Abstract
Purpose
Optimal oxygenation targets for patients with acute hypoxemic respiratory failure in the intensive care unit (ICU) are not clearly defined due to substantial variability in design of previous trials. This study aimed to perform a pre-specified individual patient data meta-analysis of the Handling Oxygenation Targets in the ICU (HOT-ICU) and the Handling Oxygenation Targets in coronavirus disease 2019 (COVID-19) (HOT-COVID) trials to compare targeting a partial pressure of arterial oxygen (PaO2) of 8–12 kPa in adult ICU patients, assessing both benefits and harms.
Methods
We assessed 90-day all-cause mortality and days alive without life support in 90 days using a generalised mixed model. Heterogeneity of treatment effects (HTE) was evaluated in 14 subgroups, and results graded using the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN).
Results
At 90 days, mortality was 40.4% (724/1792) in the 8 kPa group and 40.9% (733/1793) in the 12 kPa group (risk ratio, 0.99; 95% confidence interval [CI] 0.92–1.07; P = 0.80). No difference was observed in number of days alive without life support. Subgroup analyses indicated more days alive without life support in COVID-19 patients targeting 8 kPa (P = 0.04) (moderate credibility), and lower mortality (P = 0.03) and more days alive without life support (P = 0.02) in cancer-patients targeting 12 kPa (low credibility).
Conclusion
This study reported no overall differences comparing a PaO2 target of 8–12 kPa on mortality or days alive without life support in 90 days. Subgroup analyses suggested HTE in patients with COVID-19 (moderate credibility) and cancer (low credibility).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
In this individual patient data meta-analysis of the HOT-ICU and HOT-COVID trials, no overall difference was observed in mortality or days alive without life support when comparing a lower oxygenation target (8 kPa PaO2) with a higher oxygenation target (12 kPa PaO2). Subgroup analyses suggested a benefit of the lower oxygenation target on days alive without life support in patients with coronavirus disease 2019 (moderate credibility) and of the higher oxygenation target on mortality and days alive without life support in patients with cancer (low credibility). |
Introduction
Oxygen therapy is an essential part of care for patients admitted to the intensive care unit (ICU) with acute hypoxemic respiratory failure, but should be administered at levels that provide adequate supply for the body while avoiding the risks associated with both excessively high and low levels [1]. Currently, there is no consensus on the optimal oxygen level for ICU patients, and guidelines offer only general recommendations [2,3,4]. A significant challenge in determining the ideal oxygenation strategy for ICU patients is the large variation in study design, study populations, and definitions of oxygenation targets across conducted clinical trials, where 'low' target levels in some trials overlap with 'high' target levels in others [5,6,7,8,9,10,11,12]. These differences make it difficult to aggregate data into precise and reliable estimates of the treatment effects, which is crucial for informing clinical practice [13, 14]. This problem is exemplified by the recently updated Cochrane review comparing higher versus lower oxygenation strategies in the ICU [15]. Despite identifying 19 trials, the review found no significant difference in mortality and assessed the certainty of evidence for this outcome as ‘very low’. The downgrading was primarily attributed to bias due to indirectness caused by the variations in interventions and patient demographics between the trials.
We have chosen a focused approach, conducting an individual patient data meta-analysis (IPDMA) of two recent trials with considerable overlap in inclusion and exclusion criteria, common trial sites and identical interventions: the Handling Oxygenation Targets in the ICU (HOT-ICU) trial and the Handling Oxygenation Targets in coronavirus disease 2019 (COVID-19) (HOT-COVID) trial [5, 16]. These trials were specifically selected, because they were conducted under the same trial protocol and shared trial sites, interventions, outcomes, and the inclusion of ICU patients with acute hypoxemic respiratory failure [17, 18]. This allowed us to assess the effects of the identical interventions with more precision, and to assess heterogeneity of intervention effects in clinically important patient subgroups.
The aim of the present IPDMA was to assess the effects of targeting a partial pressure of arterial oxygen (PaO2) of 8 kPa versus a PaO2 of 12 kPa on all-cause mortality and days alive without life support in 90 days in ICU patients with acute respiratory failure, both overall and in pre-specified subgroups. We hypothesised that targeting a PaO2 of 8 kPa would result in lower all-cause mortality and increased days alive without life support at 90 days, in comparison to a target PaO2 of 12 kPa. This hypothesis is based on the potential deleterious effects of hyperoxaemia in ICU patients [19].
Methods
Study design and oversight
This IPDMA of the HOT-ICU and HOT-COVID trials was conducted in accordance with the protocol published before inclusion of the last patient in the HOT-COVID trial [20]. Any deviations from the protocol are explicitly stated in the electronic supplementary material (ESM) 2. The results are presented in accordance with the Preferred Reporting Items for a Systematic Review and Meta-Analysis of Individual Participant Data (PRISMA-IPD) [21]. The PRISMA-IPD checklist is presented in the ESM 1 (eTable 1).
