Abstract
Purpose
Focal, patellar cartilage defects are a challenging problem as most cases have an underlying multifactorial pathogenesis. This systematic review of current literature analysed clinical results after regenerative cartilage repair of the patella with a special focus on the assessment and treatment of existing patellofemoral malalignment.
Methods
A systematic review was conducted to identify articles reporting clinical results after cartilage regenerative surgeries of the patella using the PubMed and Scopus database. The extracted data included patient-reported outcome measures (PROMS) and whether cartilage repair was performed alone or in combination with concomitant surgeries of underlying patellofemoral co-pathologies. In cases of isolated cartilage repair, specific exclusion criteria regarding underlying co-pathologies were screened. In cases of concomitant surgeries, the type of surgeries and their specific indications were extracted.
Results
A total of 35 original articles were included out of which 27 (77%) were cohort studies with level IV evidence. The most frequently used technique for cartilage restoration of the patella was autologous chondrocyte implantation (ACI). Results after isolated cartilage repair alone were reported by 15 (43%) studies. Of those studies, 9 (60%) excluded patients with underlying patellofemoral malalignment a priori and 6 (40%) did not analyse underlying co-pathologies at all. Among the studies including combined surgeries, the most frequently reported concomitant procedures were release of the lateral retinaculum, reconstruction of the medial patellofemoral ligament (MPFL), and osteotomy of the tibial tubercle. In summary, these studies showed lower preoperative PROMS but similar final PROMS in comparison with the studies reporting on isolated cartilage repair. The most frequently used PROMS were the IKDC-, Lysholm- and the Modified Cincinnati Score.
Conclusion
This comprehensive literature review demonstrated good clinical outcomes after patellar cartilage repair with no evidence of minor results even in complex cases with the need for additional patellofemoral realignment procedures. However, a meaningful statistical comparison between isolated patellar cartilage repair and combined co-procedures is not possible due to very heterogeneous patient cohorts and a lack of analysis of specific subgroups in recent literature.
Level of evidence
Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Focal cartilage defects of the knee are a common problem, especially in young and active patients as they can lead to pain, swelling and altered joint function [30]. Additionally, there is evidence that these defects are associated with an increased risk of early osteoarthritis over time [12, 64].
Although the general benefit of cartilage regenerative surgeries in the knee has been proven, the patellofemoral joint has often been considered a problematic location by many previous studies [16, 49, 51, 55, 63]. A recent systematic review by Hinckel et al. including 59 articles, did not confirm these concerns. This review showed that cartilage restoration of the patellofemoral joint led to improved clinical outcomes along with low complication rates [32]. However, the authors also reported that lesions at the patella may lead to worse results in direct comparison with those at the trochlea.
Focal cartilage defects of the patella are challenging as in most cases a multifactorial pathogenesis is underlying. It is known that patella dislocations lead to cartilage defects in up to 95% of cases and the risk of (osteo-)chondral flake fractures is reported in up to 58% of patients [41, 50, 58]. Since the risk for re-dislocation of the patella is almost 50% within the first 2 years, additional patella stabilisation is necessary, if surgical therapy of the cartilage defect is planned [4]. Consequently, predisposing factors for patella instability must be analysed and considered when appropriate [72]. Factors include trochlea dysplasia, patella alta, increased tibial tuberosity–trochlea groove (TTTG) distance, genu valgum and increased femoral torsion. [1, 4, 14, 33, 71]
However, even without history of patella dislocation, cartilage defects of the patellofemoral joint are highly associated with co-pathologies, whereas trochlea dysplasia, patella alta and increased lateral patella tilt seem to be particularly predisposing [3, 44]. Therefore, also in these cases, possible co-pathologies must be properly analysed and considered carefully if surgical treatment of patellar cartilage defects is planned. Additionally, for correct interpretation of clinical results after regenerative cartilage procedures at the patella, information regarding the presence and, if applicable, about the surgical treatment of these co-pathologies is necessary. To date, the influence of concomitant procedures addressing patellofemoral stability and alignment in combination with surgical cartilage restoration at the patella is still unclear.
The purpose of the present study was to perform a systematic literature review of clinical trials investigating the results after regenerative cartilage repair of the patella. Among these studies, a special focus was set on the analysis and treatment of preoperative co-pathologies.
It was hypothesised that in most of the included studies, patients with relevant co-pathologies were excluded a priori or a proper presentation of co-pathologies did not exist. Additionally, it was hypothesised that additional treatment of co-pathologies would lead to similar results in comparison with isolated regenerative cartilage therapy at the patella.
Materials and methods
Search details
A comprehensive literature search to identify articles reporting clinical results after cartilage regenerative surgeries at the patella was conducted according to the PRISMA statement (Preferred Reporting Items for Systematic Reviews and Meta-Analysis) [40]. The PubMed database and the Scopus database were used for this literature research.
Inclusion and exclusion criteria
Inclusion criteria to qualify for this systematic review were:
-
1.
