Abstract
Purpose
Glenoid bone integrity is crucial for shoulder stability. The purpose of this study was to investigate a non-invasive method for quantifying bone loss regarding reliability and accuracy to detect glenoid bone deficiency in standard two-dimensional (2D) and three-dimensional (3D) computed tomography (CT) measurements at different time points. It was hypothesized that the diameter of the circle used would significantly differ between raters, rendering this method inaccurate and not allowing for an exact estimation of glenoid defect size.
Methods
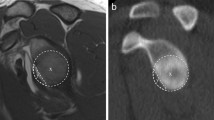
Fifty-two shoulder CTs from 26 patients (26 2D-CTs; 26 3D-CTs) with anterior glenoid bone defects were evaluated by 6 raters at time 0 (T0) and at least 3 weeks after (T1) to assess the glenoid bone defect using the ratio method (“best fit circle”). Inter- and intra-rater differences concerning circle dimensions (circle diameter), measured width of bone loss and calculated percentage of bone loss (length-width-ratio) were compared in 2D- versus 3D-CT scans. The intraclass coefficient (ICC) was used to determine the inter- and intra-rater agreement.
Results
The mean circle diameter difference in 2D-CT was 2.0 ± 1.9 mm versus 1.8 ± 1.5 mm in 3D-CT, respectively (p < 0.01). Mean width of bone loss in 2D-CT was 1.9 ± 1.7 mm compared to 1.7 ± 1.5 mm in 3D-CT, respectively (p < 0.01). The mean difference of bone loss percentage was 5.1 ± 4.8% in 2D-CT and 4.8 ± 4.5% in 3D-CT (p < 0.01). No significant differences concerning circle diameter, bone loss width and bone loss percentage were detected comparing T0 and T1. Circle diameter, bone loss width and bone loss percentage measurements in 3D-CT were significantly smaller compared to 2D-CT at T0 and T1 (p < 0.01). Agreement (ICC) was fair to good for all indicators of circle diameter (range 0.76–0.83), bone loss width (range 0.76–0.86) and percentage of bone loss (range 0.85–0.91). Overall, 3D-CT showed superior agreement compared to 2D-CT.
Conclusion
The ratio method varies in all glenoid parameters and is not valid for consistently quantifying glenoid bone defects even in 3D computed tomography. This must be taken into consideration when determining proper surgical treatment. The degree of glenoid bone loss alone should not be used to decide for or against a bony procedure. Rather, it is more important to define a defect size as “critical” and to also take other patient-specific factors into consideration so that the best treatment option can be undertaken. Application of the “best fitting circle” is a source of error when using the ratio method; therefore, care should be taken when measuring the circle diameter.
Level of evidence
III.


Similar content being viewed by others
References
Bishop JY, Jones GL, Rerko MA, Donaldson C, Group MS (2013) 3-D CT is the most reliable imaging modality when quantifying glenoid bone loss. Clin Orthop Relat Res 471:1251–1256
Boileau P, Villalba M, Hery JY, Balg F, Ahrens P, Neyton L (2006) Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Jt Surg Am 88:1755–1763
Bois AJ, Fening SD, Polster J, Jones MH, Miniaci A (2012) Quantifying glenoid bone loss in anterior shoulder instability: reliability and accuracy of 2-dimensional and 3-dimensional computed tomography measurement techniques. Am J Sports Med 40:2569–2577
Burkhart SS, De Beer JF (2000) Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill–Sachs lesion. Arthroscopy 16:677–694
Chuang TY, Adams CR, Burkhart SS (2008) Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthroscopy 24:376–382
Edwards TB, Boulahia A, Walch G (2003) Radiographic analysis of bone defects in chronic anterior shoulder instability. Arthroscopy 19:732–739
Frank RM, Golijanin P, Vopat BG, Gross DJ, Chauhan V, Romeo AA et al (2018) Impact of sagittal rotation on axial glenoid width measurement in the setting of glenoid bone loss. Am J Orthop (Belle Mead NJ) 47:6
Gerber C, Nyffeler RW (2002) Classification of glenohumeral joint instability. Clin Orthop Relat Res 400:65–76
Griffith JF, Antonio GE, Tong CW, Ming CK (2003) Anterior shoulder dislocation: quantification of glenoid bone loss with CT. AJR Am J Roentgenol 180:1423–1430