The HOT-ICU and HOT-COVID trials were investigator-initiated, multi-centre, parallel-group, randomised clinical trials. Both utilised centralised randomisation with computer-generated concealed assignment sequences in permuted blocks of varying sizes with the HOT-ICU trail being stratified for trial site, chronic obstructive pulmonary disease (COPD), and active haematological cancer, and the HOT-COVID trial being stratified for trial site. For both, detailed protocols and statistical analysis plans were published prior to trial completion [17, 18, 22].
The HOT-ICU trial was conducted from June 20, 2017, to August 3, 2020, and randomised 2928 patients [5]. The HOT-COVID trial was conducted from August 25, 2020, to March 8, 2023, and randomised 726 of a planned 780 patients; it was stopped early, prior to assessment of trial results [16], due to slow recruitment. No patients were randomised into both trials. Both trials were approved by the Danish Health and Medicines Agency, the Health Research Ethics Committee in the North Denmark Region, the Danish Data Protection Agency, and by all required authorities in participating countries, and were prospectively registered at ClinicalTrials.gov (NCT03174002 and NCT04425031).
Participants
Both trials included adult patients (≥ 18 years of age) admitted to an ICU with acute hypoxemic respiratory failure. At randomisation, patients received supplemental oxygen either through an open system with a flow rate of at least 10 L per minute, or through a closed system with HOT-ICU requiring a minimum fraction of inspired oxygen (FiO2) of 0.50, while HOT-COVID allowed any FiO2. Patients were expected to receive supplemental oxygen for at least 24 h in the ICU and were required to have a functioning arterial line for frequent PaO2 monitoring. Arterial lines are considered standard of care for patients admitted to the ICU with acute hypoxemic respiratory failure in all participating countries. The two trials differed only in HOT-COVID mandating a verified Severe Acute Respiratory Syndrome COronaVirus 2 (SARS-CoV-2) infection at randomisation [17, 18]. Full lists of inclusion and exclusion criteria for both trials are provided in the ESM 1.
Intervention
In both trials, patients were randomised 1:1 to receive supplemental oxygen targeting a PaO2 of either 8 kPa (Lower Oxygenation Group) or 12 kPa (Higher Oxygenation Group). The intervention was administered throughout the entire ICU stay, including any readmissions, for up to 90 days after randomisation. PaO2 levels were achieved via titration of administered FiO2 based on intermittent arterial blood gas analyses correlated to the continuous measurement of peripheral oxygen saturation.
Outcomes
The primary outcome was 90-day all-cause mortality. The secondary outcome was the absolute number of days alive without life support in 90 days from randomisation. Life support was defined as any use of either mechanical ventilation, vasopressor or inotropic support, or renal replacement therapy. Details are provided in the ESM 1.
Subgroups
The intervention effects on the primary and secondary outcome were assessed in a total of 14 subgroups according to the follow baseline characteristics; age, sex, admission type (medical, elective surgical, or emergency surgical), ventilatory support [invasive mechanical ventilation, non-invasive ventilation or continuous positive airway pressure (CPAP), or open systems], COPD, pneumonia, intracranial pathology (traumatic brain injury, haemorrhagic or ischaemic stroke, and patients resuscitated from cardiac arrest), heart disease (ischaemic heart disease, chronic heart failure, and acute myocardial infarction), chronic dialysis, intestinal ischaemia, cancer (active haematological cancer and metastatic cancer), shock (plasma lactate > 2 mmol/L and use of continuous vasopressor or inotropes), COVID-19, and in patients receiving mechanical ventilation according to their PaO2/FiO2 ratio [20]. The expected direction of the intervention effect is presented both in the protocol [20] and in ESM 1 (eTable 2). The credibility of the effect modifications in the subgroup analyses was estimated using the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) tool [23]. A total of eight mandatory domains and one optional were considered, and the overall credibility of the proposed effect modification was ranked as ‘very low’, ‘low’, ‘moderate’, or ‘high’. Subgroups with a p value for interaction below 0.10 were graded with ICEMAN in accordance with the guidelines for this instrument requiring that all outcomes with a potential interaction are assessed [23]; nevertheless, only subgroup interactions with a p value below 0.05 were considered statistically significant to provide a conservative interpretation of subgroup results given the risk of chance findings [20]. Details on baseline characteristics, outcome definitions, and ICEMAN are provided in the ESM 1.
Statistical analyses
All analyses were conducted in the intention-to-treat population, being all randomised patients, except for those where follow-up data could not be obtained due to withdrawn or unobtainable consent according to national regulations. All tests for statistical significance were two-sided, with alpha levels set at 0.05. Subgroup analyses are reported with 95% confidence intervals (CIs) and p values for the test of interaction. No adjustments for multiplicity were conducted in the primary analyses [20]. Given the risk of multiplicity, we post hoc included sensitivity analyses in which we adjusted the subgroup analyses for multiplicity ad modum Jakobsen et al. [24].
