Abstract
Purpose
After cardiac surgery, fluid bolus therapy (FBT) with 20% human albumin may facilitate less fluid and vasopressor administration than FBT with crystalloids. We aimed to determine whether, after cardiac surgery, FBT with 20% albumin reduces the duration of vasopressor therapy compared with crystalloid FBT.
Methods
We conducted a multicentre, parallel-group, open-label, randomised clinical trial in six intensive care units (ICUs) involving cardiac surgery patients deemed to require FBT. We randomised 240 patients to receive up to 400 mL of 20% albumin/day as FBT, followed by 4% albumin for any subsequent FBT on that day, or to crystalloid FBT for at least the first 1000 mL, with use of crystalloid or 4% albumin FBT thereafter. The primary outcome was the cumulative duration of vasopressor therapy. Secondary outcomes included fluid balance.
Results
Of 480 randomised patients, 466 provided consent and contributed to the primary outcome (mean age 65 years; median EuroSCORE II 1.4). The cumulative median duration of vasopressor therapy was 7 (interquartile range [IQR] 0–19.6) hours with 20% albumin and 10.8 (IQR 0–22.8) hours with crystalloids (difference − 3.8 h, 95% confidence interval [CI] − 8 to 0.4; P = 0.08). Day one fluid balance was less with 20% albumin FBT (mean difference − 701 mL, 95% CI − 872 to − 530).
Conclusions
In patients after cardiac surgery, when compared to a crystalloid-based FBT, 20% albumin FBT was associated with a reduced positive fluid balance but did not significantly reduce the duration of vasopressor therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
We conducted a multicentre randomised controlled trial of 20% albumin vs. crystalloid-based fluid bolus therapy (FBT) in 480 cardiac surgery patients admitted to intensive care unit. FBT with 20% albumin was associated with a less positive fluid balance but did not result in a statistically significant reduction in the duration of vasopressor therapy. This information can be used to guide choice of agent for FBT in this setting. |
Introduction
Intravenous fluid bolus therapy (FBT) is common after cardiac surgery [1]. It is given to optimize intravascular volume and end organ perfusion and it accounts for half of all the intravenous fluid received during the first post-operative day [1]. FBT may consist of crystalloid and/or colloid fluid. Albumin, a natural colloid, may improve haemodynamics with less administered volume than crystalloid fluids [2,3,4]. Accordingly, albumin solutions are widely used after cardiac surgery in some countries [5, 6].
Amongst albumin solutions, 4% albumin is the most frequently used colloid in intensive care units (ICUs) worldwide [7, 8]. However, 20% albumin has been reported to confer a physiological advantage compared to both crystalloid [3] and 4% albumin [9] and a survival benefit in patients with liver failure [10] and in septic shock patients [3]. Consistent with such observations, in a recent pilot trial in cardiac surgery patients, compared to FBT with crystalloids, FBT with up to 200 mL of 20% albumin was associated with a reduced duration and dose of norepinephrine [11].
Like FBT, vasopressor therapy is also common after cardiac surgery [12, 13] with its initiation often dependent on the haemodynamic status achieved with prior FBT. Vasopressor therapy is mostly based on catecholamines such as norepinephrine or epinephrine. Catecholamines, however, may reduce blood flow to end organs by vasoconstricting their vascular beds and have negative sequelae on cardiac [14,15,16,17], metabolic, microbiome, and immune functions [18]. Reducing vasopressor duration in patients most susceptible to such effects may reduce morbidity [19, 20]. Thus, achieving and sustaining hemodynamic targets with less fluid and reduced duration of vasopressor therapy appears desirable.
Accordingly, we tested the primary hypothesis that, compared to FBT with crystalloid fluids, 20% albumin FBT would reduce the duration of vasopressor use in patients after cardiac surgery requiring cardiopulmonary bypass. We also tested the secondary hypothesis that 20% albumin FBT would do so whilst decreasing fluid balance.
Methods
Study design
The HAS FLAIR-II trial was a pragmatic investigator-initiated, multicentre, open label, randomised controlled trial (Australian New Zealand Clinical Trial Registry; ACTRN No. 12620000137998). The Austin Hospital Human Research Ethics Committee approved the trial protocol, which is available in the supplemental materials (HREC/57780/Austin-2019). The research ethics committee granted approval for a hierarchical consent model, consistent with the Australian National Health and Medical Research Council statement on ethical conduct in human research and local laws (electronic supplemental materials, ESMs) [21]. We used the CONSORT Statement checklist for the reporting of randomised clinical trials [22]. A independent data and safety monitoring committee oversaw the conduct of the study and reviewed blinded safety data.
Study Population
We conducted this trial at six ICUs in Australia. Screening was conducted by a HAS FLAIR-II Investigator (ESM). Patient eligibility criteria were the treating clinician considered that FBT was necessary in the ICU after any form of cardiac surgery requiring cardiopulmonary bypass. Other criteria were that the use of albumin and crystalloid as FBT was judged equally appropriate, the patient was mechanically ventilated at the time of ICU admission after cardiac surgery, and arterial and central venous catheters were in situ. Patients were excluded if any of the following were true: aged less than 18 years of old, previous FBT in the ICU after cardiac surgery, known contraindication to the study fluid (e.g. hypersensitivity reaction), documented refusal of study fluid, imminent death, previous enrolment in HAS FLAIR-II or pregnancy.
