Abstract
Purpose
Extracorporeal membrane oxygenation (ECMO) use for severe coronavirus disease 2019 (COVID-19) patients has increased during the course of the pandemic. As uncertainty existed regarding patient’s outcomes, early guidelines recommended against establishing new ECMO centers. We aimed to explore the epidemiology and outcomes of ECMO for COVID-19 related cardiopulmonary failure in five countries in the Middle East and India and to evaluate the results of ECMO in 5 new centers.
Methods
This is a retrospective, multicenter international, observational study conducted in 19 ECMO centers in five countries in the Middle East and India from March 1, 2020, to September 30, 2020. We included patients with COVID-19 who received ECMO for refractory hypoxemia and severe respiratory acidosis with or without circulatory failure. Data collection included demographic data, ECMO-related specific data, pre-ECMO patient condition, 24 h post-ECMO initiation data, and outcome. The primary outcome was survival to home discharge. Secondary outcomes included mortality during ECMO, survival to decannulation, and outcomes stratified by center type.
Results
Three hundred and seven COVID-19 patients received ECMO support during the study period, of whom 78 (25%) were treated in the new ECMO centers. The median age was 45 years (interquartile range IQR 37–52), and 81% were men. New center patients were younger, were less frequently male, had received higher PEEP, more frequently inotropes and prone positioning before ECMO and were less frequently retrieved from a peripheral center on ECMO. Survival to home discharge was 45%. In patients treated in new and established centers, survival was 55 and 41% (p = 0.03), respectively. Multivariable analysis retained only a SOFA score < 12 at ECMO initiation as associated with survival (odds ratio, OR 1.93 (95% CI 1.05–3.58), p = 0.034), but not treatment in a new center (OR 1.65 (95% CI 0.75–3.67)).
Conclusions
During pandemics, ECMO may provide favorable outcomes in highly selected patients as resources allow. Newly formed ECMO centers with appropriate supervision of regional experts may have satisfactory results.
Similar content being viewed by others
In this multicenter international cohort in 19 ECMO centers from five countries in the Middle East and India, 307 critically ill COVID-19 patients received ECMO therapy, of whom 138 (45%) survived to home discharge. The current study showed that new satellite ECMO centers could be safely implemented with appropriate close supervision of regional experts and may provide favorable outcomes in highly selected critically ill patients |
Introduction
Extracorporeal membrane oxygenation (ECMO) is a complex, labor-intensive, and high-risk intervention that may be considered for patients with acute severe respiratory and cardiac failure [1,2,3,4,5]. Early during the coronavirus disease 2019 (COVID-19) pandemic, several guidelines suggested considering ECMO for selected patients with respiratory and cardiac failure refractory to conventional therapies [6, 7]. Some of these guidelines recommended against establishing new ECMO centers [8]. However, with a better understanding of the disease and the increasing need for ECMO in regions that lacked this service, the updated version of the recommendation on this topic was less stringent, allowing for the creation of new ECMO centers in selected cases [9]. During the current pandemic, several case series and large cohort registries were published and discussed ECMO provision and utility [10,11,12,13,14,15,16]. The objective of this study was to report the regional epidemiology and outcomes of COVID-19 patients receiving ECMO therapy in the South Asia, West Asia, and Africa Chapter of Extracorporeal Life Support Organization (SWAAC-ELSO) region [17] and to evaluate the results of ECMO implemented in new centers.
Methods
Study design
This was a retrospective, multicenter international, observational study. We included COVID-19 patients who received ECMO between 1 March 2020, and 30 September 2020. After the SWAAC ELSO steering committee's authorization, IRB approval was obtained from the coordinating center King Saud Medical City in Riyadh. The country representatives obtained IRB approval for each participating center as well.
