenarios. a consensus statement. Cartilage 13(1_suppl):1036S–1046S. https://doi.org/10.1177/1947603519894729
Filardo G, Kon E, Andriolo L, Di Martino A, Zaffagnini S, Marcacci M (2014) Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: a comparison of patellar and trochlear lesions. Am J Sports Med 42(3):626–634
Filardo G, Kon E, Andriolo L, Di Matteo B, Balboni F, Marcacci M (2014) Clinical profiling in cartilage regeneration: prognostic factors for midterm results of matrix-assisted autologous chondrocyte transplantation. Am J Sports Med 42(4):898–905
Fossum V, Hansen AK, Wilsgaard T, Knutsen G (2019) Collagen-covered autologous chondrocyte implantation versus autologous matrix-induced chondrogenesis: a randomized trial comparing 2 methods for repair of cartilage defects of the knee. Orthop J Sports Med 7(9):2325967119868212
Frisbie DD, Lu Y, Kawcak CE, DiCarlo EF, Binette F, McIlwraith CW (2009) In vivo evaluation of autologous cartilage fragment-loaded scaffolds implanted into equine articular defects and compared with autologous chondrocyte implantation. Am J Sports Med 37(Suppl 1):71S–80S
Gille J, Reiss E, Freitag M, Schagemann J, Steinwachs M, Piontek T, Reiss E (2021) Autologous matrix-induced chondrogenesis for treatment of focal cartilage defects in the knee: a follow-up study. Orthop J Sports Med 9(2):2325967120981872
Gou GH, Tseng FJ, Wang SH, Chen PJ, Shyu JF, Weng CF, Pan RY (2020) Autologous chondrocyte implantation versus microfracture in the knee: a meta-analysis and systematic review. Arthroscopy 36(1):289–303
Grevenstein D, Mamilos A, Schmitt VH, Niedermair T, Wagner W, Kirkpatrick CJ, Brochhausen C (2021) Excellent histological results in terms of articular cartilage regeneration after spheroid-based autologous chondrocyte implantation (ACI). Knee Surg Sports Traumatol Arthrosc 29(2):417–421
Harris JD, Brand JC, Cote MP, Faucett SC, Dhawan A (2017) Research pearls: the significance of statistics and perils of pooling. Part 1: clinical versus statistical significance. Arthroscopy 33(6):1102–1112
Hoburg A, Niemeyer P, Laute V, Zinser W, John T, Becher C, Izadpanah K, Diehl P, Kolombe T, Fay J, Siebold R, Fickert S (2022) Safety and efficacy of matrix-associated autologous chondrocyte implantation with spheroids for patellofemoral or tibiofemoral defects: a 5-year follow-up of a phase 2. Dose-Confirmation Trial Orthop J Sports Med 10(1):23259671211053380
Jones KJ, Kelley BV, Arshi A, McAllister DR, Fabricant PD (2019) Comparative effectiveness of cartilage repair with respect to the minimal clinically important difference. Am J Sports Med 47(13):3284–3293
Jungmann PM, Welsch GH, Brittberg M, Trattnig S, Braun S, Imhoff AB, Salzmann GM (2017) Magnetic resonance imaging score and classification system (AMADEUS) for assessment of preoperative cartilage defect severity. Cartilage 8(3):272–282
Knutsen G, Drogset JO, Engebretsen L, Grontvedt T, Isaksen V, Ludvigsen TC, Roberts S, Solheim E, Strand T, Johansen O (2007) A randomized trial comparing autologous chondrocyte implantation with microfracture. Findings at five years. J Bone Joint Surg Am 89(10):2105–2112
Kraeutler MJ, Belk JW, Purcell JM, McCarty EC (2018) Microfracture versus autologous chondrocyte implantation for articular cartilage lesions in the knee: a systematic review of 5-year outcomes. Am J Sports Med 46(4):995–999
Kreuz PC, Kalkreuth RH, Niemeyer P, Uhl M, Erggelet C (2019) Long-term clinical and MRI results of matrix-assisted autologous chondrocyte implantation for articular cartilage defects of the knee. Cartilage 10(3):305–313
Levinson C, Cavalli E, Sindi DM, Kessel B, Zenobi-Wong M, Preiss S, Salzmann G, Neidenbach P (2019) Chondrocytes from device-minced articular cartilage show potent outgrowth into fibrin and collagen hydrogels. Orthop J Sports Med 7(9):2325967119867618