Clinical trials reporting results after regenerative cartilage therapy for focal cartilage defects at the patella.
-
2.
Results reported by means of patient-reported outcome measures (PROMs).
-
3.
Level of evidence (LOE) 1–4.
-
4.
English language.
Exclusion criteria were:
-
1.
Publication dates earlier than the year 2000.
-
2.
Follow-up less than 12 months.
-
3.
Less than 5 patients with cartilage lesions located at the patella.
-
4.
No outcomes reported separately for patients with cartilage lesions located at the patella.
-
5.
Only children and adolescents included.
-
6.
Other systematic reviews and meta-analyses.
Search strategy
Different combinations of the following keywords were used for the initial data base search: cartilage repair, cartilage restoration, cartilage transplantation, cartilage implantation, microfracture, microfracturing, osteochondral autologous transfer, OATS, mosaicplasty, osteochondral allograft transplantation, autologous chondrocyte implantation, ACI, MACI, patella, patellar, patellofemoral. The search was performed in April 2020. All abstracts of the identified publications were judged for inclusion suitability primarily by authors DB and JM. If the abstract showed any inclusion criteria, the entire paper was read. All authors performed the analysis of the articles based on the inclusion and exclusion criteria and all authors had to agree to include or exclude an article.
If two separate studies had the same authors and intervention but had different follow-up, then only the study with the longer follow-up was included for the outcome analysis.
Study quality
The quality of the included studies was analysed by means of the Methodological Index for Non-Randomised Studies (MINORS), which consists of eight items for non-comparative studies and four additional items for comparative studies [62]. A maximum of 2 points can be assigned to each item, resulting in a maximum score of 16 points for non-comparative studies and 24 points for comparative studies. The assessment was performed independently by two reviewers (DB, JM) and the final score was determined by consensus. Additionally, the level of evidence (LOE) of the included studies was registered.
Data extraction and analysis
For all included studies, the extraction of data included: the first author’s name, publication year, journal, study design, LOE, MINORS, number of cases with patellar cartilage defects, patients’ age, follow-up time, defect size, and surgical technique. In the case of comparative studies, the definition of the study groups was documented. If subgroups of patients with patellar cartilage defects were defined and the demographic data and results were given separately, only this data was extracted. As already mentioned above, studies with no separate data for patellar defects were excluded from the analysis. This also applied for studies that combined patellofemoral cartilage defects into one study group.
For all included studies, the used PROMS were noted and the corresponding results were analysed. If a comparison of preoperative PROMS with PROMS at final follow-up was performed, the p-value representing a possible significant difference was documented. If a comparison with preoperative PROMS was not performed or if a p value was not given, the main outcome of the studies was extracted as a short summary.
Furthermore, all included studies were analysed whether isolated cartilage repair alone was performed, or concomitant surgeries of underlying co-pathologies were performed in combination with cartilage repair.
In the case of isolated cartilage repair, the specific inclusion and exclusion criteria were analysed to further characterise the study cohort and to evaluate if patients with typical co-pathologies were excluded.
In the case of concomitant surgeries, the type of surgeries and, if given, the specific indications for these surgeries were extracted. For studies that directly compared patients with and without concomitant surgeries, the results were extracted for each group separately.
Statistical analysis
The extracted quantitative parameters (age, follow-up time, defect size and results of the PROMs) were given as mean ± standard deviation (SD), when provided in the articles. Otherwise, alternative values like median or range were extracted.
Due to the high statistical and methodological heterogeneity of the included studies, a meta-analysis comparing the results between patients with and without concomitant surgeries was not possible. Instead, a narrative description and comparison of the clinical results was performed.
Results
Search results and study design
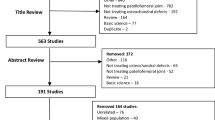
After screening for eligible studies, a total of 35 original articles were identified and included in this systematic review (Fig. 1, Table 1). With 27 studies (80%), the vast majority were prospective or retrospective cohort studies with level IV evidence. The mean MINORS score was 13.3 of 16 (range from 10 to 16) for non-comparative studies and 20.1 of 24 (range from 16 to 23) for comparative studies. The number of reported cases ranged from 6 to 110, the mean age of the included patients ranged from 15 to 39.2 years, and the mean follow-up time ranged from 24 to 153 months. The most frequently used techniques for cartilage restoration were autologous chondrocyte implantation (ACI) in 48.6% and autologous osteochondral transplantation (AOT) in 22.9% of cases. The range of retropatellar cartilage defect sizes in studies using the ACI technique was 2.8–6.4 cm2 and for AOT 1.16–1.6 cm2.