Settings
The study was conducted in 19 ECMO centers in five countries of the SWAAC ELSO region. These countries included Saudi Arabia, Qatar, Kuwait, Egypt, and India, which had 14 established ECMO centers prior to the pandemic and five new centers instituted during the pandemic. Of the 14 established centers, 4 were high-volume centers managing more than 20 ECMO patients per year before the pandemic. New centers were defined as those who started ECMO services after January 2020 to cover the demand of COVID-19 patients with severe acute respiratory failure and/or acute severe cardiac failure in area that lacked this service in select cases with appropriate close supervision of regional experts. Physicians, perfusionists and nurses who had already been trained in ECMO under the close supervision of established ECMO centers provided the required training, following ELSO guidelines and using ELSO education ELSOed (previously ECMOed) [18] or equivalent material. Most of these new centers were established in tertiary hospitals with prior experience in managing severe acute respiratory distress syndrome (ARDS). A maximum of two ECMO runs were allowed simultaneously. Patient selection was carried out by national ECMO experts through a central command telemedicine system explicitly designed for COVID-19 operational management. In new centers, the ECMO machines were monitored by an in-house perfusionist with previous ECMO experience and training, while the nurse-to-patient ratio was 1:1. The medical staff included in-house trained intensivists, and on-call critical care consultants with previous ECMO experience. Ultrasound-guided ECMO cannulation was performed by cardiothoracic surgeons or intensivists with previous experience and training. For the most severe patients treated at non-ECMO centers, an ECMO retrieval team was activated to initiate ECMO and to transport patients to an established or a new ECMO center. The participating centers included both ELSO and non-ELSO affiliated centers.
Patients
We included all consecutive COVID-19 patients admitted and treated in the participating centers with venovenous or venoarterial ECMO for acute respiratory or circulatory failure.
Data collection
Data collection included demographic data, patient comorbidities, sepsis-related organ failure assessment (SOFA) score [19], Murray Score [20], ECMO configuration, complications during ECMO, pre-ECMO patient condition, 24 h post-ECMO initiation data, ECMO run time, and outcomes (survival to ECMO weaning, home discharge). We stratified the cohort into two groups, based on whether they received ECMO in established or new centers.
Outcomes measures
The primary outcome was survival to home discharge. Secondary outcomes included survival during ECMO support and survival to ECMO decannulation. Major bleeding was defined as bleeding that required blood transfusion and/or required surgical intervention, and Infection was defined as positive culture result of blood, tracheal aspirate and cannula sites.
Statistical analysis
Continuous variables were reported as medians and interquartile ranges and were compared using the Wilcoxon rank-sum test. Categorical variables were reported as frequencies and percentages and were compared using χ2 or Fisher’s exact test. Ordinal variables were compared using the Kruskal–Wallis test. Kaplan–Meier curves were constructed to compare the effect of different variables on outcomes of interest. Binary logistic regression was then used to evaluate the influence of pre-ECMO and ECMO day 1 factors on the outcomes. Continuous variables were dichotomized using the median value. A multivariable logistic regression model was used to identify variables independently associated with survival after ECMO. Variables entered in the multivariable model were those with univariable value of p less than 0.10. We also included variables previously shown to be associated with survival after ECMO initiation in previous series of COVID and non-COVID ECMO patients [21]. The results were reported as odds ratio (OR) with a 95% confidence interval (CI). The Breusch–Pagan test of heteroskedasticity was applied to all logistic models to assess the inconsistency of variance across different centers (intra-class correlation). All statistical tests were two-tailed, and p values < 0.05 were considered significant. All statistical analyses were performed using R software, version 4.0.2 (06-22-2020) (R Foundation for Statistical Computing, Vienna, Austria).
Results
Patient characteristics and demographics
During the study period, 307 COVID-19 patients received ECMO at participating sites. Table 1 describes the characteristics of new and established centers. Demographic data and patient characteristics are provided in Table 2. Patients’ median age was 45 years (interquartile range, IQR 37–52), 81% were men, and 94% received venovenous ECMO. Prior to ECMO initiation, the median number of days with intubation and mechanical ventilation was 2.5 (IQR 1–5), PaO2/FiO2 ratio was 60 (IQR 52–68), Murray score was 3.5 (IQR 3.4–3.7), SOFA score was 12 (IQR 9–14), 58% of the patients had received vasopressors and 52% had received prone positioning (Table 2). The median PEEP and driving pressure before ECMO and on ECMO day 1 were 13 (IQR 10.5–15) and 8 (IQR 8–10) cm H2O and 20 (IQR 17–23) and 19 (IQR 14–20) cm H2O, respectively. Patients treated in new centers were younger, less frequently male, had received higher PEEP, more frequent inotropes, and more prone positioning before ECMO and were less frequently retrieved from a peripheral center on ECMO (Table 2).