Randomisation and allocation concealment
Patients in the trial were randomly assigned 1:1 to receive 20% albumin or crystalloid FBT using a computer-generated permuted block sequence (sizes 2 and 4) provided by an independent statistician. The schedule was stratified by site and the presence of a vasopressor at the time of randomisation. The sequence was embedded into the Research Electronic Data Capture (REDCap) system, with allocation concealed until after study personnel had enrolled each patient [23, 24].
Interventions
For up to 7 days after randomisation, or until vasopressor therapy was discontinued for 4 consecutive hours in the presence of a mean arterial pressure (MAP) ≥ 65 mmHg, patients received all FBT in the ICU as the assigned trial fluid. In the intervention group, patients received clinician-determined FBT as 20% albumin (presented as a 100 mL bottle; CSL Behring, Melbourne, Australia) up to a maximum of 400 mL (80 g albumin) per calendar day. If this daily maximum were reached, additional FBT on that calendar day was administered as 4% albumin—presented as a 500 mL bottle (CSL Behring, Melbourne, Australia).
The crystalloid group were not permitted to receive any form of albumin until cumulatively at least 1000 mL of crystalloid fluid bolus had been received. Thereafter, the treating clinician could use 4% albumin (but not 20% albumin). Suitable crystalloid solutions included 0.9% sodium chloride solution, compound sodium lactate or Plasma-Lyte148 (Baxter Healthcare).
Once the patient was discharged from the ICU, the type of fluid administered was not dictated by the trial protocol. All other treatments were administered at the discretion of the treating clinician.
Outcome measures
The primary outcome was the cumulative duration of vasopressor therapy until the first observed period of cessation of vasopressor therapy. Primary outcome data were censored at midnight on study day 7; calendar days were used with day 1 as a partial day. Cessation of vasopressor therapy was defined as discontinuation of all vasopressor drugs for 4 consecutive hours in the presence of a MAP ≥ 65 mmHg. The primary outcome of cessation of vasopressors could occur only once, even if vasopressors were recommenced > 4 h later. Patients who did not receive any vasopressor drug within 7 days of randomisation were assigned zero hours of vasopressor therapy. Drugs considered as vasopressors are listed in supplementary Table S1 [25].
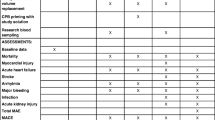
Secondary outcomes included fluid balance, cumulative proportion of patients receiving any vasopressor drug, duration of mechanical ventilation and ICU admission, time to readiness for ICU discharge, duration of hospital admission and death at day 7 and 30.
Statistical analysis
The statistical analysis plan was reported before the completion of enrolment [26]. We assumed a pooled standard deviation of vasopressor therapy duration of 32 h. It was estimated that 200 patients per group would have 80% power (2-sided α = 0.05) to detect a difference in the cumulative hours of vasopressor therapy of 9 h. Whilst there is no current consensus, we postulate that a 9-h reduction in the duration of vasopressor therapy would represent a minimally important clinical difference. Since this patient cohort in our region is typically managed by 2 or 3 nursing shifts in a 24-h period. A reduction of work-load across one short shift, or earlier suitability for ward discharge may translate in practise to lower clinical resource consumption. As the distribution of the primary outcome was expected to be nonparametric, the sample size was inflated by 15% [27]. To further account for withdrawal from the trial and refusing to allow retention of data (5%), we planned to enrol 480 patients.
Categorical variables are reported using frequencies and percentages. Continuous variables are reported as means with standard deviations and medians with interquartile ranges (IQRs).
The primary outcome was calculated as the difference (95% confidence interval [CI]) in the median (quantile = 0.5) cumulative hours of vasopressor treatment between the 20% albumin and crystalloid group within a simple quantile linear regression model incorporating trial site and vasopressor use at the time of randomisation as a random effect [28]. Secondary outcomes were calculated similarly except for the outcome’s, mortality and the cumulative proportion of patients receiving any vasopressor therapy which were returned by a simple logistic model incorporating trial site and vasopressor use at the time of randomisation as a random effect [28].
The primary outcome was assessed in a total of three subgroups. The first two were pre-specified in the protocol (presence or absence of vasopressor therapy at the time of a randomisation and according to a preoperative plasma albumin ≤ 37 g/L) whilst the third (according to sex) was a supplementary (post hoc) addition. Heterogeneity between subgroups in the primary outcome was tested for using a quantile linear regression model incorporating trial site and vasopressor use at the time of randomisation as a random effect and an interaction between treatment and subgroup. Time to vasopressor liberation in the strata of patients receiving vasopressor therapy at randomisation is summarised graphically using Kaplan–Meier curves.