Isolated cartilage repair
In this systematic review, 15 studies (43%) reported on patellar cartilage repair without any concomitant surgeries. Detailed information about the inclusion/exclusion criteria and the main results of these 15 studies are presented in Table 2 (online addition). The analysis showed that underlying pathologies were not reported at all (6 studies) or patients with appropriate co-pathologies were excluded a priori (9 studies). The most often reported exclusion criteria of co-pathologies were tibio-femoral varus/valgus malalignment (6x) and patellofemoral malalignment, such as patella alta or baja (3x), increased patellar tilt (3x), increased patellar shift (1x), increased TTTG > 15 mm (1x) or trochlea dysplasia (1x). Eleven out of the 15 surveys with isolated patellar cartilage repair (73%) reported at least one significantly improved patient-reported outcome measure (PROMs) of which as many as 16 different scores were assessed. The most often significantly improved PROMs postoperatively reported were the Lysholm- (5x) and the Kujala-score (3x). On average, the mean values improved from 61.6 (range 42.7–73.8) to 90.9 (range 67.6–95) for the Lysholm score and from 49.3 (range 44.9–54.8) to 76.8 (range 75.2–78.4) for the Kujala score.
Concomitant surgeries
In 20 of the 35 studies (57%), patients with the need for additional procedures due to underlying patellofemoral co-pathologies were included. Detailed information about the concomitant surgeries, their indications and the main results of these 20 studies are presented in Table 3 (online addition). Among these studies, eight (40%) reported on either soft-tissue or bony realignment procedures, and six (30%) on both soft-tissue and bony realignment procedures. Another four studies (20%) included a mixture of patients with additional soft-tissue or bony realignment procedures or the combination of both. In one study, cartilage repair was combined with soft-tissue procedures only, and in another study, it was combined with bony realignment procedures only. In 17 studies, the results of both isolated cartilage repair and cartilage repair combined with surgery of concomitant pathologies were merged. There were three studies that only reported on combined surgical approaches. [22,23,24]
The most frequently reported concomitant soft-tissue procedures were the release of the lateral retinaculum (14 studies) and the reconstruction of the MPFL (7 studies). Concomitant bony procedures were osteotomies of the tibial tubercle (17 studies), trochleaplasties (4 studies) and high tibial osteotomies (4 studies).
Among all the studies that included patients after combined surgery, 70% (14 out of 20) reported at least one significantly improved postoperative PROM, of which as many as 19 different scores were assessed. The most often significantly improved PROMs postoperatively reported were the IKDC- (11x), the Modified Cincinnati- (6x) and the Lysholm-scores (4x). On the average, the mean values improved from 41.9 (range 36.2–51) to 72.1 (range 66.3–79.4) for the IKDC-Score, from 3.1 (range 2–3.6) to 6.4 (range 5.1–8) for the Modified Cincinnati score and from 51.9 (range 40.2–69) to 83.1 (range 66–92.5) for the Lysholm-Score.
An isolated analysis of the 3 studies, which reported on combined surgical approaches only, demonstrated statistically significant improvements of all PROMs for 2 studies. [23, 24] The third study showed an improvement of the PROMs, however a statistical analysis was missing. [22]
While most of these 20 studies included heterogeneous patient groups with different combinations of surgical procedures, only one study reported on a homogeneous study group with the same treatment approach for all included patients [23]. Gigante et al. investigated the outcome of 14 patients with MACI for retropatellar chondral lesions in combination with TTO because of patellofemoral malalignment and TTTG > 20 mm. The results showed a significant improvement of all scores after a mean follow-up of 36 months. Additionally, there was only one retrospective comparative study, which directly compared the results of isolated retropatellar cartilage repair with a combination of cartilage repair and the correction of patellofemoral malalignment [31].
The analysis of indications for concomitant surgeries gave a very heterogeneous picture. In 6 out of 20 studies, no specific indications for additional patellofemoral procedures were defined at all. Among the other 14 studies, the indication was based on clinical evaluations and/or radiological values. The most frequently reported indications for additional procedures were patellofemoral malalignment or maltracking (7x), history of patella dislocation or patellofemoral instability (6x), excessive patella tilt (3x) and trochlea dysplasia (3x). In 4 studies, an increased TTTG distance was defined as indication for additional realignment, with 3 studies setting the cut-off value at 15 mm and one study at 20 mm.
Discussion
The most important finding of the present systematic review was that both isolated patellar cartilage repair alone and patellar cartilage repair combined with patellofemoral alignment correction led to good clinical results.
However, considering the fact that patellofemoral malalignment has been discussed as a risk factor for negative outcomes after patellar cartilage surgery already for several decades[10, 17, 23, 60], a rather surprising finding was that more than 40% of the included studies did not include patients with concomitant surgeries for underlying patellofemoral co-pathologies.
On the other hand, more than half of the identified studies did include patients with the need for additional patellofemoral stabilisation or realignment in combination with cartilage repair at the patella. Most of these studies reported on different combinations of concomitant surgeries and summarised the clinical outcome scores without analysing specific subgroups regarding the surgical approach.