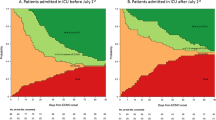
Outcomes and complications
138/307 (45%) patients were discharged home alive, while 178 (58%) patients survived ECMO (Table 3, Fig. 1). No therapeutic limitations were made in this series of patients. The home discharge survival rate of patients treated in new and established centers was 55 and 41%, p = 0.03, respectively (Table 3). However, this difference was no longer significant (OR 1.65 (95% CI 0.75–3.67)) after adjusting for confounders (Table 4). The median duration of ECMO support was 15 days. Complications included infections in 69.7% of patients; major bleeding in 23.8%, renal failure with renal replacement therapy in 31.9%, and pulmonary embolism in 4.9% of patients (Table 3).
Pre-ECMO predictors of survival
Table S1 reports the characteristics of survivors and non-survivors. Patients who survived had lower SOFA scores and less need for vasopressors at ECMO initiation. In addition, on ECMO day 1, survivors had lower plateau and driving pressures and higher respiratory system compliance with no difference in the level of PEEP. Multivariable analysis (Table 4) retained only a SOFA score < 12 at ECMO initiation as associated with survival (OR 1.93 (95% CI 1.05–3.58), p = 0.034).
Discussion
We report that the application of ECMO for COVID-19 led to an overall survival rate of 45% in a large series of patients treated in the SWAAC-ELSO region. Newly formed ECMO centers with appropriate supervision of regional experts had satisfactory results.
The published ELSO registry reported 1035 COVID-19 patients who received ECMO in 36 countries with an estimated cumulative incidence of 37.4% in-hospital mortality 90 days after ECMO initiation [22]. However, the actual day-90 mortality may markedly exceed the reported estimated mortality, since no data on long-term survival existed for many of these patients, with greater than 30% being discharged to another hospital or a long-term acute care or a rehabilitation center. Another published cohort from France by Schmidt et al. showed an estimated 31% probability of day-60 mortality [23]. While the outcome was promising, and comparable to non-COVID-19 respiratory ECMO as reported in the EOLIA trial [4], given the high experience of the centers reported by Schmidt and colleagues, observations’ generalizability of outcome may be limited. [24] The Steering Committee of the European chapter of the Extracorporeal Life Support Organization (Euro-ELSO) initiated prospective data collection of COVID-19 patients were supported on ECMO. The first 1531 cases were recently published, of whom 841 patients (55%) were weaned from ECMO with a reasonable 44% overall in-hospital mortality [25, 26]. Unlike these reports on severe COVID-19 patients on ECMO, our patients received all their care in one hospital, including rehabilitation and long-term care, making this cohort unique in reporting patient's final disposition. More recently, Lebreton et al. [27] reported the greater Paris experience during the COVID-19 pandemic, in which 138/302 (46%) patients were alive 90 days after ECMO initiation. Interestingly, patient pre-ECMO characteristics in this cohort were similar to those observed in our series and the other recently reported studies [28, 29].