Vasopressor use over the first 7 days was converted to equivalent norepinephrine doses using an established methodology and reported graphically as medians, IQRs, and ranges in a box plot [29].
Patients were analysed according to their randomised group and we included all the patients except for those who had withdrawn consent for any use of their data. We did not impute missing values. The numbers of patients with available data are reported. An independent data and safety monitoring board reviewed the data and performed one blinded interim analysis of the primary end point after recruitment and 30-day follow-up of 235 patients, using the Haybittle-Peto stopping rule (|Zk|≥ 3) for early termination due to probable harm or strong evidence of benefit. The data and safety monitoring committee recommended continuation of the trial on the basis of this analysis. Because of the negligible effect of this interim analysis on expenditure of error, the final analyses at full recruitment were minimally affected and consequently all final analyses were conducted with a 2-sided type I error alpha = 0.05. We did not correct for multiple comparisons in the evaluation of secondary outcomes. Thus, such results are exploratory and are reported as point estimates with 95% confidence intervals. All the analyses were performed with the use of R version 4.1.2 (R foundation, Vienna, Austria).
Results
Patient characteristics
From 31 August 2020 to 31 August 2022, we randomised 480 patients in six ICUs, with the final follow-up occurring on 5 September 2022. Consent to continue participation and retention of trial data were rejected by 14 patients (supplementary Table S2), resulting in 233 of 240 (97%) patients assigned to the 20% albumin group and 233 of 240 (97%) assigned to the crystalloid group (Fig. 1).Footnote 1 Baseline and clinical characteristics of enrolled patients were balanced and are shown in Table 1.
Study treatment
During the first post-operative day (median duration 8.8 hours [IQR 6–10.3]), the volume of administered FBT differed between the groups, with a mean of 363 (standard deviation [SD], 312) mL in the 20% albumin group and 1275 (SD, 773) mL in the crystalloid group [mean difference of − 912 mL (95% CI, − 1019 to − 805)] (Table 2 and supplementary Fig. S1). The early (first post-operative day) fluid balance was + 164 (SD 733) mL with 20% albumin and + 865 (SD 1106) mL with crystalloid fluid [mean difference − 701 mL (95% CI − 872 to − 530)] (Table 2). Additional 4% albumin was administered in 138 of 233 patients (59%) in the crystalloid group. The total fluid input (by any route), output, and urine output are presented in supplementary Figs. S2 to S4. Non-albumin blood products administered whilst in ICU up to day 7 are summarised in supplementary Table S3.
The mean amount of albumin administered through FBT was greater in the 20% albumin group compared to the crystalloid group for the first 2 days (supplementary Fig. S5). After randomisation, the daily plasma albumin concentration was also greater in the 20% albumin group (supplementary Fig. S6). Additional physiological and biochemical descriptors by treatment group are provided in supplementary Figs. S7 through to S15. The number of patients with one or more protocol violations was 19 (8.2%) in the 20% albumin group and 25 (10.7%) in the crystalloid group and the details are presented in supplementary Table S4.
Primary outcome
The primary outcome was available in all patients and is presented in Table 3 and Fig. 2. The difference in the cumulative duration of vasopressor therapy between the 20% albumin and crystalloid group was − 3.8 (95% CI − 8 to 0.4 ; P = 0.08) hours.
Vasopressor duration. A Distributions of vasopressor hours by study group as the cumulative proportion (y-axis) for each study group by hours (x-axis). Curves that rise faster are more favourable. B Vasopressor hours as horizontally stacked proportions by study group. Red represents better values and blue represents worse values
Secondary outcomes
Receipt of at least one vasopressor occurred in 169 patients (73%) in the 20% albumin group and in 170 patients (73%) in the crystalloid group. The median time to the commencement of vasopressor therapy in those not already receiving a vasopressor at randomisation was 1.7 (IQR 0.2–5) hours in the 20% albumin group and 1.5 (IQR 0.5–3.9) hours in the crystalloid group (supplementary Fig. S16). There was no difference in the duration of ventilation, time to readiness for ICU discharge, ICU, or hospital length of stay between the two groups (Table 3). Death prior to day 30 occurred in 2 of 233 (1%) in the 20% albumin group and 3 of 230 (1%) in the crystalloid group (Table 3). The vasopressor dose by treatment group during the first 7 days after randomisation is presented in supplementary Fig. S17.
Subgroup analysis
Differential treatment effects on vasopressor duration were not observed in the two pre-specified subgroups (supplementary Fig. S18) but may have been present according to sex. Amongst patients receiving vasopressors at randomisation, the median cumulative duration of vasopressor therapy in ICU up until day 7 was 16.9 (IQR 10–26.8) hours in the 20% albumin group and 20 (IQR 12.1–40.3) hours in the crystalloid group (difference − 3.2 h [95% CI − 7.8 to 1.4]; P = 0.17, supplementary Figs. S18-19).
Adverse events
Adverse events are reported in supplementary Table S6. No unexpected serious, possibly intervention related adverse events occurred.