Individual patient data from both trials were appended in a one-step approach using a Generalised Linear Mixed Model (GLMM) allowing for fixed slopes and random intercepts and robust variance estimation [25, 26]. Data were organised into clusters according to trial and site levels with the intercepts being allowed to vary in all clusters. The fixed slopes assume a uniform effect of the oxygenation targets across all clusters, assuming a consistent physiological impact of the intervention irrespective of trial or site locations. Random intercepts permit variations in baseline outcome levels among clusters, thus accounting for differences in patient demographics or other factors unrelated to the intervention. We treated sites participating in both trials as separate clusters for each trial [17, 18, 20]. Trial-specific stratification variables were retained (eFigure 1).
The primary outcome was analysed using a GLMM Poisson family with a log-link, and the secondary outcome using a GLMM Gaussian family with an identity link. Sensitivity analyses with adjustment for the trial-specific stratification variables COPD and active haematological cancer, and the clinically important baseline factors age, metastatic cancer, admission type, and sequential organ failure assessment (SOFA) score were performed for both the primary and the secondary outcome. We supplemented the analysis of the primary outcome with Kaplan–Meier plots. Subgroup heterogeneity of treatment effects (HTE) analyses for the primary and the secondary outcomes were performed using a generalised linear model with fixed slopes, and robust cluster variance estimation, while retaining data clustering as in the primary analyses. Further, we assessed HTE between the two trials for the primary and the secondary outcomes in supplemental post hoc interaction analyses. These tests used the trial (HOT-ICU or HOT-COVID) and the intervention group as interaction terms. No imputations for missing data were conducted since the percentage of missing data for all variables and outcomes in any analysis was less than the pre-specified 5% cut-off level necessitating this (ESM 1) [20]. All analyses were conducted using Stata statistical software release 18 (StataNordic).
Results
Participant characteristics
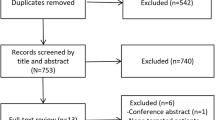
A total of 3654 patients from 35 ICUs across Denmark, Switzerland, Finland, The Netherlands, Norway, the United Kingdom, and Iceland were enrolled in two trials: 2928 patients (80.1%) in the HOT-ICU trial and 726 (19.9%) in the HOT-COVID trial, with a total of 1827 patients in the Lower Oxygenation Group and 1827 patients in the Higher Oxygenation Group. For the primary outcome of 90-day mortality, data were available for 3585 patients (98.1%): 2888 from the HOT-ICU and 697 from the HOT-COVID trial, with 1792 patients in the Lower Oxygenation Group and 1793 patients in the Higher Oxygenation Group. For the secondary outcome of days alive without life support in 90 days, data were available for 3575 patients (97.4%): 2878 from the HOT-ICU and 697 from the HOT-COVID trial, with 1786 patients in the Lower Oxygenation Group and 1789 patients in the Higher Oxygenation Group.
Baseline characteristics were similar between the two oxygenation groups, except for the presence of cardiac arrest and the end-expiratory pressure in invasively mechanically ventilated patients (Table 1). When comparing the trials, included patients differed in all baseline characteristics except for positive end-expiratory pressure (PEEP) in patients receiving non-invasive ventilation or CPAP, and in the proportion on long-term dialysis. Complete data are available in the ESM 1 (eTable 3).
Oxygenation and ICU interventions
The median recorded PaO2, with corresponding arterial oxygen saturation (SaO2) and FiO2, in the ICU were all lower in the Lower Oxygenation Group than in the Higher Oxygenation Group throughout the 90-day intervention period (Fig. 1). Details on ICU treatments, including use of mechanical ventilation, prone positioning, inhaled vasodilators, extracorporeal membrane oxygenation, circulatory support, renal replacement therapy, blood transfusions, and ventilator settings (positive end-expiratory pressure, peak inspiratory pressure, and tidal volume) are provided in the ESM 1 (eTable 4). In the HOT-COVID trial, more patients were treated with proning, inhaled vasodilators, and extracorporeal membrane oxygenation, but less received vasopressors or inotropes, renal replacement therapy, and red blood cell transfusions compared to patients in the HOT-ICU trial (ESM 1, eTable 5).
Values for PaO2, SaO2, and FiO2, according to oxygenation strategy. Shown are the median values of daily means of arterial partial pressure of oxygen (PaO2) (Panel A), arterial oxygen saturation (SaO2) (Panel B), and fraction of inspired oxygen (FiO2) (Panel C). The daily means were calculated from the 12-h lowest and highest PaO2 with concomitant values for SaO2 and FiO2. Bars represent interquartile ranges (IQR). SaO2 values were not available in blood gas analyses from one site in the HOT-ICU trial and were therefore missing for 191 patients. Data on the number of patients contributing with data per day are provided in the ESM 1, eTable 6
Primary outcome
At 90 days after randomisation, a total of 724 of 1792 patients (40.4%) in the Lower Oxygenation Group and 733 of 1793 patients (40.9%) in the Higher Oxygenation Group had died (adjusted risk ratio, 0.99; 95% CI, 0.92–1.07; P = 0.80) (Figs. 2 and 3). Additional adjustment for baseline factors in the sensitivity analysis produced similar results (Fig. 2). The post hoc analysis of HTE between the trials showed no significant interaction with a p value of 0.12.
