Abstract
Background
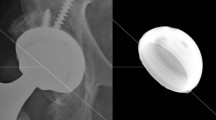
Despite continuous technical improvements, polyethylene wear debris induced periprosthetic osteolysis remains the main cause for failure of hip arthroplasty. Progressive oxidation of polyethylene was identified as another risk factor for material failure. To overcome this problem, antioxidants such as vitamin E (alpha-tocopherol) were supplemented by diffusion into the latest generation of polyethylene liners.
Objective
The purpose of the present study was to investigate the clinical outcome of patients treated with vitamin E blended highly cross-linked ultra-high molecular weight polyethylene liners (UHMWPE-XE) in comparison with conventional UHMWPE‑X liners by evaluating patient-reported outcome measures (PROM’s) at 3‑year follow-up.
Methods
A total of 143 patients were recruited into this prospective, randomized trial in our academic center. Three years after implantation, 101 patients were examined in the outpatient clinic for follow-up. Of these, 51 (50.5%) received UHMWPE-XE and 50 (49.5%) UHMWPE‑X liners. Clinical outcome was evaluated using Harris-Hip-Score (HHS) UCLA-Score and Hip Disability and Osteoarthritis Outcome Score (HOOS).
Results
There was a significant improvement in all PROM’s at one- and three-year follow-up compared to the status before implantation. PROM’s did not differ significantly between the first and third year follow-up. Both liner groups showed an equal clinical outcome.
Conclusion
The present study demonstrates that the supplementation of vitamin E to polyethylene liners is reliable and safe without showing higher complication rates compared with conventional polyethylene liners. The shortterm clinical outcome of vitamin E-blended (UHMWPE‑XE) is equivalent to those of conventional highly cross-linked polyethylene liners.
Zusammenfassung
Hintergrund
Trotz der stetigen Verbesserung der Materialeigenschaften bleibt die durch Abriebpartikel von Polyethylen im periprothetischen Gewebe induzierte aseptische Inflammation mit Osteoklastenaktivierung und aseptischer Prothesenlockerung eine der Hauptkomplikationen in der Hüftendoprothetik. Als weitere Gründe für den Materialverschleiß von Polyethylen wurden Oxidationsprozesse identifiziert. Zur Überwindung dieser Problematik, werden seit einigen Jahren hochvernetzte Polyethylen-Inlays hergestellt, die mit dem Antioxidans Tocopherol (Vitamin E) vorbehandelt werden. Das Ziel dieser Studie war es, die klinischen Ergebnisse von Patienten, denen Vitamin E “blended” bzw. konventionelle Polyethylen-Inlays in der Hüftendoprothetik implantiert wurden, anhand von PROM’s (patient related outcome measurements) zu bewerten.
Methoden
In unserem Zentrum wurden insgesamt 143 Patienten in diese prospektive, randomisierte Studie eingeschlossen. Zur 3‑Jahresnachuntersuchung kamen insgesamt 101 Patienten, von denen 51 ein Vitamin E vermischtes (50,5%) und 50 ein konventionelles (49,5%) Polyethylen-Inlay erhielten. Das klinische Ergebnis wurde anhand von Harris-Hip-Score (HHS) UCLA-Score und Hip Disability und Osteoarthritis Outcome Score (HOOS) bewertet.
Ergebnis
Es zeigte eine signifikante Verbesserung von allen PROM’s bei der 1-Jahresnachuntersuchung im Vergleich zum präoperativen Befund in beiden Kohorten. Die Ergebnisse verblieben auf hohem Niveau bei der 3-Jahresnachuntersuchung.
Schlussfolgerung
Die vorliegende Studie zeigt, dass der Einsatz von Vitamin E „blended“ Polyethylen-Inlays in der Hüftendoprothetik zuverlässig und sicher ist. Die klinischen Kurzzeitergebnisse sind denen von konventionellen Polyethylen-Inlays gleichwertig.