In the COVID-19 ELSO registry, independent factors of mortality were temporary circulatory support (venoarterial ECMO support), increasing age, lower PaO2/FiO2, acute kidney injury, chronic respiratory insufficiency, an immunocompromised status, and pre-ECMO cardiac arrest [22]. In the latest report from the greater Paris ECMO group, factors associated with improved survival were younger age (≤ 48 vs. ≥ 57 years), a shorter time between intubation and initiation of ECMO, a lower renal component of the pre-ECMO SOFA scores, and a higher case volume for venovenous ECMO in the previous year (i.e., ≥ 30 ECMOs) [27]. While, in our series of patients, we evaluated many pre-ECMO patient-level factors and found that higher SOFA score, use of vasopressors before ECMO, and treatment in an established center were associated with higher mortality in the univariable analysis. Of note, higher plateau and driving pressures, higher PaCO2, and lower PaO2/FiO2 on ECMO day 1 were associated with higher mortality. The multivariable model only retained SOFA > 12 as independent predictor of mortality. Different case mixes of patients and variable clinical management both before and after ECMO may have contributed to the differences observed in predictors of the outcomes. Indeed, ventilator settings under ECMO may also strongly impact patient outcomes [30,31,32,33,34]. In our series, PEEP was markedly decreased after ECMO, while it was previously shown that a PEEP less than 12 cmH2O on the first days of ECMO was significantly associated with poorer survival [31]. Similarly, the driving pressure remained unchanged on ECMO, while a previous study suggested that it was the only ventilator setting after ECMO initiation with an independent association with in-hospital mortality [35]. Ultraprotective ventilation permitted by ECMO was, therefore, not applied in a sizeable proportion of our patients and might partly explain the observed lower survival rate compared to other cohorts of COVID-19 patients.
During the H1N1 pandemic new ECMO centers were established in the UK to respond to a surge of severe viral ARDS [36]. In preparedness for the anticipated surge of COVID-19 patients, an early initiative was made to start 5 new centers in key geographical areas. This initiative was fueled by the lack of ECMO capacity to cover the anticipated need of extracorporeal support and projected aviation transport restrictions. The thorough supervision and training provided by experienced ECMO physicians and more conservative selection criteria allowed these newly developed centers to flatten their learning curve. Our results showing satisfactory results after ECMO initiation in these newly formed centers are reassuring. Accordingly, the most recent ELSO guideline recommending starting new ECMO centers in selected cases and under appropriate supervision [9] is supported by our findings.
This study has important limitations. First, it is retrospective and included patients treated only in the Middle East and India. Second, we did not collect the number of eligible patients not initiated on ECMO. Third, we did not collect data regarding patient’s illness severity such as the RESP score, lung CT scan, ventilatory ratio, use of nitric oxide, viral load, specific COVID-19 treatments and other specific ECMO-specific data such as sweep gas flow, pump flow rate and cannula types. Fourth, the rate of prone positioning prior to ECMO was globally low (52%) in our patients and slightly lower in the established centres (49%) compared with the new centres (61%). It was lower compared with previous published large cohorts of COVID19 patients (94% for Schmidt et al. [22] and 61% for Barbaro et al. [23]). As such, we cannot exclude that some patients would have responded to prone positioning [37] and might have avoided ECMO and its associated complications. Finally, less patients were included in new centers than in established ones, and we cannot exclude that selection criteria might have differed between these centers.
In conclusion, ECMO may provide favorable outcomes in highly selected patients as resources allow during pandemics. In situations demanding the provision of new ECMO beds in geographically challenging areas and where trained specialists are available, newly formed ECMO centers with appropriate supervision of regional experts may have satisfactory results.
Availability of data and materials
AR and HM has full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the analysis and are willing to submit to external review of the data upon request.
Code availability
Code available upon request.