The studies including combined surgical procedures reported good clinical outcomes with a significant improvement of at least one PROM in 14 of 20 studies (70%), while the remaining 6 studies demonstrated an improvement in at least one PROM, but without any statistical significance [29, 47, 55] or a statistical analysis was not available [22, 37, 73]. These results were similar to the studies reporting on isolated cartilage repair at the patella with 11 of 15 studies (73%) observing significant improvements of at least one PROM in the postoperative course. This may support the hypothesis that the need for additional patella stabilisation or realignment is not correlated with worse clinical outcomes. However, due to the very heterogeneous patient cohorts and missing analysis of specific subgroups, comparison between isolated patellar cartilage repair and combined procedures is limited.
Among the 35 included studies, there was only one which directly compared the outcome of isolated chondral repair with chondral repair and simultaneously addressing underlying patellofemoral malalignment[31]. Henderson et al. investigated 22 patients after ACI-P only and 22 patients after ACI-P in combination with lateral release, TTO and MPFL tensioning. Both groups showed improved final follow-up scores with significantly worse results for the ACI-P only group.
The efficacy of cartilage repair surgeries in the patellofemoral joint has been proven by several studies investigating different surgical techniques [15, 18, 32, 67, 68, 75]. However, a recent systematic review concluded that lesions at the patella might lead to worse results in comparison with the trochlea. One reason for this finding may be the fact that anatomic patellofemoral risk factors are more often associated with cartilage defects at the patella in comparison with the trochlea [3]. Because of these etiological and clinical differences between the patellar and trochlear location, only studies reporting outcomes after cartilage repair at the patella were included in the present literature review.
The high prevalence of anatomic risk factors in association with cartilage defects at the patella has been shown by several studies [3, 21, 44]. Therefore, the main focus of the present review was set on how underlying co-pathologies were taken into account when reporting the results after cartilage repair at the patella. Almost half of the included studies reported on isolated cartilage repair surgery at the patella without any additional procedures. In several of these studies, inclusion and exclusion criteria were not adequately reported and it is not clear if patellofemoral risk factors were present among the treated patients. Therefore, the value of these studies has to be considered as very limited. However, most of the included studies reporting on isolated cartilage repair at the patella stated sufficient information regarding inclusion and exclusion criteria. In most of these studies, patients with significant patellofemoral malalignment were excluded based on clinical evaluation or radiological measurements. On the one hand, these strict selection criteria enable a homogeneous study collective and subsequently a good evaluation of the efficacy of the cartilage repair technique itself. On the other hand, however, the study collectives do not represent the majority of patients affected by patellar cartilage defects, considering the high association with anatomic risk factors of up to 88% [44]. The exclusion of patients with patellofemoral malalignment may lead to a distortion of the results because more complex cases were not investigated. This statement can be supported by the fact that the preoperative scores demonstrated higher values among the studies with cartilage repair alone in comparison with the studies including patients with the need for additional procedures (Lysholm score 61.6 vs. 51.9).
Several studies consistently concluded that the avoidance of correcting underlying co-pathologies of retropatellar chondral lesions leads to poorer outcomes [10, 53, 54]. Anatomic abnormalities which have been proven to correlate with cartilage lesions in the patellofemoral joint are trochlea dysplasia, increased TTTG distance, genu valgum and increased femoral antetorsion, while in most cases a combination of these factors is present [3, 21, 43, 44].
Among the 20 studies, including patients who underwent concomitant surgeries, the most frequently performed additional soft-tissue procedures were lateral retinaculum release and MPFL reconstruction, while the most frequently performed bony procedures were osteotomies of the tibial tubercle. All of these techniques have been demonstrated to be successful options to improve patellofemoral alignment[36, 56, 59, 61]. Although trochlea dysplasia has been shown to be one of the most frequent co-pathologies in patients with patellar cartilage defects, trochleoplasty has been performed only in very few cases. A recent study investigated the influence of trochlea dysplasia on the outcome after patellofemoral ACI by means of a comparative matched-pair analysis between 23 patients with high-grade trochlea dysplasia (Déjour types B-D) and 23 patients without trochlea dysplasia [7]. There were no significant group differences regarding clinical outcomes and failure rates after a mean follow-up of 3.7 years. Considering these findings and the rather high invasiveness of the procedure, it can be concluded that the indication for trochleoplasty in combination with cartilage repair at the patella should be set carefully and only in cases with severe patellofemoral instability.
Further identified risk factors for patellofemoral cartilage defects are valgus malalignment and increased femoral antetorsion [21]. However, among all 35 included studies there were no reports on varization or torsional osteotomies in combination with cartilage repair at the patella. Previous studies have demonstrated the efficiency of varization and torsional osteotomies to improve patellofemoral alignment in the field of patellofemoral instability and patellofemoral pain [34, 46, 66]. The clinical evidence of these procedures in combination with cartilage repair is yet to be investigated.
Studies which investigated representative study cohorts also including complex cases with the need for additional procedures showed good results after cartilage therapy at the patella. In comparison with the studies investigating isolated cartilage repair alone, results were similar at the final follow-up. Considering the fact that the mean preoperative scores were lower in the studies including combined procedures, the postoperative benefit may be even larger in this group.