90-Day all-cause mortality including patient subgroups. All analyses were adjusted for trial-specific stratification variables: haematological cancer, COPD, and trial site in the HOT-ICU trial; trial site in the HOT-COVID trial. The p value for interaction represents the tests for interaction for each subgroup. IMV invasive mechanical ventilation, NIV non-invasive ventilation, CPAP continuous positive airway pressure, COPD chronic obstructive pulmonary disease, COVID-19 coronavirus disease 2019, PaO2 arterial partial pressure of oxygen, FiO2 fraction of inspired oxygen. *Adjusted for both trial-specific stratification variables and the baseline variables age, admission type, presence or absence of metastatic cancer, presence or absence of chronic obstructive pulmonary disease, presence or absence of haematological cancer, and the sequential organ failure assessment score, which ranges from 0 to 24 with higher scores indicating more severe organ failure. aMedian age was 69 years. bOnly patients receiving invasive ventilation, non-invasive ventilation, or continuous positive airway pressure at baseline were included
Secondary outcome
The Lower Oxygenation Group had a median of 75 days (interquartile range (IQR) 1–87 days) alive without life support in 90 days after randomisation compared to 70 days (IQR 1–86 days) in the Higher Oxygenation Group (adjusted mean difference, 1.5 days; 95% CI – 0.7 to 3.7 days; P = 0.27) (Fig. 4 and eFigure 2). Additional adjustment for baseline factors in the sensitivity analysis produced similar results (Fig. 4). The post hoc analysis of HTE between the trials showed a significant interaction with a P value of 0.04.
Days alive without life support including patient subgroups. Days alive without life support is defined as the absolute number of days alive without the use of invasive ventilation, non-invasive ventilation, non-intermittent continuous positive airway pressure, vasopressor or inotropic infusion, or any renal replacement therapy in 90 days after randomisation. The p value for interaction represents the tests for interaction for each subgroup. All analyses were adjusted for trial-specific stratification variables: haematological cancer, COPD, and trial site in the HOT-ICU trial; trial site in the HOT-COVID trial. IMV invasive mechanical ventilation, NIV non-invasive ventilation, CPAP continuous positive airway pressure, COPD chronic obstructive pulmonary disease, COVID-19 Coronavirus disease 2019, PaO2 arterial partial pressure of oxygen, and FiO2 fraction of inspired oxygen. *Adjusted for both trial-specific stratification variables and the baseline variables age, admission type, presence or absence of metastatic cancer, presence or absence of chronic obstructive pulmonary disease, presence or absence of haematological cancer, and the sequential organ failure assessment score, which ranges from 0 to 24 with higher scores indicating more severe organ failure. aMedian age was 69 years. bOnly patients receiving invasive ventilation, non-invasive ventilation, or continuous positive airway pressure at baseline were included.
Subgroup analyses
In the HTE analyses of 14 subgroups, significant interactions with the intervention were identified in patients with cancer and patients with COVID-19 (Figs. 2 and 4).
In patients with cancer at baseline, we observed a suggested increase in mortality in the Lower Oxygenation Group (P = 0.03), and more days alive without life support for patients in the Higher Oxygenation Group (P = 0.02).
In patients with COVID-19, we observed a suggested increase in the number of days alive without life support for patients in the Lower Oxygenation Group (P = 0.04).
The ICEMAN credibility assessments rated the effect modification for patients with COVID-19 at baseline, as ‘moderate’. The credibility of effect modification was graded as ‘low’ for both outcomes in patients with cancer. Comprehensive gradings are available in the ESM 1. Post hoc sensitivity analyses of all subgroups with multiplicity adjustment are provided in the ESM 1, eTable 8 and 9.
Discussion
This IPDMA was conducted to investigate the benefits and harms of targeting a PaO2 of 8 kPa compared to 12 kPa in ICU patients with acute hypoxemic respiratory failure. We combined individual patient data from two clinical trials based on the same protocol, enhancing statistical power, and enabling a more detailed investigation with minimal bias due to indirectness. Overall, we found no effects on mortality or number of days alive without life support in 90 days. Subgroup analyses suggested more days alive without life support in patients with COVID-19 targeted at 8 kPa (moderate credibility). Conversely, patients with cancer had higher mortality at a target of 8 kPa and more days alive without life support at a target of 12 kPa (low credibility).