Discussion
Key findings
In patients after cardiac surgery, FBT with 20% albumin compared to crystalloid fluid did not significantly reduce the cumulative duration of vasopressor therapy. However, FBT with 20% albumin was associated with a reduced volume of fluid used for resuscitation and a less positive post-operative fluid balance. Finally, we did not observe any adverse events with the use of 20% albumin.
Relationship to previous findings
Several lines of evidence support the notion that 20% albumin causes longer lasting plasma-volume expansion [30,31,32]. This effect may be logically expected to attenuate the need for vasopressor support. However, in adults treated in ICU after cardiac surgery, the data are sparse.
In a comparative observational trial of 120 ventilated cardiac surgery patients [33], investigators recorded blood pressure measurements continuously and cardiac output 15 min before and for 30 min after FBT. Patients were grouped into those that received 500 mL of crystalloid, 500 mL of 4% albumin or 100 mL of 20% albumin group. The initial effect on blood pressure and cardiac output of 20% albumin was similar to 500 mL of 4% albumin or crystalloid fluid, but with 80% less volume. Moreover, there were more rapid reductions in blood pressure after crystalloid FBT suggesting a difference in how the effect might be sustained.
In an observational study [34] of the cardiovascular effect of 20% albumin in 20 patients after cardiac surgery, investigators reported that hypotension was the most common trigger for FBT, and that a mean arterial pressure increase of > 10% occurred in 85% of patients during the 20% albumin bolus. However, such effect dissipated in two thirds of patients within the following 10 min. Our findings align with such observations.
In a previous single centre before-and-after exploratory study [11], 50 patients were treated with crystalloid FBT and 50 patients with up to two ‘doses’ of 100 mL of 20% albumin. FBT with 20% albumin diminished fluid balance, with less volume of FBT administered and achieved a significantly shorter median time to cessation of norepinephrine. The present study findings are aligned with such preliminary observations in terms of fluid balance but the reduction in the duration of vasopressor observed was not significant.
Finally, a recent randomised controlled trial compared 4% albumin solution as cardiopulmonary bypass priming as well as intravenous volume replacement intraoperatively and for up to 24-h postoperatively to Ringer acetate solution in 1386 patients [35]. The investigators reported reduced fluid balance during the 24-h intervention period with 4% albumin but no difference in post-operative complications between the two groups. No data were presented regarding the use of vasopressor agents.
Implications of study findings
Our findings suggest that, in cardiac surgery patients admitted to ICU and deemed to need FBT by the treating team, 20% albumin FBT does not significantly reduce the duration of vasopressor therapy.
Study strengths and limitations
This study has several strengths. As a pragmatic multicentre trial conducted in trial sites with mortality and processes of care outcomes consistent with those reported in global cardiac registries [36,37,38,39,40], the results are likely to carry a degree of external validity. To minimise biases and promote balance, the permuted block random allocation sequence was concealed and stratified by study centre. There was no loss of data for the primary outcome. Treatment separation was achieved as shown by the plasma albumin levels.
This trial has several limitations. First, the intervention was not masked, and the primary outcome may have been influenced by bedside clinicians. This creates the potential for performance and observer bias. However, blinding of intravenous fluid requires considerable logistical support to ensure patient safety, and whilst this has been done for phase III trials [2, 41] we considered the cost and complexity prohibitive for this trial, particularly given the fluid is provided in different volumes and containers. In the absence of consensus on indications for FBT initiation or algorithms for goal directed therapy in cardiac surgery [42], the decision to administer FBT was at the discretion of the treating clinical team, according to their local practise. Patients were cared for by a large multi-disciplinary team spanning several shift changes, making systematic performance bias less likely. Second, the number of additional episodes of vasopressor treatment (recommencing vasopressors after 4 h without vasopressor treatment) was not collected. Third, in keeping with the pragmatic nature of the trial and study feasibility, 4% albumin was permitted after the first 1000 mL of crystalloid FBT as this is common practice in our region [6]. However, this may have led to an underestimation of the effect of 20% albumin. Fourth, enrolment was not restricted to patients receiving vasopressors prior to randomisation because we reasoned that a proportion would, later, go on to receive vasopressor therapy. This proportion would be decreased if 20% albumin was a more effective therapy in improving the blood pressure and/or cardiac output. Fifth, as a pragmatic trial only the intervention i.e. the composition of FBT was protocolised. Processes of care such as sedation and transfusion of non-albumin blood products were determined by the treating clinician, according to their local practice. Sixth, data regarding the administration of systemic corticosteroids as a co-intervention such as hydrocortisone (an uncommon practice in Australia), were not collected.
Conclusion
In adult patients after cardiac surgery requiring cardiopulmonary bypass in whom clinician-determined FBT was administered, compared to a predominantly crystalloid-based approach, FBT with 20% albumin did not result in a statistically significant reduction in the duration of vasopressor therapy but was associated with a reduced fluid balance. These findings can be used to guide intensive care clinicians in the choice of fluid for FBT in cardiac surgery patients.