References
Combes A, Peek GJ, Hajage D, Hardy P, Abrams D, Schmidt M, Dechartres A, Elbourne D (2020) ECMO for severe ARDS: systematic review and individual patient data meta-analysis. Intensive Care Med 46(11):2048–2057. https://doi.org/10.1007/s00134-020-06248-3
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, Firmin RK, Elbourne D (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374(9698):1351–1363. https://doi.org/10.1016/s0140-6736(09)61069-2
Rabie AA, Asiri A, Rajab M et al (2021) Beyond frontiers: feasibility and outcomes of prolonged veno-venous extracorporeal membrane oxygenation in severe acute respiratory distress syndrome. ASAIO J 67(3):339–344. https://doi.org/10.1097/MAT.0000000000001367
Combes A, Hajage D, Capellier G, Demoule A, Lavoué S, Guervilly C, Da Silva D, Zafrani L, Tirot P, Veber B, Maury E, Levy B, Cohen Y, Richard C, Kalfon P, Bouadma L, Mehdaoui H, Beduneau G, Lebreton G, Brochard L, Ferguson ND, Fan E, Slutsky AS, Brodie D, Mercat A, EOLIA Trial Group, REVA, ECMONet (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med 378(21):1965–1975. https://doi.org/10.1056/NEJMoa1800385
Goligher EC, Tomlinson G, Hajage D et al (2018) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome and posterior probability of mortality benefit in a post hoc Bayesian analysis of a randomized clinical trial. JAMA 320(21):2251–2259. https://doi.org/10.1001/jama.2018.14276
Bartlett RH, Ogino MT, Brodie D et al (2020) Initial ELSO guidance document: ECMO for COVID-19 patients with severe cardiopulmonary failure. ASAIO J 66(5):472–474. https://doi.org/10.1097/MAT.0000000000001173
Alhazzani W, Møller MH, Arabi YM et al (2020) Surviving Sepsis Campaign: guidelines on the management of critically ill adults with Coronavirus Disease 2019 (COVID-19). Intensive Care Med 46(5):854–887. https://doi.org/10.1007/s00134-020-06022-5
Shekar K, Badulak J, Peek G et al (2020) ELSO Guideline Working Group. Extracorporeal Life Support Organization Coronavirus Disease 2019 interim guidelines: a consensus document from an International Group of interdisciplinary extracorporeal membrane oxygenation providers. ASAIO J 66(7):707–721. https://doi.org/10.1097/MAT.0000000000001193
JenelleBadulak M, Antonini V, Stead CM et al (2021) Updated 2021 guidelines from the extracorporeal life support organization. ASAIO J 67(5):485–495. https://doi.org/10.1097/MAT.0000000000001422
COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators (2020) Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med 47:60–73. https://doi.org/10.1007/s00134-020-06294-x
Alshahrani MS, Sindi A, Alshamsi F (2018) Extracorporeal membrane oxygenation for severe Middle East respiratory syndrome coronavirus. Ann Intensive Care 8(1):3. https://doi.org/10.1186/s13613-017-0350-x
MacLaren G, Fisher D, Brodie D (2020) Preparing for the most critically Ill patients with COVID-19: the potential role of extracorporeal membrane oxygenation. JAMA 323(13):1245–1246. https://doi.org/10.1001/JAMA.2020.2342
Ramanathan K, Antognini D, Combes A et al (2020) Planning and provision of ECMO services for severe ARDS during the COVID-19 Pandemic and other outbreaks of emerging infectious diseases. Lancet Respir Med 8(5):518–526. https://doi.org/10.1016/S2213-2600(20)30121-1
MacLaren G, Combes A, Brodie D (2021) What is new in ECMO for COVID-19? Intensive Care Med 47(1):107–109. https://doi.org/10.1007/s00134-020-06284-z
Mufti H, Bahudden H, Al Aseri Z, Azzam M (2020) Extracorporeal membrane oxygenation in COVID-19: the Saudi ECLS-Chapter perspective. Saudi Crit Care 4(4):115–118. https://doi.org/10.4103/sccj.sccj_55_20
Heinsar S, Peek GJ, Fraser JF (2020) ECMO during the COVID-19 Pandemic: when is it justified? Crit Care 24(1):650. https://doi.org/10.1186/s13054-020-03386-4
Pooboni S (2017) SWAC ELSO: past, present, and future. Qatar Med J. https://doi.org/10.5339/qmj.2017.swacelso.9
