Abstract
Purpose
The shortage of organs for transplantation is an important medical and societal problem because transplantation is often the best therapeutic option for end-stage organ failure.
Methods
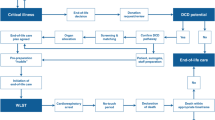
We review the potential deceased organ donation pathways in adult ICU practice, i.e. donation after brain death (DBD) and controlled donation after circulatory death (cDCD), which follows the planned withdrawal of life-sustaining treatments (WLST) and subsequent confirmation of death using cardiorespiratory criteria.
Results
Strategies in the ICU to increase the number of organs available for transplantation are discussed. These include timely identification of the potential organ donor, optimization of the brain-dead donor by aggressive management of the physiological consequence of brain death, implementation of cDCD protocols, and the potential for ex vivo perfusion techniques.
Conclusions
Organ donation should be offered as a routine component of the end-of-life care plan of every patient dying in the ICU where appropriate, and intensivists are the key professional in this process.


Similar content being viewed by others
References
Lesieur O, Leloup M, Gonzalez F, Mamzer M-F (2014) Eligibility for organ donation following end-of-life decisions: a study performed in 43 French intensive care units. Intensive Care Med. doi:10.1007/s00134-014-3409-2
Frontera JA, Curtis JR, Nelson JE et al (2015) Integrating palliative care into the care of neurocritically ill patients. Crit Care Med. doi:10.1097/CCM.0000000000001131
Domínguez-Gil B, Murphy P, Procaccio F (2015) Ten changes that could improve organ donation in the intensive care unit. Intensive Care Med. doi:10.1007/s00134-015-3833-y
Da Silva IRF, Frontera JA (2015) Worldwide barriers to organ donation. JAMA Neurol 72:112–118. doi:10.1001/jamaneurol.2014.3083
Wahlster S, Wijdicks EFM, Patel PV et al (2015) Brain death declaration: practices and perceptions worldwide. Neurology 84:1870–1879. doi:10.1212/WNL.0000000000001540
Wijdicks EFM, Varelas PN, Gronseth GS et al (2010) Evidence-based guideline update: determining brain death in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 74:1911–1918. doi:10.1212/WNL.0b013e3181e242a8
Wijdicks EFM (2002) Brain death worldwide: accepted fact but no global consensus in diagnostic criteria. Neurology 58:20–25
Citerio G, Crippa IA, Bronco A et al (2014) Variability in brain death determination in Europe: looking for a solution. Neurocrit Care 21:376–382. doi:10.1007/s12028-014-9983-x
Greer DM, Varelas PN, Haque S, Wijdicks EFM (2008) Variability of brain death determination guidelines in leading US neurologic institutions. Neurology 70:284–289. doi:10.1212/01.wnl.0000296278.59487.c2
Shappell CN, Frank JI, Husari K et al (2013) Practice variability in brain death determination: a call to action. Neurology 81:2009–2014. doi:10.1212/01.wnl.0000436938.70528.4a
Powner DJ, Hernandez M, Rives TE (2004) Variability among hospital policies for determining brain death in adults. Crit Care Med 32:1284–1288
Hornby K, Shemie SD, Teitelbaum J, Doig C (2006) Variability in hospital-based brain death guidelines in Canada. Can J Anaesth 53:613–619. doi:10.1007/BF03021854
Citerio G, Murphy PG (2015) Brain death: the European perspective. Semin Neurol 35:139–144. doi:10.1055/s-0035-1547533
Haupt WF, Rudolf J (1999) European brain death codes: a comparison of national guidelines. J Neurol 246:432–437
Scott JB, Gentile MA, Bennett SN et al (2013) Apnea testing during brain death assessment: a review of clinical practice and published literature. Respir Care 58:532–538. doi:10.4187/respcare.01962
Shemie SD, Hornby L, Baker A et al (2014) International guideline development for the determination of death. Intensive Care Med 40:788–797. doi:10.1007/s00134-014-3242-7
Shemie S, Baker A (2015) Uniformity in brain death criteria. Semin Neurol 35:162–168. doi:10.1055/s-0035-1547538