Statement on data sharing
Deidentified individual participant data collected during the HAS FLAIR-II trial (and the data dictionary) will be shared beginning two years after article publication with no end date. These data will be available to researchers to who provide a methodologically sound proposal for the purposes of achieving specific aims outlined in that proposal. Proposals should be directed to the corresponding author via email: geoff.wigmore@unimelb.edu.au and will be reviewed by the HAS FLAIR-II study management committee. Requests to access data to undertake hypothesis-driven research will not be unreasonably withheld. To gain access, data requesters will need to sign a data access agreement and to confirm that data will only be used for the agreed purpose for which access was granted.
Notes
e.g. known hypersensitivity reaction to the study fluid—refers to the exclusion criterion—Contraindication to study fluids in the CONSORT diagram.
References
Parke RL, McGuinness SP, Gilder E, McCarthy LW (2014) Intravenous fluid use after cardiac surgery: a multicentre, prospective, observational study. Crit Care Resusc 16:164–169
Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R, Doig G, Hayek M, O’Donnell S, Bell A, Blythe D, Cade J, Chapman M, Cole L, Cooper J, Davies A, French C, Joyce C, McArthur C, MacMahon S, Neal B, Presneill J, Saul P, Seppelt I, Stephens D, Turner A, Williams A, Woolfe C, Peto R, Sandercock P, Sprung C, Young D, Lo SK, Sivarajasingham S, Francis L, Woodward M, Charlton J, Harry C, Higgins L, Moulden K, Vallance S, Chadderton J, Newby L, Bates S, Goldsmith D, Voss A, Palermo A, Jayne K, Merai M, Pandey S, Schmidt M, Carroll R, McFadyen B, Clarke J, Powell J, Tai J, Hynesova I, Weisbrodt L, Bradley L, Kelly T, Limpus A, Moore R, Creed S, Kaplan S, Rivett J, Thomas J, Marsden K, Boyce C, Howe B, Robertson M, O’Connor A, Potter J, Ramakrishnan N, Powell C, Rajbhandari D, Girling K, Hodgetts M, Jovanovska A, Little L, The SSI (2004) A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med 350:2247–2256. https://doi.org/10.1056/NEJMoa040232
Caironi P, Tognoni G, Masson S, Fumagalli R, Pesenti A, Romero M, Fanizza C, Caspani L, Faenza S, Grasselli G, Iapichino G, Antonelli M, Parrini V, Fiore G, Latini R, Gattinoni L (2014) Albumin replacement in patients with severe sepsis or septic shock. N Engl J Med 370:1412–1421. https://doi.org/10.1056/NEJMoa1305727
Hanley C, Callum J, Karkouti K, Bartoszko J (2021) Albumin in adult cardiac surgery: a narrative review. Can J Anaesth 68:1197–1213. https://doi.org/10.1007/s12630-021-01991-7
Liu L, McCluskey SA, Law M, Abrahamyan L, Peer M, Tait G, Rao V, Wijeysundera DN, Scales DC, Callum J, Karkouti K, Bartoszko J (2022) Albumin use for fluid resuscitation in cardiac surgical patients: a survey of Canadian perioperative care providers. Can J Anesthesia/J Canadien d’anesthésie 69:818–831. https://doi.org/10.1007/s12630-022-02237-w
Ramanan M, Roberts S, Adrian McCullough JP, Naidoo R, Rapchuk I, Matebele M, Tabah A, Kruger P, Smith J, Shekar K (2021) Fluid resuscitation after cardiac surgery in the intensive care unit: a bi-national survey of clinician practice. (The FRACS-ICU clinician survey). Ann Card Anaesth 24:441–446. https://doi.org/10.4103/aca.ACA_190_20
Hammond NE, Taylor C, Saxena M, Liu B, Finfer S, Glass P, Seppelt I, Willenberg L, Myburgh J (2015) Resuscitation fluid use in Australian and New Zealand Intensive Care Units between 2007 and 2013. Intensive Care Med 41:1611–1619. https://doi.org/10.1007/s00134-015-3878-y
Glassford NJ, Mårtensson J, Eastwood GM, Jones SL, Tanaka A, Wilkman E, Bailey M, Bellomo R (2016) Defining the characteristics and expectations of fluid bolus therapy: a worldwide perspective. J Crit Care 35:126–132. https://doi.org/10.1016/j.jcrc.2016.05.017
Mårtensson J, Bihari S, Bannard-Smith J, Glassford NJ, Lloyd-Donald P, Cioccari L, Luethi N, Tanaka A, Crisman M, Rey de Castro N, Ottochian M, Huang A, Cronhjort M, Bersten AD, Prakash S, Bailey M, Eastwood GM, Bellomo R (2018) Small volume resuscitation with 20% albumin in intensive care: physiological effects: the SWIPE randomised clinical trial. Intensive Care Med 44:1797–1806. https://doi.org/10.1007/s00134-018-5253-2