The COVID-19 subgroup analysis reinforces the main findings of the HOT-COVID trial [16], showing an increase in the number of days alive without life support for patients targeted to a PaO2 of 8 kPa. Among trials focusing on targeted oxygenation in the ICU, only three have included COVID-19 patients: 110 patients in the HOT-ICU trial [27], 19 patients in the ICONIC trial [28], and 726 patients in the HOT-COVID trial [16]. However, the ICONIC trial did not report outcomes for this specific subgroup. Consequently, by combining data from the HOT-ICU and HOT-COVID trials, this subgroup analysis represents all currently published evidence on targeted oxygen therapy for COVID-19 patients in the ICU. The observed intervention effect might stem from a more homogeneous patient population with a shared respiratory failure cause. From a biological perspective, the distinct pathophysiology of COVID-19 pneumonia [29] with endotheliopathy [30], damage to lung cells [30, 31], and potentially lower levels of antioxidants [32, 33] could have led to increased lung tissue damage due to oxygen toxicity in patients exposed to higher levels of supplemental oxygen [34].
The observed modification of the intervention effect on both outcomes for patients with cancer at baseline aligns with the results from the subgroup analysis of patients with haematological malignancy at baseline in the HOT-ICU trial [35], but contrasts with the pre-specified expected direction of the intervention effect [20]. Although hypoxia plays a pivotal role in cancer growth [36], the current evidence on the benefit of oxygen therapy in cancer treatment is inconclusive [37], and the findings should be interpreted cautiously.
Differences in baseline characteristics were evident between the two trials. Patients in the HOT-ICU trial were older, had higher SOFA scores, more comorbidities, and a higher proportion received invasive mechanical ventilation at baseline, while patients in the HOT-COVID trial were younger and primarily presented with pulmonary single-organ failure due to COVID-19. Post hoc analyses showed no significant HTE between the two trials for the primary outcome of 90-day all-cause mortality. However, significant HTE was found for days alive without life support, indicating that baseline differences or differences in treatment received in the two trials have affected the effects of the intervention on this outcome. Importantly, all patients in both trials had acute hypoxemic respiratory failure mandating supplemental oxygen in an ICU setting at randomisation. These trial-level differences underscore that we cannot treat the pooled data as independent of the trial it was part of, which highlights the importance of using a clustered mixed model [38]. This approach provides a high degree of statistical power to assess both the overall intervention effect and subgroup HTE, while considering both between-trial and within-trial differences that might lead to varying rates of baseline mortality or days alive without life support [39, 40].
The overall findings of this IPDMA are consistent with the latest published comprehensive meta-analysis on randomised trials on lower versus higher oxygenation strategies in ICU patients [15]. Further, it highlights that using a lower oxygenation target of 8 kPa is safe for most ICU patients which aligns with the newest clinical recommendations [4]. While the observed heterogeneity of treatment effects for patients with cancer and that for patients with COVID-19 suggest the existence of patient subgroups that may benefit from specific oxygen levels [41], and highlights the still poorly understood pathophysiological mechanisms involved in acute respiratory distress syndrome [42, 43], it is important to underscore that these subgroup findings needs to confirmed in independent trials [44, 45].
Strengths and limitations
The strengths of the current individual patient data meta-analysis include the publication of the protocol prior to inclusion of the last patient in the HOT-COVID trial, and methodology consistent with previously conducted patient-level meta-analyses in critically ill patients [46,47,48].
In addition, the inclusion of a large ICU population with acute hypoxemic respiratory failure, identical trial protocols for oxygenation targeting, recruitment from a sizeable number of ICUs in several countries, and the use of an endorsed tool for the evaluation of credibility in effect modification analyses [23, 49], all add to the external validity of the findings.
Limitations of the study include the lack of multiplicity adjustments, which especially in the subgroup analyses increases the risk of false positive findings. The results should therefore be interpreted cautiously and only as hypothesis-generating, a fact which is underlined by the results of the post hoc multiplicity-adjusted subgroup analyses. The decision not to multiplicity-adjust the primary analyses was made to avoid deflation of the study-wide alpha level, thus addressing a general null hypothesis rather than the specific null hypotheses for each subgroup analysis. Moreover, such adjustments assume independence between analyses, which is improbable given that patients are likely to share relevant characteristics despite being analysed in different subgroups. Also, the findings of this study may not apply to ICU patients without hypoxemic respiratory failure or those less ill. Differences in baseline characteristics between the two trials were evident. These differences likely reflect different patient populations: HOT-COVID patients were more homogeneous, primarily suffering from COVID-19 respiratory failure, whereas HOT-ICU patients were more heterogeneous and sicker, with multiple organ failure. Additionally, treatment algorithms for COVID-19 evolved during the pandemic. Initially, high-flow systems were avoided due to fears of transmission, but later, these systems were widely used to prevent intubation. These differences are unlikely due to variations in the interpretation of the common inclusion criteria, as both trials were conducted at the same sites by the same clinicians. The post hoc between-trial HTE analysis suggests that baseline or treatment differences may have influenced the intervention effects on the secondary outcome of days alive without life support, highlighting a limitation of our study. However, the between-trial HTE analysis for the primary outcome of 90-day mortality revealed no statistically significant heterogeneity.