Shemie SD, Baker A (2014) Where have we been? Where are we going? Initiatives to improve uniformity of policies, integrity of practice, and improve understanding of brain death within the global medical community and lay public. J Crit Care 29:1114–1116. doi:10.1016/j.jcrc.2014.08.007
Gries CJ, White DB, Truog RD et al (2013) An Official American Thoracic Society/International Society for Heart and Lung Transplantation/Society of Critical Care Medicine/Association of Organ and Procurement Organizations/United Network of Organ Sharing Statement: ethical and policy considerations in organ donation after circulatory determination of death. Am J Respir Crit Care Med 188:103–109. doi:10.1164/rccm.201304-0714ST
Dalal AR (2015) Philosophy of organ donation: review of ethical facets. World J Transpl 5:44–51. doi:10.5500/wjt.v5.i2.44
Shaw D (2015) Organ donation is the right decision: a delicate truth. Intensive Care Med. doi:10.1007/s00134-015-3891-1
Shemie SD (2007) Clarifying the paradigm for the ethics of donation and transplantation: was “dead” really so clear before organ donation? Philos Ethics Humanit Med 2:18. doi:10.1186/1747-5341-2-18
Sixty-Third World Health Assembly World Health Organization (2010) WHO guiding principles on human cell, tissue and organ transplantation. Cell Tissue Bank 11:413–419
Steinbrook R (2007) Organ donation after cardiac death. N Engl J Med 357:209–213. doi:10.1056/NEJMp078066
Bernat JL (2008) The boundaries of organ donation after circulatory death. N Engl J Med 359:669–671. doi:10.1056/NEJMp0804161
Morrissey PE, Monaco AP (2014) Donation after circulatory death: current practices, ongoing challenges, and potential improvements. Transplantation 97:258–264. doi:10.1097/01.TP.0000437178.48174.db
Domínguez-Gil B, Haase-Kromwijk B, Van Leiden H et al (2011) Current situation of donation after circulatory death in European countries. Transpl Int 24:676–686. doi:10.1111/j.1432-2277.2011.01257.x
Borry P, Van Reusel W, Roels L, Schotsmans P (2008) Donation after uncontrolled cardiac death (uDCD): a review of the debate from a European perspective. J Law Med Ethics 36:752–759. doi:10.1111/j.1748-720X.2008.00334.x
Bernat JL, Bleck TP, Blosser SA et al (2014) Circulatory death determination in uncontrolled organ donors: a panel viewpoint. Ann Emerg Med 63:384–390. doi:10.1016/j.annemergmed.2013.05.018
Simpkin AL, Robertson LC, Barber VS, Young JD (2009) Modifiable factors influencing relatives’ decision to offer organ donation: systematic review. BMJ 338:b991–b991. doi:10.1136/bmj.b991
Singbartl K, Murugan R, Kaynar AM et al (2011) Intensivist-led management of brain-dead donors is associated with an increase in organ recovery for transplantation. Am J Transpl 11:1517–1521. doi:10.1111/j.1600-6143.2011.03485.x
Bastami S, Matthes O, Krones T, Biller-Andorno N (2013) Systematic review of attitudes toward donation after cardiac death among healthcare providers and the general public. Crit Care Med 41:897–905. doi:10.1097/CCM.0b013e31827585fe
Manara AR, Murphy PG, O’Callaghan G (2011) Donation after circulatory death. Br J Anaesth 108:i108–i121. doi:10.1093/bja/aer357
Souter MJ, Blissitt PA, Blosser S et al (2015) Recommendations for the critical care management of devastating brain injury: prognostication, psychosocial, and ethical management. Neurocrit Care 23:4–13. doi:10.1007/s12028-015-0137-6
Mark NM, Rayner SG, Lee NJ, Curtis JR (2015) Global variability in withholding and withdrawal of life-sustaining treatment in the intensive care unit: a systematic review. Intensive Care Med. doi:10.1007/s00134-015-3810-5
Sprung CL, Cohen SL, Sjokvist P et al (2003) End-of-life practices in European intensive care units: the Ethicus Study. JAMA 290:790–797. doi:10.1001/jama.290.6.790
Patel S, Martin JR, Marino PS (2014) Donation after circulatory death. Crit Care Med 42:2219–2224. doi:10.1097/CCM.0000000000000511
Algahim MF, Love RB (2015) Donation after circulatory death. Current Opinion Organ Transpl 20:1–6. doi:10.1097/MOT.0000000000000179
McKeown DW, Bonser RS, Kellum JA (2011) Management of the heartbeating brain-dead organ donor. Br J Anaesth 108:i96–i107. doi:10.1093/bja/aer351