Zakhary B, Shekar K, Diaz R, Badulak J, Johnston L et al (2020) Extracorporeal Life Support Organization (ELSO) ECMOed Taskforce. Position Paper on Global Extracorporeal Membrane Oxygenation Education and Educational Agenda for the Future: a statement from the Extracorporeal Life Support Organization ECMOed Taskforce. Crit Care Med 48(3):406–414. https://doi.org/10.1097/CCM.0000000000004158
Vincent JL, Moreno R, Takala J, et al, On behalf of the Working Group on Sepsis Related Problems of the European Society of Intensive Care Medicine (1996) The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med 22(7):707–710. https://doi.org/10.1007/BF01709751
Murray JF, Matthay MA, Luce JM, Flick MR (1988) An expanded definition of the adult respiratory distress syndrome. Am Rev Respir Dis 138(3):720–723. https://doi.org/10.1164/ajrccm/138.3.720
Schmidt M, Bailey M, Sheldrake J, Hodgson C, Aubron C, Rycus PT, Scheinkestel C, Cooper DJ, Brodie D, Pellegrino V, Combes A, Pilcher D (2014) Predicting survival after extracorporeal membrane oxygenation for severe acute respiratory failure. The Respiratory Extracorporeal Membrane Oxygenation Survival Prediction (RESP) score. Am J Respir Crit Care Med 189(11):1374–1382. https://doi.org/10.1164/rccm.201311-2023OC
Barbaro RP, MacLaren G, Boonstra PS, Iwashyna TJ, Slutsky AS, Fan E, Bartlett RH, Tonna JE, Hyslop R, Fanning JJ, Rycus PT, Hyer SJ, Anders MM, Agerstrand CL, Hryniewicz K, Diaz R, Lorusso R, Combes A, Brodie D, Organization ELS (2020) Extracorporeal membrane oxygenation support in COVID-19: an international cohort study of the Extracorporeal Life Support Organization registry. Lancet. https://doi.org/10.1016/S0140-6736(20)32008-0
Schmidt M, Hajage D, Lebreton G et al (2020) Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome associated with COVID-19: a retrospective cohort study. Lancet Respir Med 8(11):1121–1131. https://doi.org/10.1016/S2213-2600(20)30328-3
Shekar K, Slutsky AS, Brodie D (2020) ECMO for severe ARDS associated with COVID-19: now we know we can, but should we? Lancet Respir Med 8:1066–1068
Lorusso R, Combes A, Coco VL et al (2021) ECMO for COVID-19 patients in Europe and Israel. Intensive Care Med 47:344–348. https://doi.org/10.1007/s00134-020-06272-3
Di Nardo M, Hoskote A, Thiruchelvam T et al (2020) EuroELSO Neonatal & Pediatric Working Group & Collaborators on COVID-19. Extracorporeal membrane oxygenation in children with COVID-19: preliminary report from the collaborative EuroELSO prospective survey. ASAIO J 67(2):121–124. https://doi.org/10.1097/MAT.0000000000001309
Lebreton G, Schmidt M et al (2021) Extracorporeal membrane oxygenation network organization and clinical outcomes during the COVID-19 pandemic in Greater Paris, France: a multicentre cohort study. Lancet Respir Med. https://doi.org/10.1016/S2213-2600(21)00096-5
Shaefi S, Brenner SK, Gupta S et al (2021) Extracorporeal membrane oxygenation in patients with severe respiratory failure from COVID-19. Intensive Care Med 47:208–221. https://doi.org/10.1007/s00134-020-06331-9
Diaz RA, Graf J, Zambrano JM et al (2021) ECMO for COVID-19-associated severe ARDS in Chile: a nationwide incidence and cohort study. Am J Respir Crit Care Med. https://doi.org/10.1164/rccm.202011-4166OC
Schmidt M, Stewart C et al (2015) Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome: a retrospective international multicenter study. Crit Care Med 43(3):654–664. https://doi.org/10.1097/CCM.0000000000000753
Pham T, Combes A et al (2013) Extracorporeal membrane oxygenation for pandemic influenza A(H1N1)-induced acute respiratory distress syndrome: a cohort study and propensity-matched analysis. Am J Respir Crit Care Med 187(3):276–285. https://doi.org/10.1164/rccm.201205-0815OC
Schmidt M, Pham T et al (2019) Mechanical ventilation management during extracorporeal membrane oxygenation for acute respiratory distress syndrome .An international multicenter prospective cohort. Am J Respir Crit Care Med 200(8):1002–1012. https://doi.org/10.1164/rccm.201806-1094OC