Finally, we specifically included data from the HOT-ICU and HOT-COVID trials to reduce bias stemming from indirectness, thus enhancing the precision of overall effect estimates and allowing for investigation of subgroup effects. This selection was deliberate as both trials employed identical interventions and were conducted in similar settings, with randomised patients receiving supplemental oxygen via both open and closed systems. Unlike other large randomised controlled trials (RCTs) [6,7,8,9,10], which included a broader patient population, these two trials focused solely on patients with severe acute hypoxemic respiratory failure at randomisation and maintained the intervention throughout the entirety of ICU admission for up to 90 days. Although the trials were compatible, we recognise that their data may not be entirely independent and apply a hierarchical mixed model with clustering at both the trial and site levels.
Conclusion
This IPDMA revealed no significant differences in mortality or days alive without life support at 90 days when comparing a PaO2 target of 8–12 kPa overall. Subgroup analyses indicated that patients with COVID-19 targeted to a PaO2 of 8 kPa had more days alive without life support (moderate credibility), whereas patients with cancer showed higher mortality with a PaO2 target of 8 kPa and more days alive with a target of 12 kPa (low credibility). These findings need to be confirmed through trials specifically designed to evaluate these populations individually.
Data availability
We will make the final de-identified data set available for sharing in accordance with the recent International Committee of Medical Journal Editors (ICMJE) recommendations [50] and data sharing agreements adhering to the laws of the participating countries. All trial-related documents are available from www.cric.nu/hot-covid and www.cric.nu/hot-icu.
References
Helmerhorst HJF, Arts DL, Schultz MJ et al (2017) Metrics of arterial hyperoxia and associated outcomes in critical care. Crit Care Med 45:187–195. https://doi.org/10.1097/CCM.0000000000002084
O’Driscoll BR, Howard LS, Earis J et al (2017) BTS guideline for oxygen use in adults in healthcare and emergency settings. Thorax 72:i1-90. https://doi.org/10.1136/thoraxjnl-2016-209729
Beasley R, Chien J, Douglas J et al (2015) Thoracic Society of Australia and New Zealand oxygen guidelines for acute oxygen use in adults: Swimming between the flags. Respirology 20:1182–1191. https://doi.org/10.1111/resp.12620
Møller MH, Granholm A, Al Duhailib Z et al (2023) Higher versus lower oxygenation targets in adult ICU patients: a rapid practice guideline. Acta Anaesthesiol Scand. https://doi.org/10.1111/aas.14366
Schjørring OL, Klitgaard TL, Perner A et al (2021) Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med 384:1–11. https://doi.org/10.1056/NEJMoa2032510
Asfar P, Schortgen F, Boisramé-helms J et al (2017) Hyperoxia and hypertonic saline in patients with septic shock ( HYPERS2S ): a two-by-two factorial, multicentre, randomised, clinical trial. Lancet Respir Med 5:180–190. https://doi.org/10.1016/S2213-2600(17)30046-2
Mackle D, Bailey M, Beasley R et al (2020) Conservative oxygen therapy during mechanical ventilation in the ICU. N Engl J Med 382:989–998. https://doi.org/10.1056/nejmoa1903297
Barrot L, Asfar P, Mauny F et al (2020) Liberal or conservative oxygen therapy for acute respiratory distress syndrome. N Engl J Med 382:999–1008. https://doi.org/10.1056/nejmoa1916431
Schmidt H, Kjaergaard J, Hassager C et al (2022) Oxygen targets in comatose survivors of cardiac arrest. N Engl J Med. https://doi.org/10.1056/nejmoa2208686
Semler MW, Casey JD, Lloyd BD et al (2022) Oxygen-saturation targets for critically ill adults receiving mechanical ventilation. N Engl J Med 387:1759–1769. https://doi.org/10.1056/nejmoa2208415
Girardis M, Busani S, Damiani E et al (2016) Effect of conservative vs conventional oxygen therapy on mortality among patients in an intensive care unit the oxygen-icu randomized clinical trial. JAMA J Am Med Assoc 316:1583–1589. https://doi.org/10.1001/jama.2016.11993
Girardis M, de Man AME, Singer M (2023) Trials on oxygen targets in the critically ill patients: do they change our knowledge and practice? Intensive Care Med 49:559–562. https://doi.org/10.1007/s00134-023-06999-9
Barbateskovic M, Koster TM, Eck RJ et al (2021) A new tool to assess Clinical Diversity In Meta-analyses (CDIM) of interventions. J Clin Epidemiol 135:29–41. https://doi.org/10.1016/j.jclinepi.2021.01.023