A previous systematic review by Trinh et al. investigated the postoperative outcomes after ACI with or without additional patellofemoral osteotomy [70]. Based on 11 included studies, the authors found greater improvements in clinical scores after combined procedures, which supports the findings of the present systematic review.
This study, as all systematic reviews, has several limitations. First, there was a large heterogeneity of study designs, study qualities, patient population, outcome measurement instruments and data reporting across the included studies. Accordingly, a significant comparison of the individual results of studies with or without respecting co-pathologies such as patellofemoral and femoro-tibial malalignment is limited. Furthermore, due to a probably existing selection bias of included studies of patients treated with patellar chondral repair only, a careful interpretation of the results is required, not allowing for a deductive conclusion. Second, although the included studies reported an adequate overall mean follow-up of at least 50.2 months, the wide range of 24–153-month follow-up of the individual surveys may additionally limit the interpretation of the PROMs. Finally, as a cause of inconsistent documentation, long-term complications reported in some of the studies of this review could be considered.
Despite these limitations, the findings of this systematic review provide clinically relevant information. The results of the included studies demonstrate that the need for simultaneous correction of patellofemoral risk factors leads to similar clinical outcomes in comparison with isolated cartilage repair at the patella. An even larger benefit may be expected for patients with the need for additional procedures.
Conclusion
This study demonstrated good clinical outcomes after patellar cartilage repair with no evidence of worse results in complex cases with the need for additional patellofemoral realignment procedures. However, a meaningful statistical comparison between isolated patellar cartilage repair and combined co-procedures was not possible due to heterogeneous patient cohorts and a lack of analysis of specific subgroups in recent literature.
References
Ahrend MD, Eisenmann T, Herbst M, Gueorguiev B, Keller G, Schmidutz F et al (2021) Increased tibial tubercle-trochlear groove and patellar height indicate a higher risk of recurrent patellar dislocation following medial reefing. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06581-0
Akgün E, Akpolat AO (2019) Autologous osteochondral transplantation method of treatment for patellar osteochondral lesions. J Orthop Surg (Hong Kong) 27:2309499019851620
Ambra LF, Hinckel BB, Arendt EA, Farr J, Gomoll AH (2019) Anatomic risk factors for focal cartilage lesions in the patella and trochlea: a case-control study. Am J Sports Med 47:2444–2453
Arendt EA, Askenberger M, Agel J, Tompkins MA (2018) Risk of redislocation after primary patellar dislocation: a clinical prediction model based on magnetic resonance imaging variables. Am J Sports Med 46:3385–3390
Astur DC, Arliani GG, Binz M, Astur N, Kaleka CC, Amaro JT et al (2014) Autologous osteochondral transplantation for treating patellar chondral injuries: evaluation, treatment, and outcomes of a two-year follow-up study. J Bone Joint Surg Am 96:816–823
Astur DC, Bernardes A, Castro S, Arliani GG, Kaleka CC, Astur N et al (2017) Functional outcomes after patellar autologous osteochondral transplantation. Knee Surg Sports Traumatol Arthrosc 25:3084–3091
Barbieri Mestriner A, Ackermann J, Morlin Ambra LF, Franciozi CE, Faloppa F, Gomoll AH (2020) Trochlear dysplasia does not affect the outcomes of patellofemoral autologous chondrocyte implantation. Arthroscopy 36:3019–3027
Biant LC, Bentley G, Vijayan S, Skinner JA, Carrington RWJ (2014) Long-term results of autologous chondrocyte implantation in the knee for chronic chondral and osteochondral defects. Am J Sports Med 42:2178–2183
Bouwmeester PSJM, Kuijer R, Homminga GN, Bulstra SK, Geesink RGT (2002) A retrospective analysis of two independent prospective cartilage repair studies: autogenous perichondrial grafting: Versus subchondral drilling 10 years post-surgery. J Orthop Res 20:267–273
Brittberg M, Lindahl A, Nilsson A, Ohlsson C, Isaksson O, Peterson L (1994) Treatment of deep cartilage defects in the knee with autologous chondrocyte transplantation. N Engl J Med 331:889–895
Chadli L, Cottalorda J, Delpont M, Mazeau P, Thouvenin Y, Louahem D (2017) Autologous osteochondral mosaicplasty in osteochondritis dissecans of the patella in adolescents. Int Orthop 41:197–202
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum 52:2033–2039