Lind M, Larsen A (2008) Equal cartilage repair response between autologous chondrocytes in a collagen scaffold and minced cartilage under a collagen scaffold: an in vivo study in goats. Connect Tissue Res 49(6):437–442
Marlovits S, Aldrian S, Wondrasch B, Zak L, Albrecht C, Welsch G, Trattnig S (2012) Clinical and radiological outcomes 5 years after matrix-induced autologous chondrocyte implantation in patients with symptomatic, traumatic chondral defects. Am J Sports Med 40(10):2273–2280
Marlovits S, Singer P, Zeller P, Mandl I, Haller J, Trattnig S (2006) Magnetic resonance observation of cartilage repair tissue (MOCART) for the evaluation of autologous chondrocyte transplantation: determination of interobserver variability and correlation to clinical outcome after 2 years. Eur J Radiol 57(1):16–23
Marmotti A, Bruzzone M, Bonasia DE, Castoldi F, Rossi R, Piras L, Maiello A, Realmuto C, Peretti GM (2012) One-step osteochondral repair with cartilage fragments in a composite scaffold. Knee Surg Sports Traumatol Arthrosc 20(12):2590–2601
Massen FK, Inauen CR, Harder LP, Runer A, Preiss S, Salzmann GM (2019) One-step autologous minced cartilage procedure for the treatment of knee joint chondral and osteochondral lesions: a series of 27 patients with 2-year follow-up. Orthop J Sports Med 7(6):2325967119853773
Matthews JR, Brutico JM, Abraham DT, Heard JC, Tucker BS, Tjoumakaris FP, Freedman KB (2022) Differences in clinical and functional outcomes between osteochondral allograft transplantation and autologous chondrocyte implantation for the treatment of focal articular cartilage defects. Orthop J Sports Med 10(2):23259671211058424
Migliorini F, Eschweiler J, Schenker H, Baroncini A, Tingart M, Maffulli N (2021) Surgical management of focal chondral defects of the knee: a Bayesian network meta-analysis. J Orthop Surg Res 16(1):543
Niemeyer P, Laute V, Zinser W, Becher C, Kolombe T, Fay J, Pietsch S, Kuzma T, Widuchowski W, Fickert S (2019) A Prospective, randomized, open-label, multicenter, phase III noninferiority trial to compare the clinical efficacy of matrix-associated autologous chondrocyte implantation with spheroid technology versus arthroscopic microfracture for cartilage defects of the knee. Orthop J Sports Med 7(7):2325967119854442
Niemeyer P, Laute V, Zinser W, John T, Becher C, Diehl P, Kolombe T, Fay J, Siebold R, Fickert S (2020) Safety and efficacy of matrix-associated autologous chondrocyte implantation with spheroid technology is independent of spheroid dose after 4 years. Knee Surg Sports Traumatol Arthrosc 28(4):1130–1143
Ossendorff R, Franke K, Erdle B, Uhl M, Sudkamp NP, Salzmann GM (2019) Clinical and radiographical ten years long-term outcome of microfracture vs. autologous chondrocyte implantation: a matched-pair analysis. Int Orthop 43(3):553–559
Pareek A, Reardon PJ, Maak TG, Levy BA, Stuart MJ, Krych AJ (2016) Long-term outcomes after osteochondral autograft transfer: a systematic review at mean follow-up of 10.2 years. Arthroscopy 32(6):1174–1184
Riboh JC, Cvetanovich GL, Cole BJ, Yanke AB (2017) Comparative efficacy of cartilage repair procedures in the knee: a network meta-analysis. Knee Surg Sports Traumatol Arthrosc 25(12):3786–3799
Salzmann GM, Calek AK, Preiss S (2017) Second-generation autologous minced cartilage repair technique. Arthrosc Tech 6(1):e127–e131. https://doi.org/10.1016/j.eats.2016.09.011
Salzmann GM, Ossendorff R, Gilat R, Cole BJ (2021) Autologous minced cartilage implantation for treatment of chondral and osteochondral lesions in the knee joint: an overview. Cartilage 13(1_suppl):1124S–1136S. https://doi.org/10.1177/1947603520942952
Schneider S, Ossendorff R, Holz J, Salzmann GM (2021) Arthroscopic minced cartilage implantation (MCI): a technical note. Arthrosc Tech 10(1):e97–e101. https://doi.org/10.1016/j.eats.2020.09.015
Schreiner MM, Raudner M, Marlovits S, Bohndorf K, Weber M, Zalaudek M, Rohrich S, Szomolanyi P, Filardo G, Windhager R, Trattnig S (2021) The MOCART (magnetic resonance observation of cartilage repair tissue) 2.0 knee score and atlas. Cartilage 13(1_suppl):571S–587S