Caraceni P, Riggio O, Angeli P, Alessandria C, Neri S, Foschi FG, Levantesi F, Airoldi A, Boccia S, Svegliati-Baroni G, Fagiuoli S, Romanelli RG, Cozzolongo R, Di Marco V, Sangiovanni V, Morisco F, Toniutto P, Tortora A, De Marco R, Angelico M, Cacciola I, Elia G, Federico A, Massironi S, Guarisco R, Galioto A, Ballardini G, Rendina M, Nardelli S, Piano S, Elia C, Prestianni L, Cappa FM, Cesarini L, Simone L, Pasquale C, Cavallin M, Andrealli A, Fidone F, Ruggeri M, Roncadori A, Baldassarre M, Tufoni M, Zaccherini G, Bernardi M, Domenicali M, Giannone FA, Merli M, Gioia S, Fasolato S, Sticca A, Campion D, Risso A, Saracco GM, Maiorca D, Rizzotto A, Lanzi A, Neri E, Visani A, Mastroianni A, Alberti AB, Mazzarelli C, Vangeli M, Marzioni M, Capretti F, Kostandini A, Magini G, Colpani M, Laffi G, Gabbani T, Marsico M, Zappimbulso M, Petruzzi J, Calvaruso V, Parrella G, Caporaso N, Auriemma F, Guarino M, Pugliese F, Gasbarrini A, Leo P, De Leonardis F, Pecchioli A, Rossi P, Raimondo G, Negri E, Dallio M, Loguercio C, Conte D, Celli N, Bringiotti R, Castellaneta NM, Salerno F (2018) Long-term albumin administration in decompensated cirrhosis (ANSWER): an open-label randomised trial. The Lancet 391:2417–2429. https://doi.org/10.1016/S0140-6736(18)30840-7
Wigmore GJ, Anstey JR, St. John A, Greaney J, Morales-Codina M, Presneill JJ, Deane AM, MacIsaac CM, Bailey M, Tatoulis J, Bellomo R (2019) 20% Human albumin solution fluid bolus administration therapy in patients after cardiac surgery (the HAS FLAIR Study). J Cardiothor Vasc Anesth 33:2920–2927. https://doi.org/10.1053/j.jvca.2019.03.049
Guinot PG, Durand B, Besnier E, Mertes PM, Bernard C, Nguyen M, Berthoud V, Abou-Arab O, Bouhemad B (2023) Epidemiology, risk factors and outcomes of norepinephrine use in cardiac surgery with cardiopulmonary bypass: a multicentric prospective study. Anaesth Crit Care Pain Med 42:101200. https://doi.org/10.1016/j.accpm.2023.101200
Vail EA, Shieh MS, Pekow PS, Gershengorn HB, Walkey AJ, Lindenauer PK, Wunsch H (2021) Use of vasoactive medications after cardiac surgery in the United States. Ann Am Thorac Soc 18:103–111. https://doi.org/10.1513/AnnalsATS.202005-465OC
Duarte PAD, Leichtweis GE, Andriolo L, Delevatti YA, Jorge AC, Fumagalli AC, Santos LC, Miura CK, Saito SK (2017) Factors associated with the incidence and severity of new-onset atrial fibrillation in adult critically ill patients. Crit Care Res Pract 2017:8046240. https://doi.org/10.1155/2017/8046240
Wittstein IS (2012) Stress cardiomyopathy: a syndrome of catecholamine-mediated myocardial stunning? Cell Mol Neurobiol 32:847–857. https://doi.org/10.1007/s10571-012-9804-8
Rona G (1985) Catecholamine cardiotoxicity. J Mol Cell Cardiol 17:291–306. https://doi.org/10.1016/s0022-2828(85)80130-9
Liaudet L, Calderari B, Pacher P (2014) Pathophysiological mechanisms of catecholamine and cocaine-mediated cardiotoxicity. Heart Fail Rev 19:815–824. https://doi.org/10.1007/s10741-014-9418-y
Andreis DT, Singer M (2016) Catecholamines for inflammatory shock: a Jekyll-and-Hyde conundrum. Intensive Care Med 42:1387–1397. https://doi.org/10.1007/s00134-016-4249-z
Lamontagne F, Richards-Belle A, Thomas K, Harrison DA, Sadique MZ, Grieve RD, Camsooksai J, Darnell R, Gordon AC, Henry D, Hudson N, Mason AJ, Saull M, Whitman C, Young JD, Rowan KM, Mouncey PR (2020) Effect of reduced exposure to vasopressors on 90-day mortality in older critically ill patients with vasodilatory hypotension: a randomized clinical trial. JAMA 323:938–949. https://doi.org/10.1001/jama.2020.0930
Richards-Belle A, Hylands M, Muttalib F, Taran S, Rochwerg B, Day A, Mouncey PR, Radermacher P, Couban R, Asfar P, Adhikari NKJ, Lamontagne F (2023) Lower versus higher exposure to vasopressor therapy in vasodilatory hypotension: a systematic review with meta-analysis. Crit Care Med 51:254–266. https://doi.org/10.1097/ccm.0000000000005736
National Health and Medical Research Council (Australia), Australian Research Council., Australian Vice-Chancellors' Committee. (2007 (Updated 2018)) National Statement on Ethical Conduct in Human Research.