Combes A, Schmidt M, Hodgson CL, Fan E, Ferguson ND, Fraser JF, Jaber S, Pesenti A, Ranieri M, Rowan K, Shekar K, Slutsky AS, Brodie D (2020) Extracorporeal life support for adults with acute respiratory distress syndrome. Intensive Care Med. https://doi.org/10.1007/s00134-020-06290-1
Abrams D, Schmidt M, Pham T et al (2020) Mechanical ventilation for acute respiratory distress syndrome during extracorporeal life support. Research and practice. Am J Respir Crit Care Med 201(5):514–525. https://doi.org/10.1164/rccm.201907-1283CI
SerpaNeto A, Deliberato RO et al (2018) Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med 44(11):1914–1922. https://doi.org/10.1007/s00134-018-5375-6
Noah MA, Peek GJ, Finney SJ et al (2011) Referral to an extracorporeal membrane oxygenation center and mortality among patients with severe 2009 influenza A(H1N1). JAMA 306(15):1659–1668. https://doi.org/10.1001/jama.2011.1471
Guervilly C, Prud’homme E, Pauly V, Bourenne J, Hraiech S, Daviet F, Adda M, Coiffard B, Forel JM, Roch A, Persico N, Papazian L (2019) Prone positioning and extracorporeal membrane oxygenation for severe acute respiratory distress syndrome: time for a randomized trial? Intensive Care Med 45(7):1040–1042. https://doi.org/10.1007/s00134-019-05570-9
Acknowledgements
We would like to express our appreciation for the help and support of Faisal A. Alaklobi, MD Pediatric Infectious Disease & Infection Control, King Saud Medical City—KSA, Matthew Paden, MD. ELSO President-Elect (2020–2022), Associate Professor of Pediatric Critical Care-Emory University, Atlanta, Georgia, USA, Christine Stead, CEO-ELSO, Lakshmi Raman, Associate Professor of Pediatrics, Medical Director of ECMO, University of Texas Medical Center, Dallas, TX, Mark Ogino, ELSO past president (2020–2022), Dipanjan Chatterjee, Critical Care services Medica Superspecialty Hospital, Kolkata, Mohammad A. Alodat Chairman Critical Care Department, King Saud Medical City, Riyadh-KSA, Waleed Alatraby, Critical Care Department in King Saud Medical City-KSA and Mostafa Rajab, Critical Care services in Prince Mohamed bin Abdelaziz hospital-KSA, Abdullah K Alcharif, MD, USA.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
Design conception: AR, MA, AAF, AK, A, IFH, KS, DB, and BZ. Data collection and validation: AR, MA, AAF, AK, A, IFH, AC, PO, AE, HAF, AB, A, and HM. Statistical analysis: HM. Acquisition, analysis, or interpretation of data: all authors. Drafting of the manuscript: AR, writing and editing: AR, AC, MA, AAF, KS, SB, HM, DB, JB, PO, AE, SB, and YA. Critical revision of the manuscript for important intellectual content, final review, and approval: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
KS acknowledges research support from the Metro North Hospital and Health Service and the Prince Charles Hospital Foundation. DB receives research support from ALung Technologies. He has been on the medical advisory boards for Baxter, Abiomed, Xenios, and Hemovent and is the President-Elect of the Extracorporeal Life Support Organization (ELSO). AC reported receiving grants and personal fees from Maquet, Xenios, and Baxter and serving as the recent past president of the EuroELSO organization. Other authors have no conflict of interest.
Ethics approval
IRB approval was obtained from the coordinating center King Saud Medical City in Riyadh, Saudi Arabia. The country representatives obtained IRB approval for each center.
Consent to participate
Waived as all data are unidentified.
Consent for publication
All authors accept and confirmed publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Rabie, A.A., Azzam, M.H., Al-Fares, A.A. et al. Implementation of new ECMO centers during the COVID-19 pandemic: experience and results from the Middle East and India. Intensive Care Med 47, 887–895 (2021). https://doi.org/10.1007/s00134-021-06451-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-021-06451-w