Griffith JF, Antonio GE, Yung PS, Wong EM, Yu AB, Ahuja AT et al (2008) Prevalence, pattern, and spectrum of glenoid bone loss in anterior shoulder dislocation: CT analysis of 218 patients. AJR Am J Roentgenol 190:1247–1254
Gross DJ, Golijanin P, Dumont GD, Parada SA, Vopat BG, Reinert SE et al (2016) The effect of sagittal rotation of the glenoid on axial glenoid width and glenoid version in computed tomography scan imaging. J Shoulder Elbow Surg 25:61–68
Itoi E, Lee SB, Berglund LJ, Berge LL, An KN (2000) The effect of a glenoid defect on anteroinferior stability of the shoulder after Bankart repair: a cadaveric study. J Bone Jt Surg Am 82:35–46
Kubicka AM, Stefaniak J, Lubiatowski P, Dlugosz J, Dzianach M, Redman M et al (2016) Reliability of measurements performed on two dimensional and three dimensional computed tomography in glenoid assessment for instability. Int Orthop 40:2581–2588
Lacheta L, Siebenlist S, Imhoff AB, Willinger L (2018) Recurrent instability and instability arthropathy. Unfallchirurg 121:142–151
Lo IK, Burkhart SS (2004) Arthroscopic revision of failed rotator cuff repairs: technique and results. Arthroscopy 20:250–267
Mologne TS, Provencher MT, Menzel KA, Vachon TA, Dewing CB (2007) Arthroscopic stabilization in patients with an inverted pear glenoid: results in patients with bone loss of the anterior glenoid. Am J Sports Med 35:1276–1283
Parada SA, Eichinger JK, Dumont GD, Parada CA, Greenhouse AR, Provencher MT et al (2018) Accuracy and reliability of a simple calculation for measuring glenoid bone loss on 3-dimensional computed tomography scans. Arthroscopy 34:84–92
Porcellini G, Campi F, Paladini P (2002) Arthroscopic approach to acute bony Bankart lesion. Arthroscopy 18:764–769
Provencher MT, Bhatia S, Ghodadra NS, Grumet RC, Bach BR Jr, Dewing CB et al (2010) Recurrent shoulder instability: current concepts for evaluation and management of glenoid bone loss. J Bone Jt Surg Am 92(Suppl 2):133–151
Rerko MA, Pan X, Donaldson C, Jones GL, Bishop JY (2013) Comparison of various imaging techniques to quantify glenoid bone loss in shoulder instability. J Shoulder Elbow Surg 22:528–534
Shaha JS, Cook JB, Song DJ, Rowles DJ, Bottoni CR, Shaha SH et al (2015) Redefining “critical” bone loss in shoulder instability: functional outcomes worsen with “subcritical” bone loss. Am J Sports Med 43:1719–1725
Sugaya H, Moriishi J, Dohi M, Kon Y, Tsuchiya A (2003) Glenoid rim morphology in recurrent anterior glenohumeral instability. J Bone Jt Surg Am 03(Suppl 85):878–884
Sugaya H (2014) Techniques to evaluate glenoid bone loss. Curr Rev Musculoskelet Med 7:1–5
Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A (2005) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J Bone Jt Surg Am 87:1752–1760
Sugaya H, Moriishi J, Kanisawa I, Tsuchiya A (2006) Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. Surgical technique. J Bone Jt Surg Am 88(Suppl 1 Pt 2):159–169
Yamamoto N, Itoi E, Abe H, Kikuchi K, Seki N, Minagawa H et al (2009) Effect of an anterior glenoid defect on anterior shoulder stability: a cadaveric study. Am J Sports Med 37:949–954
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Frank Martetschläger and Sepp Braun have received consulting fees from Arthrex. Andreas Imhoff has received consulting fees from Arthrex, Arthrosurface and Medi Bayreuth. Peter J. Millett has received consulting fees from Arthrex, Medbridge, Springer Publishing and royalties from Arthrex. Peter J. Millett has stock options in VuMedi and GameReady. Research activities at Steadman Philippon Research Institute are supported by Vail Valley Medical Center and corporate sponsorships by Smith&Nephew, Arthrex, Siemens and Össur. Elmar Herbst, Andreas Voss, Pia Jungmann and Lucca Lacheta declare no conflict of interests.
Ethical approval
The study is in accordance with the institutional ethic guidelines and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lacheta, L., Herbst, E., Voss, A. et al. Insufficient consensus regarding circle size and bone loss width using the ratio—“best fit circle”—method even with three-dimensional computed tomography. Knee Surg Sports Traumatol Arthrosc 27, 3222–3229 (2019). https://doi.org/10.1007/s00167-019-05391-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05391-9