Cohen M, Amaro JT, Fernandes Rde S, Arliani GG, Astur Dda C, Kaleka CC et al (2012) Osteochondral autologous transplantation for treating chondral lesions in the patella. Rev Bras Ortop 47:348–353
Diederichs G, Köhlitz T, Kornaropoulos E, Heller MO, Vollnberg B, Scheffler S (2013) Magnetic resonance imaging analysis of rotational alignment in patients with patellar dislocations. Am J Sports Med 41:51–57
Donoso R, Figueroa D, Espinoza J, Yañez C, Saavedra J (2019) Osteochondral autologous transplantation for treating patellar high-grade chondral defects: a systematic review. Orthop J Sports Med 7:2325967119876618
Familiari F, Cinque ME, Chahla J, Godin JA, Olesen ML, Moatshe G et al (2018) Clinical outcomes and failure rates of osteochondral allograft transplantation in the knee: a systematic review. Am J Sports Med 46:3541–3549
Farr J (2007) Autologous chondrocyte implantation improves patellofemoral cartilage treatment outcomes. Clin Orthop Relat Res 463:187–194
Figueroa D, Calvo Rodriguez R, Donoso R, Espinoza J, Vaisman A, Yañez C (2020) High-grade patellar chondral defects: promising results from management with osteochondral autografts. Orthop J Sports Med 8:2325967120933138
Figueroa D, Melean P, Calvo R, Gili F, Zilleruelo N, Vaisman A (2011) Osteochondral autografts in full thickness patella cartilage lesions. Knee 18:220–223
Filardo G, Kon E, Andriolo L, Di Martino A, Zaffagnini S, Marcacci M (2014) Treatment of “patellofemoral” cartilage lesions with matrix-assisted autologous chondrocyte transplantation: a comparison of patellar and trochlear lesions. Am J Sports Med 42:626–634
Flury A, Hoch A, Andronic O, Fritz B, Imhoff FB, Fucentese SF (2021) Increased femoral antetorsion correlates with higher degrees of lateral retropatellar cartilage degeneration, further accentuated in genu valgum. Knee Surg Sports Traumatol Arthrosc 29:1760–1768
Gaweda K, Walawski J, Wegłowski R, Drelich M, Mazurkiewicz T (2006) Early results of one-stage knee extensor realignment and autologous osteochondral grafting. Int Orthop 30:39–42
Gigante A, Enea D, Greco F, Bait C, Denti M, Schonhuber H et al (2009) Distal realignment and patellar autologous chondrocyte implantation: mid-term results in a selected population. Knee Surg Sports Traumatol Arthrosc 17:2–10
Gillogly SD, Arnold RM (2014) Autologous chondrocyte implantation and anteromedialization for isolated patellar articular cartilage lesions: 5 to 11 year follow-up. Am J Sports Med 42:912–920
Gobbi A, Chaurasia S, Karnatzikos G, Nakamura N (2015) Matrix-induced autologous chondrocyte implantation versus multipotent stem cells for the treatment of large patellofemoral chondral lesions: a nonrandomized prospective trial. Cartilage 6:82–97
Gobbi A, Kon E, Berruto M, Francisco R, Filardo G, Marcacci M (2006) Patellofemoral full-thickness chondral defects treated with Hyalograft-C: a clinical, arthroscopic, and histologic review. Am J Sports Med 34:1763–1773
Gomoll AH, Gillogly SD, Cole BJ, Farr J, Arnold R, Hussey K et al (2014) Autologous chondrocyte implantation in the patella: a multicenter experience. Am J Sports Med 42:1074–1081
Gracitelli GC, Meric G, Pulido PA, Görtz S, De Young AJ, Bugbee WD (2015) Fresh osteochondral allograft transplantation for isolated patellar cartilage injury. Am J Sports Med 43:879–884
Hangody L, Dobos J, Baló E, Pánics G, Hangody LR, Berkes I (2010) Clinical experiences with autologous osteochondral mosaicplasty in an athletic population: a 17 year prospective multicenter study. Am J Sports Med 38:1125–1133
Heir S, Nerhus TK, Røtterud JH, Løken S, Ekeland A, Engebretsen L et al (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38:231–237
Henderson IJ, Lavigne P (2006) Periosteal autologous chondrocyte implantation for patellar chondral defect in patients with normal and abnormal patellar tracking. Knee 13:274–279
Hinckel BB, Pratte EL, Baumann CA, Gowd AK, Farr J, Liu JN et al (2020) Patellofemoral cartilage restoration: a systematic review and meta-analysis of clinical outcomes. Am J Sports Med 48:1756–1772
Huntington LS, Webster KE, Devitt BM, Scanlon JP, Feller JA (2020) Factors associated with an increased risk of recurrence after a first-time patellar dislocation: a systematic review and meta-analysis. Am J Sports Med 48:2552–2562
Imhoff FB, Cotic M, Liska F, Dyrna FGE, Beitzel K, Imhoff AB et al (2019) Derotational osteotomy at the distal femur is effective to treat patients with patellar instability. Knee Surg Sports Traumatol Arthrosc 27:652–658
Joshi N, Reverte-Vinaixa M, Diaz-Ferreiro EW, Dominguez-Oronoz R (2012) Synthetic resorbable scaffolds for the treatment of isolated patellofemoral cartilage defects in young patients: magnetic resonance imaging and clinical evaluation. Am J Sports Med 40:1289–1295