Snow M, Middleton L, Mehta S, Roberts A, Gray R, Richardson J, Kuiper JH, Consortium A, Smith A, White S, Roberts S, Griffiths D, Mohammed A, Moholkar K, Ashraf T, Green M, Hutchinson J, Bhullar T, Chitnis S, Shaw A, van Niekerk L, Hui A, Drogset JO, Knutsen G, McNicholas M, Bowditch M, Johnson D, Turner P, Chugh S, Hunt N, Ali S, Palmer S, Perry A, Davidson A, Hill P, Deo S, Satish V, Radford M, Langstaff R, Houlihan-Burne D, Spicer D, Phaltankar P, Hegab A, Marsh D, Cannon S, Briggs T, Pollock R, Carrington R, Skinner J, Bentley G, Price A, Schranz P, Mandalia V, O’Brien S (2023) A randomized trial of autologous chondrocyte implantation versus alternative forms of surgical cartilage management in patients with a failed primary treatment for chondral or osteochondral defects in the knee. Am J Sports Med 51(2):367–378
Tseng TH, Jiang CC, Lan HH, Chen CN, Chiang H (2020) The five year outcome of a clinical feasibility study using a biphasic construct with minced autologous cartilage to repair osteochondral defects in the knee. Int Orthop 44(9):1745–1754
Tsuyuguchi Y, Nakasa T, Ishikawa M, Miyaki S, Matsushita R, Kanemitsu M, Adachi N (2021) The benefit of minced cartilage over isolated chondrocytes in atelocollagen gel on chondrocyte proliferation and migration. Cartilage 12(1):93–101
Vanlauwe J, Saris DB, Victor J, Almqvist KF, Bellemans J, Luyten FP, Tig/Act, Group EXTS (2011) Five-year outcome of characterized chondrocyte implantation versus microfracture for symptomatic cartilage defects of the knee: early treatment matters. Am J Sports Med 39(12):2566–2574
Welsch GH, Mamisch TC, Quirbach S, Zak L, Marlovits S, Trattnig S (2009) Evaluation and comparison of cartilage repair tissue of the patella and medial femoral condyle by using morphological MRI and biochemical zonal T2 mapping. Eur Radiol 19(5):1253–1262
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
AR: contributed to conceptualization, data curation, formal analysis, methodology, project administration, resources, writing—original draft, and writing—review and editing. RO: contributed to conceptualization, data curation, formal analysis, methodology, and writing—review and editing. FÖ: contributed to conceptualization, data curation, formal analysis, methodology, and writing—review and editing. VAS: contributed to conceptualization, data curation, formal analysis, resources, methodology, and writing—review and editing. SS: contributed to conceptualization, data curation, formal analysis, methodology, writing—review and editing, and supervision. SP: contributed to formal analysis, methodology, resources, writing—review and editing, and supervision. GMS: contributed to conceptualization, data curation, formal analysis, methodology, project administration, writing—review and editing, and supervision. JH: contributed to conceptualization, data curation, formal analysis, methodology, project administration, resources, and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
All other authors declare that they have no conflict of interest.
Disclosures
Salzmann GM is a consultant for Arthrex.
Ethical approval
Ethical approval for this study was obtained from the local ethical committee of the Canton Zurich (KEK-ZH-Nr. 2015-0258).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Investigation performend at Schulthess Klinik, Zurich, Switzerland.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Runer, A., Ossendorff, R., Öttl, F. et al. Autologous minced cartilage repair for chondral and osteochondral lesions of the knee joint demonstrates good postoperative outcomes and low reoperation rates at minimum five-year follow-up. Knee Surg Sports Traumatol Arthrosc 31, 4977–4987 (2023). https://doi.org/10.1007/s00167-023-07546-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07546-1