Martin D, de Jong A, Radermacher P (2023) Is the U-shaped curve still of relevance to oxygenation of critically ill patients? Intensive Care Med 49:566–568. https://doi.org/10.1007/s00134-023-07014-x
Klitgaard TL, Schjørring OL, Nielsen FM et al (2023) Higher versus lower fractions of inspired oxygen or targets of arterial oxygenation for adults admitted to the intensive care unit. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD012631.pub3
Nielsen FM, Klitgaard TL, Siegemund M et al (2024) Lower vs higher oxygenation target and days alive without life support in COVID-19 the HOT-COVID randomized clinical trial. JAMA J Am Med Assoc. https://doi.org/10.1001/jama.2024.2934
Schjørring OL, Perner A, Wetterslev J et al (2019) Handling Oxygenation Targets in the Intensive Care Unit (HOT-ICU)-Protocol for a randomised clinical trial comparing a lower vs a higher oxygenation target in adults with acute hypoxaemic respiratory failure. Acta Anaesthesiol Scand 63:956–965. https://doi.org/10.1111/aas.13356
Mølgaard Nielsen F, Lass Klitgaard T, Crescioli E et al (2021) Handling oxygenation targets in ICU patients with COVID-19—Protocol and statistical analysis plan in the HOT-COVID trial. Acta Anaesthesiol Scand 65:1497–1504. https://doi.org/10.1111/aas.13956
Helmerhorst HJF, Schultz MJ, Van Der VPHJ et al (2015) Bench-to-bedside review : the effects of hyperoxia during critical illness. Crit Care. https://doi.org/10.1186/s13054-015-0996-4
Nielsen FM, Klitgaard TL, Bruun NH et al (2023) Lower or higher oxygenation targets for acute Hypoxaemic respiratory failure: protocol for an individual patient data meta-analysis. Acta Anaesthesiol Scand 67:1–9. https://doi.org/10.1111/aas.14220
Stewart LA, Clarke M, Rovers M et al (2015) Preferred reporting items for a systematic review and meta-analysis of individual participant data: the PRISMA-IPD statement. JAMA J Am Med Assoc 313:1657–1665. https://doi.org/10.1001/jama.2015.3656
Schjørring OL, Klitgaard TL, Perner A et al (2020) The handling oxygenation targets in the intensive care unit (HOT-ICU) trial: Detailed statistical analysis plan. Acta Anaesthesiol Scand 64:847–856. https://doi.org/10.1111/aas.13569
Schandelmaier S, Briel M, Varadhan R et al (2020) Development of the instrument to assess the credibility of effect modification analyses (ICEMAN) in randomized controlled trials and meta-analyses. CMAJ 192:E901–E906. https://doi.org/10.1503/cmaj.200077
Jakobsen JC, Gluud C, Winkel P, et al (2014) The thresholds for statistical and clinical significance—a five-step procedure for evaluation of intervention effects in randomised clinical trials. 1–12
Riley RD, Debray TPA (2021) The one‐stage approach to IPD meta‐analysis. In: Riley RD, Tierney JF, Stewart LA (eds) Individual participant data meta‐analysis. Wiley, pp 127–162. https://doi.org/10.1002/9781119333784.ch6
Lee Y, Nelder JA (1996) Hierarchical generalized linear models. J R Stat Soc Ser B 58:619–656. https://doi.org/10.1111/j.2517-6161.1996.tb02105.x
Rasmussen BS, Klitgaard TL, Perner A et al (2021) Oxygenation targets in ICU patients with COVID-19: a post hoc subgroup analysis of the HOT-ICU trial. Acta Anaesthesiol Scand. https://doi.org/10.1111/aas.13977
van der Wal LI, Grim CCA, del Prado MR et al (2023) Conservative versus liberal oxygenation targets in intensive care unit patients (ICONIC): a randomized clinical trial. Am J Respir Crit Care Med Preprint: https://doi.org/10.1164/rccm.202303-0560OC
Osuchowski MF, Winkler MS, Skirecki T et al (2021) The COVID-19 puzzle : deciphering pathophysiology and phenotypes of a new disease entity. Lancet Respir 9:622–642. https://doi.org/10.1016/S2213-2600(21)00218-6
Ackermann M, Verleden SE, Kuehnel M et al (2020) Pulmonary vascular endothelialitis, thrombosis, and angiogenesis in Covid-19. N Engl J Med 383:120–128. https://doi.org/10.1056/nejmoa2015432
McGonagle D, Bridgewood C, Meaney JFM (2021) A tricompartmental model of lung oxygenation disruption to explain pulmonary and systemic pathology in severe COVID-19. Lancet Respir Med 9:665–672. https://doi.org/10.1016/S2213-2600(21)00213-7
Khomich OA, Kochetkov SN, Bartosch B, Ivanov AV (2018) Redox biology of respiratory viral infections. Viruses. https://doi.org/10.3390/v10080392
Bastin A, Abbasi F, Roustaei N et al (2023) Severity of oxidative stress as a hallmark in COVID-19 patients. Eur J Med Res 28:1–10. https://doi.org/10.1186/s40001-023-01401-2
Dushianthan A, Bracegirdle L, Cusack R et al (2023) Alveolar hyperoxia and exacerbation of lung injury in critically ill SARS-CoV-2 pneumonia. Med Sci 11:70. https://doi.org/10.3390/medsci11040070