Koh JL, Stewart C (2014) Patellar instability. Clin Sports Med 33:461–476
Kreuz PC, Müller S, Freymann U, Erggelet C, Niemeyer P, Kaps C et al (2011) Repair of focal cartilage defects with scaffold-assisted autologous chondrocyte grafts: clinical and biomechanical results 48 months after transplantation. Am J Sports Med 39:1697–1705
Kreuz PC, Steinwachs M, Erggelet C, Krause SJ, Ossendorf C, Maier D et al (2007) Classification of graft hypertrophy after autologous chondrocyte implantation of full-thickness chondral defects in the knee. Osteoarthr Cartil 15:1339–1347
Kusano T, Jakob RP, Gautier E, Magnussen RA, Hoogewoud H, Jacobi M (2012) Treatment of isolated chondral and osteochondral defects in the knee by autologous matrix-induced chondrogenesis (AMIC). Knee Surg Sports Traumatol Arthrosc 20:2109–2115
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100
Lording T, Lustig S, Servien E, Neyret P (2014) Chondral injury in patellofemoral instability. Cartilage 5:136–144
Macmull S, Jaiswal PK, Bentley G, Skinner JA, Carrington RW, Briggs TW (2012) The role of autologous chondrocyte implantation in the treatment of symptomatic chondromalacia patellae. Int Orthop 36:1371–1377
Macri EM, Felson DT, Ziegler ML, Cooke TDV, Guermazi A, Roemer FW et al (2019) The association of frontal plane alignment to MRI-defined worsening of patellofemoral osteoarthritis: the MOST study. Osteoarthr Cartil 27:459–467
Mehl J, Feucht MJ, Bode G, Dovi-Akue D, Südkamp NP, Niemeyer P (2016) Association between patellar cartilage defects and patellofemoral geometry: a matched-pair MRI comparison of patients with and without isolated patellar cartilage defects. Knee Surg Sports Traumatol Arthrosc 24:838–846
Minas T, Bryant T (2005) The role of autologous chondrocyte implantation in the patellofemoral joint. Clin Orthop Relat Res 436:30–39
Nelitz M, Dreyhaupt J, Williams SR, Dornacher D (2015) Combined supracondylar femoral derotation osteotomy and patellofemoral ligament reconstruction for recurrent patellar dislocation and severe femoral anteversion syndrome: surgical technique and clinical outcome. Int Orthop 39:2355–2362
Nho SJ, Foo LF, Green DM, Shindle MK, Warren RF, Wickiewicz TL et al (2008) Magnetic resonance imaging and clinical evaluation of patellar resurfacing with press-fit osteochondral autograft plugs. Am J Sports Med 36:1101–1109
Niemeyer P, Laute V, Zinser W, Becher C, Diehl P, Kolombe T et al (2020) Clinical outcome and success rates of ACI for cartilage defects of the patella: a subgroup analysis from a controlled randomized clinical phase II trial (CODIS study). Arch Orthop Trauma Surg 140:717–725
Niemeyer P, Steinwachs M, Erggelet C, Kreuz PC, Kraft N, Kostler W et al (2008) Autologous chondrocyte implantation for the treatment of retropatellar cartilage defects: clinical results referred to defect localisation. Arch Orthop Trauma Surg 128:1223–1231
Nomura E, Inoue M, Kurimura M (2003) Chondral and osteochondral injuries associated with acute patellar dislocation. Arthroscopy 19:717–721
Pachowsky ML, Trattnig S, Wondrasch B, Apprich S, Marlovits S, Mauerer A et al (2014) In vivo evaluation of biomechanical properties in the patellofemoral joint after matrix-associated autologous chondrocyte transplantation by means of quantitative T2 MRI. Knee Surg Sports Traumatol Arthrosc 22:1360–1369
Perdisa F, Filardo G, Sessa A, Busacca M, Zaffagnini S, Marcacci M et al (2017) One-step treatment for patellar cartilage defects with a cell-free osteochondral scaffold: a prospective clinical and MRI evaluation. Am J Sports Med 45:1581–1588
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med 30:2–12
Peterson L, Minas T, Brittberg M, Nilsson A, Sjögren-Jansson E, Lindahl A (2000) Two to 9 year outcome after autologous chondrocyte transplantation of the knee. Clin Orthop Relat Res 374:212–234
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38:1117–1124
Platt BN, Bowers LC, Magnuson JA, Marx SM, Liu JN, Farr J et al (2021) Return to sport after medial patellofemoral ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med. https://doi.org/10.1177/0363546521990004
Sadlik B, Puszkarz M, Kosmalska L, Wiewiorski M (2017) All-arthroscopic autologous matrix-induced chondrogenesis-aided repair of a patellar cartilage defect using dry arthroscopy and a retraction system. J Knee Surg 30:925–929
Seeley MA, Knesek M, Vanderhave KL (2013) Osteochondral injury after acute patellar dislocation in children and adolescents. J Pediatr Orthop 33:511–518
Sherman SL, Erickson BJ, Cvetanovich GL, Chalmers PN, Farr J 2nd, Bach BR Jr et al (2014) Tibial tuberosity osteotomy: indications, techniques, and outcomes. Am J Sports Med 42:2006–2017