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMJ 340:c332. https://doi.org/10.1136/bmj.c332
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, Duda SN, Consortium RE (2019) The REDCap consortium: building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG (2009) Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Fujii T, Luethi N, Young PJ, Frei DR, Eastwood GM, French CJ, Deane AM, Shehabi Y, Hajjar LA, Oliveira G, Udy AA, Orford N, Edney SJ, Hunt AL, Judd HL, Bitker L, Cioccari L, Naorungroj T, Yanase F, Bates S, McGain F, Hudson EP, Al-Bassam W, Dwivedi DB, Peppin C, McCracken P, Orosz J, Bailey M, Bellomo R, Investigators ftVT (2020) Effect of vitamin c, hydrocortisone, and thiamine vs hydrocortisone alone on time alive and free of vasopressor support among patients with septic shock: the VITAMINS randomized clinical trial. JAMA 323:423–431. https://doi.org/10.1001/jama.2019.22176
Wigmore G, Deane AM, Anstey J, Bailey M, Bihari S, Eastwood G, Ghanpur R, Maiden MJ, Presneill JJ, Raman J, Bellomo R, for the Has Flair-II trial investigators (2022) Study protocol and statistical analysis plan for the 20% human albumin solution fluid bolus administration therapy in patients after cardiac surgery-ll (HAS FLAIR-II) trial. Crit Care Resusc 24:309–318. https://doi.org/10.51893/2022.4.OA1
Lehmann Eldahjm (1998) Nonparametrics : statistical methods based on ranks. Prentice Hall, Upper Saddle River
International Council for Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (1998) ICH Topic E9 Statistical Principles for Clinical Trials. https://www.ema.europa.eu/en/documents/scientific-guideline/ich-e-9-statistical-principles-clinical-trials-step-5_en.pdf
Khanna A, English SW, Wang XS, Ham K, Tumlin J, Szerlip H, Busse LW, Altaweel L, Albertson TE, Mackey C, McCurdy MT, Boldt DW, Chock S, Young PJ, Krell K, Wunderink RG, Ostermann M, Murugan R, Gong MN, Panwar R, Hästbacka J, Favory R, Venkatesh B, Thompson BT, Bellomo R, Jensen J, Kroll S, Chawla LS, Tidmarsh GF, Deane AM (2017) Angiotensin II for the treatment of vasodilatory shock. N Engl J Med 377:419–430. https://doi.org/10.1056/NEJMoa1704154
Bihari S, Bannard-Smith J, Bellomo R (2020) Albumin as a drug: its biological effects beyond volume expansion. Crit Care Resusc 22:257–265. https://doi.org/10.1016/S1441-2772(23)00394-0
Hahn RG, Zdolsek M, Hasselgren E, Zdolsek J, Björne H (2019) Fluid volume kinetics of 20% albumin. Br J Clin Pharmacol 85:1303–1311. https://doi.org/10.1111/bcp.13897
Zdolsek M, Hahn RG, Zdolsek JH (2018) Recruitment of extravascular fluid by hyperoncotic albumin. Acta Anaesthesiol Scand 62:1255–1260. https://doi.org/10.1111/aas.13150
Yanase F, Cutuli SL, Naorungroj T, Bitker L, Wilson A, Eastwood GM, Bellomo R (2021) A comparison of the hemodynamic effects of fluid bolus therapy with crystalloids vs. 4% albumin and vs. 20% albumin in patients after cardiac surgery. Heart Lung 50:870–876. https://doi.org/10.1016/j.hrtlng.2021.07.014
Cutuli SL, Bitker L, Osawa EA, O’Brien Z, Canet E, Yanase F, Ancona P, Wilson A, Lucchetta L, Kubicki M, Cronhjort M, Cioccari L, Peck L, Young H, Eastwood GM, Martensson J, Glassford NJ, Bellomo R (2020) Haemodynamic effect of a 20% albumin fluid bolus in post-cardiac surgery patients. Crit Care Resusc 22:15–25. https://doi.org/10.51893/2020.1.oa2
Pesonen E, Vlasov H, Suojaranta R, Hiippala S, Schramko A, Wilkman E, Eränen T, Arvonen K, Mazanikov M, Salminen U-S, Meinberg M, Vähäsilta T, Petäjä L, Raivio P, Juvonen T, Pettilä V (2022) Effect of 4% albumin solution vs ringer acetate on major adverse events in patients undergoing cardiac surgery with cardiopulmonary bypass: a randomized clinical trial. JAMA 328:251–258. https://doi.org/10.1001/jama.2022.10461
SWEDEHEART Annual report 2023, issued in 2024. ISSN: 2000-1843. http://www.ucr.uu.se/swedeheart/
National Adult Cardiac Surgery Audit (NACSA) 2024 Summary Report. http://www.nicor.org.uk/national-cardiac-audit-programme/cardiac-surgery-audit-nacsa
Mundy J, Seevanayagam S, Williams-Spence J, Tran L, Solman N, McLaren J, Marrow N, Reid C. The Australian and New Zealand Society of Cardiac and Thoracic Surgeons’ Cardiac Surgery Database Program Annual Report 2022 Second Edition. Monash University, School of Public Health and Preventive Medicine, December 2023. Report No 16, 93 pages.