Klitgaard TL, Schjørring OL, Severinsen MT et al (2022) Lower versus higher oxygenation targets in ICU patients with haematological malignancy—insights from the HOT-ICU trial. BJA Open 128:55–64. https://doi.org/10.1016/j.bjao.2022.100090
Muz B, de la Puente P, Azab F, Azab AK (2015) The role of hypoxia in cancer progression, angiogenesis, metastasis, and resistance to therapy. Hypoxia. https://doi.org/10.2147/hp.s93413
Luo Z, Tian M, Yang G et al (2022) Hypoxia signaling in human health and diseases: implications and prospects for therapeutics. Signal Transduct Target Ther 7:1–30. https://doi.org/10.1038/s41392-022-01080-1
Tudur Smith C, Marcucci M, Nolan S et al (2016) Individual participant data meta-analyses compared with meta-analyses based on aggregate data (Review). Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.MR000007.pub3.www.cochranelibrary.com
Reade MC, Delaney A, Bailey MJ et al (2010) Prospective meta-analysis using individual patient data in intensive care medicine. Intensive Care Med 36:11–21. https://doi.org/10.1007/s00134-009-1650-x
Riley RD, Lambert PC, Abo-Zaid G (2010) Meta-analysis of individual participant data: rationale, conduct, and reporting. BMJ 340:521–525. https://doi.org/10.1136/bmj.c221
de Grooth HJ, Parienti JJ (2023) Heterogeneity between studies can be explained more reliably with individual patient data. Intensive Care Med Preprint: https://doi.org/10.1007/s00134-023-07163-z
Bos LDJ, Laffey JG, Ware LB et al (2022) Towards a biological definition of ARDS: are treatable traits the solution? Intensive Care Med Exp 10:1–14. https://doi.org/10.1186/s40635-022-00435-w
Grasselli G, Calfee CS, Camporota L et al (2023) ESICM guidelines on acute respiratory distress syndrome: definition, phenotyping and respiratory support strategies. Springer, Berlin
UK-ROX (ICNARC project number: NIHR130508). https://www.icnarc.org/Our-Reseach/Studies/Uk-Rox. Accessed 4 Jan 2024
Young PJ, Al-Fares A, Aryal D et al (2023) Protocol and statistical analysis plan for the mega randomised registry trial comparing conservative vs. liberal oxygenation targets in adults with nonhypoxic ischaemic acute brain injuries and conditions in the intensive care unit (Mega-ROX Brains). Crit Care Resusc 25:53–59. https://doi.org/10.1016/j.ccrj.2023.04.011
Holgersson J, Meyer MAS, Dankiewicz J et al (2022) Hypothermic versus normothermic temperature control after cardiac arrest. NEJM Evid. https://doi.org/10.1056/evidoa2200137
Young PJ, Bellomo R, Bernard GR et al (2019) Fever control in critically ill adults. an individual patient data meta-analysis of randomised controlled trials. Intensive Care Med 45:468–476. https://doi.org/10.1007/s00134-019-05553-w
Rowan KM, Angus DC, Bailey M et al (2017) Early, goal-directed therapy for septic shock—a patient-level meta-analysis. N Engl J Med 376:2223–2234. https://doi.org/10.1056/NEJMoa1701380
Kent DM, Steyerberg E, Van Klaveren D (2018) Personalized evidence based medicine: Predictive approaches to heterogeneous treatment effects. BMJ 363:k4245
International Comittee of Medical Journal Editors (ICMJE) Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly work in Medical Journals. https://www.icmje.org/recommendations/. Accessed 22 Sep 2023
Funding
Open access funding provided by Aalborg University Hospital. This work was funded by the Danish Ministry of Higher Education and Science, the Innovation Fund Denmark and others; HOT-ICU ClinicalTrials.gov number, NCT03174002; HOT-COVID ClinicalTrials.gov number, NCT04425031.
Author information
Authors and Affiliations
Contributions
Concept and design: all authors. Acquisition, analysis, or interpretation of data: all authors. Drafting of manuscript: FMN drafted the first version of the manuscript. All authors carefully read and approved the final version. Statistical analysis: NHB and FMN. Data Access, Responsibility, and Analysis: FMN, NHB and BSR all had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Conflict of Interest
FMN was coordinating investigator of the HOT-COVID trial. TLK was coordinating investigator of the HOT-ICU and HOT-COVID trials. OLS was coordinating investigator of the HOT-ICU trial. BSR was the sponsor of the HOT-ICU and HOT-COVID trials. MHM has no conflict of interest. NHB has no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nielsen, F.M., Klitgaard, T.L., Bruun, N.H. et al. Lower or higher oxygenation targets in the intensive care unit: an individual patient data meta-analysis. Intensive Care Med (2024). https://doi.org/10.1007/s00134-024-07523-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00134-024-07523-3