Youn TS, Greer DM (2014) Brain death and management of a potential organ donor in the intensive care unit. Crit Care Clin 30:813–831. doi:10.1016/j.ccc.2014.06.010
Smith M (2004) Physiologic changes during brain stem death-lessons for management of the organ donor. J Heart Lung Transpl 23:S217–S222. doi:10.1016/j.healun.2004.06.017
Kotloff RM, Blosser S, Fulda GJ et al (2015) Management of the potential organ donor in the ICU: Society of Critical Care Medicine/American College of Chest Physicians/Association of Organ Procurement Organizations consensus statement. Crit Care Med 43:1291–1325. doi:10.1097/CCM.0000000000000958
Al-Khafaji A, Elder M, Lebovitz DJ et al (2015) Protocolized fluid therapy in brain-dead donors: the multicenter randomized MOnIToR trial. Intensive Care Med. doi:10.1007/s00134-014-3621-0
Greer DM, Valenza F, Citerio G (2015) Improving donor management and transplantation success: more research is needed. Intensive Care Med. doi:10.1007/s00134-015-3661-0
Dupuis S, Amiel J-A, Desgroseilliers M et al (2014) Corticosteroids in the management of brain-dead potential organ donors: a systematic review. Br J Anaesth 113:346–359. doi:10.1093/bja/aeu154
Pinsard M, Ragot S, Mertes PM et al (2014) Interest of low-dose hydrocortisone therapy during brain-dead organ donor resuscitation: the CORTICOME study. Crit Care 18:R158. doi:10.1186/cc13997
Macdonald PS, Aneman A, Bhonagiri D et al (2012) A systematic review and meta-analysis of clinical trials of thyroid hormone administration to brain dead potential organ donors. Crit Care Med 40:1635–1644. doi:10.1097/CCM.0b013e3182416ee7
Mascia L, Mastromauro I, Viberti S et al (2009) Management to optimize organ procurement in brain dead donors. Minerva Anestesiol 75:125–133. doi:10.2147/CLEP.S71403
Mascia L, Pasero D, Slutsky AS et al (2010) Effect of a lung protective strategy for organ donors on eligibility and availability of lungs for transplantation: a randomized controlled trial. JAMA 304:2620–2627. doi:10.1001/jama.2010.1796
Niemann CU, Feiner J, Swain S et al (2015) Therapeutic hypothermia in deceased organ donors and kidney-graft function. N Engl J Med 373:405–414. doi:10.1056/NEJMoa1501969
Dikdan GS, Mora-Esteves C, Koneru B (2012) Review of randomized clinical trials of donor management and organ preservation in deceased donors. Transplantation. doi:10.1097/TP.0b013e3182547537
Dhital KK, Iyer A, Connellan M et al (2015) Adult heart transplantation with distant procurement and ex vivo preservation of donor hearts after circulatory death: a case series. Lancet. doi:10.1016/S0140-6736(15)60038-1
Cypel M, Yeung JC, Liu M et al (2011) Normothermic ex vivo lung perfusion in clinical lung transplantation. N Engl J Med 364:1431–1440. doi:10.1056/NEJMoa1014597
Cypel M, Yeung JC, Hirayama S et al (2008) Technique for prolonged normothermic ex vivo lung perfusion. J Heart Lung Transpl 27:1319–1325. doi:10.1016/j.healun.2008.09.003
Machuca TN, Mercier O, Collaud S et al (2015) Lung transplantation with donation after circulatory determination of death donors and the impact of ex vivo lung perfusion. Am J Transpl 15:993–1002. doi:10.1111/ajt.13124
Reeb J, Keshavjee S, Cypel M (2015) Expanding the lung donor pool: advancements and emerging pathways. Current Opinion Organ Transpl. doi:10.1097/MOT.0000000000000233
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflict of interest for this manuscript.
Additional information
All the authors have contributed equally to this work.
Take-home message: The shortage of organs for transplantation is an important medical and societal problem. Strategies in the ICU can increase the number of organ available for transplantation. These include: 1. optimizing the management of donors after brain death (DBD). 2. Implementing controlled DCD (cDCD). 3. Introducing a pathway for patients with devastating brain Injury (DBI).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Citerio, G., Cypel, M., Dobb, G.J. et al. Organ donation in adults: a critical care perspective. Intensive Care Med 42, 305–315 (2016). https://doi.org/10.1007/s00134-015-4191-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-015-4191-5