Beckmann A, Meyer R, Lewandowski J, Markewitz A, Blaßfeld D, Böning A (2023) German heart surgery report 2022: the annual updated registry of the German society for thoracic and cardiovascular surgery. Thorac Cardiovasc Surg 71:340–355. https://doi.org/10.1055/s-0043-1769597
Kim KM, Arghami A, Habib R, Daneshmand MA, Parsons N, Elhalabi Z, Krohn C, Thourani V, Bowdish ME (2023) The society of thoracic surgeons adult cardiac surgery database: 2022 update on outcomes and research. Ann Thorac Surg 115:566–574. https://doi.org/10.1016/j.athoracsur.2022.12.033
Finfer S, Micallef S, Hammond N, Navarra L, Bellomo R, Billot L, Delaney A, Gallagher M, Gattas D, Li Q, Mackle D, Mysore J, Saxena M, Taylor C, Young P, Myburgh J (2022) Balanced multielectrolyte solution versus saline in critically ill adults. N Engl J Med 386:815–826. https://doi.org/10.1056/NEJMoa2114464
Grant MC, Crisafi C, Alvarez A, Arora RC, Brindle ME, Chatterjee S, Ender J, Fletcher N, Gregory AJ, Gunaydin S, Jahangiri M, Ljungqvist O, Lobdell KW, Morton V, Reddy VS, Salenger R, Sander M, Zarbock A, Engelman DT (2024) perioperative care in cardiac surgery: a joint consensus statement by the enhanced recovery after surgery (ERAS) cardiac society, ERAS international society, and the society of thoracic surgeons (STS). Ann Thorac Surg 117:669–689. https://doi.org/10.1016/j.athoracsur.2023.12.006
Acknowledgements
The HAS FLAIR-II investigators: Leah Peck (Research coordinator, Critical Care Registered Nurse, GradCert(CritCareNurs)), Helen Young (Research coordinator, Masters of Nursing, GradDip(Midwifery), GradDip(CritCare), BN), Will Dovenya, Xu K, Akinori Maeda, Ke Xu, Sofia Spano, Fumitaka Yanase and Helen Young, Austin Hospital, Melbourne, Victoria, Australia. Michelle Horton, Stephanie Pearce, Paul Power and Jemma Trickey, Barwon Health, Geelong, Victoria, Australia. Deborah Barge, Kathleen Byrne, Michael Haeusler, Chris MacIsaac and Madeleina Snowdon, The Royal Melbourne Hospital, Melbourne, Victoria, Australia. Additional contributions: we thank Carol Hodgson, Jamie Cooper, Jess Kasza and Cameron Patrick, for participation in the trial data safety monitoring committee.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This study was supported by CSL Behring, which is a manufacturer of albumin solution products. CSL Behring participated in the design of pharmacovigilance surveillance; otherwise, it did not participate in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, or approval of the manuscript; or decision to submit the manuscript for publication. GJW was supported by a NHMRC Postgraduate scholarship.
Author information
Authors and Affiliations
Consortia
Contributions
GJW had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: GJW, AMD, JJP and RB. Acquisition, analysis, or interpretation of data: Wigmore, Eastwood, Serpa Neto, Peck, Young, Yanase, Spano, Maeda, Dovenya,Xu, Maiden, Bihari, Baker, Bennetts, Ghanpur, Anstey, Deane, Presneill, Raman, Bellomo. Drafting of the manuscript: Wigmore, Deane, Presneill, Eastwood, Serpa Neto, Maiden, Bihari, Baker, Bennetts, Ghanpur, Anstey, Raman, Bellomo. Critical revision of the manuscript for important intellectual content: Wigmore, Deane, Presneill, Eastwood, Serpa Neto, Maiden, Bihari, Baker, Bennetts, Ghanpur, Anstey, Raman, Bellomo. Statistical analysis: Wigmore, Serpa Neto, Presneill, Bellomo. Obtained funding: Bellomo. Administrative, technical, or material support: Wigmore, Deane, Presneill, Eastwood, Serpa Neto, Maiden, Bihari, Ghanpur, Anstey, Raman, Bellomo. Supervision: Wigmore, Deane, Presneill, Bellomo.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The HAS FLAIR-II investigators are listed in the acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wigmore, G.J., Deane, A.M., Presneill, J.J. et al. Twenty percent human albumin solution fluid bolus administration therapy in patients after cardiac surgery-II: a multicentre randomised controlled trial. Intensive Care Med (2024). https://doi.org/10.1007/s00134-024-07488-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00134-024-07488-3