Sherman SL, Humpherys J, Farr J (2019) Optimizing patellofemoral cartilage restoration and instability with tibial tubercle osteotomy. Arthroscopy 35:2255–2256
Singhal R, Rogers S, Charalambous CP (2013) Double-bundle medial patellofemoral ligament reconstruction with hamstring tendon autograft and mediolateral patellar tunnel fixation: a meta-analysis of outcomes and complications. Bone Joint J 95-b:900–905
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73:712–716
Solheim E, Hegna J, Inderhaug E (2018) Early determinants of long-term clinical outcome after cartilage repair surgery in the knee. J Orthop 15:222–225
Spahn G, Hofmann GO (2014) Focal cartilage defects within the medial knee compartment. predictors for osteoarthritis progression. Z Orthop Unfall 152:480–488
Spahn G, Kirschbaum S (2005) Operative treatment of deep chondral defects of the patella: results after abrasive arthroplasty and periosteal arthroplasty. Knee Surg Sports Traumatol Arthrosc 13:352–356
Stambough JB, Davis L, Szymanski DA, Smith JC, Schoenecker PL, Gordon JE (2018) Knee pain and activity outcomes after femoral derotation osteotomy for excessive femoral anteversion. J Pediatr Orthop 38:503–509
Su CA, Trivedi NN, Le HT, Sivasundaram L, Maak TG, Salata MJ et al (2021) Clinical and radiographic outcomes after treatment of patellar chondral defects: a systematic review. Sports Health 13:490–501
Sumida Y, Nakamura K, Feil S, Siebold M, Kirsch J, Siebold R (2021) Good healing potential of patellar chondral defects after all-arthroscopic autologous chondrocyte implantation with spheroids: a second-look arthroscopic assessment. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-00021-06584-x
Teo BJ, Buhary K, Tai BC, Hui JH (2013) Cell-based therapy improves function in adolescents and young adults with patellar osteochondritis dissecans. Clin Orthop Relat Res 471:1152–1158
Trinh TQ, Harris JD, Siston RA, Flanigan DC (2013) Improved outcomes with combined autologous chondrocyte implantation and patellofemoral osteotomy versus isolated autologous chondrocyte implantation. Arthroscopy 29:566–574
Uimonen M, Ponkilainen V, Hirvinen S, Mattila VM, Kask G, Nurmi H et al (2021) The risk of osteochondral fracture after patellar dislocation is related to patellofemoral anatomy. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06547-2
Uimonen MM, Repo JP, Huttunen TT, Nurmi H, Mattila VM, Paloneva J (2021) Surgery for patellar dislocation has evolved towards anatomical reconstructions with assessment and treatment of anatomical risk factors. Knee Surg Sports Traumatol Arthrosc 29:1944–1951
Visonà E, Chouteau J, Aldegheri R, Fessy MH, Moyen B (2010) Patella osteochondritis dissecans end stage: the osteochondral mosaicplasty option. Orthop Traumatol Surg Res 96:543–548
von Keudell A, Han R, Bryant T, Minas T (2017) Autologous chondrocyte implantation to isolated patella cartilage defects. Cartilage 8:146–154
Waltenspül M, Suter C, Ackermann J, Kühne N, Fucentese SF (2021) Autologous matrix-induced chondrogenesis (AMIC) for isolated retropatellar cartilage lesions: outcome after a follow-up of minimum 2 years. Cartilage. https://doi.org/10.1177/19476035211021908
Yonetani Y, Tanaka Y, Kanamoto T, Nakamura N, Nakata K, Horibe S (2019) Autologous osteochondral transplantation in full-thickness patella chondral lesion: a case series. J Orthop Case Rep 9:53–57
Funding
Open Access funding enabled and organized by Projekt DEAL. There was no funding for the present study.
Author information
Authors and Affiliations
Contributions
All authors contributed to the conception and design of the study. DB and JM were responsible for the identification and screening of the literature. All authors contributed to the assessment of eligibility of the included studies as well as to the analysis and interpretation of the extracted data. The article was primarily drafted by DB and JM. All authors contributed to internal reviews of the manuscript and the final version was approved by all authors.
Corresponding author
Ethics declarations
Conflict of interest
All authors confirm that they do not have any conflicts of interest regarding the present study.
Ethical approval
Ethical approval was not necessary as this was a systematic review of previously published literature.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Burger, D., Feucht, M., Muench, L.N. et al. Good clinical outcomes after patellar cartilage repair with no evidence for inferior results in complex cases with the need for additional patellofemoral realignment procedures: a systematic review. Knee Surg Sports Traumatol Arthrosc 30, 1752–1768 (2022). https://doi.org/10.1007/s00167-021-06728-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06728-z