Similar content being viewed by others
Abbreviations
- ADL:
-
Activities of daily living
- ASA:
-
American Society of Anesthesiologists
- CoC:
-
Ceramic-on-ceramic
- HHS:
-
Harris hip score
- HOOS:
-
Hip disability and osteoarthritis outcome score
- HXLPE:
-
Highly cross-linked polyethylene
- MoM:
-
Metal-on-metal
- PROM:
-
Patient-reported outcome measures
- QOL:
-
Quality of life
- SD:
-
Standard deviation
- THA:
-
Total hip arthroplasty
- UCLA:
-
University of California Los Angeles
- UHMWPE:
-
Ultrahigh molecular weight polyethylene
- UHMWPE‑X:
-
Conventional cross-linked ultrahigh molecular weight polyethylene
- UHMWPE-XE:
-
Highly cross-linked ultrahigh molecular weight polyethylene
References
Clark CR, Heckman JD (2001) Volume versus outcomes in orthopaedic surgery: a proper perspective is paramount. J Bone Joint Surg Am 83-A(11):1619–1621
Gundtoft PH, Overgaard S, Schonheyder HC, Moller JK, Kjaersgaard-Andersen P, Pedersen AB (2015) The “true” incidence of surgically treated deep prosthetic joint infection after 32,896 primary total hip arthroplasties. Acta Orthop 86(3):326–334. https://doi.org/10.3109/17453674.2015.1011983
Beaulé PE, Campbell P, Mirra J, Hooper JC, Schmalzried TP (2001) Osteolysis in a cementless, second generation metal-on-metal hip replacement. Clin Orthop Relat Res 386:159–165
Haversath M, Klebingat S, VITAS-Gruppe, Jäger M (2018) Abriebanalyse mit virtuellen CAD-basierten Röntgenaufnahmen in der Endoprothetik. Orthopade 47(10):811–819. https://doi.org/10.1007/s00132-018-3602-z
Benignus C, Morlock M, Beckmann J (2019) Hüftendoprothetik beim jungen Patienten: Gleitpaarungen und Individualendoprothesen. Orthopade 48(4):292–299. https://doi.org/10.1007/s00132-019-03692-y
Tindall A, James KD, Slack R, James C, Shetty AA (2007) Long-term follow-up of a hydroxyapatite ceramic-coated threaded cup: an analysis of survival and fixation at up to 15 years. J Arthroplasty 22(8):1079–1082
Yoon PW, Yoo JJ, Kim Y, Yoo S, Lee S, Kim HJ (2016) The epidemiology and national trends of bearing surface usage in primary total hip Arthroplasty in korea. Clin Orthop Surg 8(1):29–37. https://doi.org/10.4055/cios.2016.8.1.29
Hwang KT, Kim YH, Kim YS, Choi IY (2013) Is second generation metal-on-metal primary total hip arthroplasty with a 28 mm head a worthy option?: a 12- to 18-year follow-up study. J Arthroplasty 28(10):1828–1833
Ha YC, Kim SY, Kim HJ, Yoo JJ, Koo KH (2007) Ceramic liner fracture after cementless alumina-on-alumina total hip arthroplasty. Clin Orthop Relat Res 458:106–110. https://doi.org/10.1097/blo.0b013e3180303e87
Jäger M, Wild A, Werner A, Munz D, Krauspe R (2002) Fracture analysis of a ceramic liner. Is in hip endoprosthesis replacement of ceramic on ceramic components with only one of the corresponding partners justified? Biomed Tech 47(12):306–309
Cobelli N, Scharf B, Crisi GM, Hardin J, Santambrogio L (2011) Mediators of the inflammatory response to joint replacement devices. Nat Rev Rheumatol 7(10):600–608
Jacobs CA, Christensen CP, Greenwald AS, McKellop H (2007) Clinical performance of highly cross-linked polyethylenes in total hip arthroplasty. J Bone Joint Surg Am 89(12):2779–2786
Puppulin L, Sugano N, Zhu W, Pezzotti G (2014) Structural modifications induced by compressive plastic deformation in single-step and sequentially irradiated UHMWPE for hip joint components. J Mech Behav Biomed Mater 31:86–99
Jäger M, van Wasen A, Warwas S, Landgraeber S, Haversath M, Group V (2014) A multicenter approach evaluating the impact of vitamin e‑blended polyethylene in cementless total hip replacement. Orthop Rev (Pavia) 6(2):5285. https://doi.org/10.4081/or.2014.5285
Sayeed SA, Mont MA, Costa CR, Johnson AJ, Naziri Q, Bonutti PM, Delanois RE (2011) Early outcomes of sequentially cross-linked thin polyethylene liners with large diameter femoral heads in total hip arthroplasty. Bull NYU Hosp Jt Dis 69(Suppl 1):S90–S94
Oral E, Malhi A, Muratoglu O (2006) Mechanisms of decrease in fatigue crack propagation resistance in irradiated and melted UHMWPE. Biomaterials 27:917–925
MacDonald D, Sakona A, Ianuzzi A et al (2011) Do first-generation highly crosslinked polyethylenes oxidize in vivo? Clin Orthop Relat Res 469:2278–2285
Wannomae KK, Christensen SD, Freiberg AA et al (2006) The effect of real-time aging on the oxidation and wear of highly crosslinked UHMWPE acetabular liners. Biomaterials 27:1980–1987
Currier BH, Van Citters DW, Currier JH, Collier JP (2010) In vivo oxidation in remelted highly cross-linked retrievals. J Bone Joint Surg Am 92:2409–2418
Jarrett BT, Cofske J, Rosenberg AE et al (2010) In vivo biological response to vitamin E and vitamin-E-doped polyethylene. J Bone Joint Surg Am 92:2672–2681
Oral E, Muratoglu OK (2011) Vitamin E diffused, highly crosslinked UHMWPE: a review. Int Orthop 35:215–223
Oral E, Wannomae KK, Rowell SL, Muratoglu OK (2006) Migration stability of alphatocopherol in irradiated UHMWPE. Biomaterials 27:2434–2439
Turner A, Okubo Y, Teramura S et al (2014) The antioxidant and non-antioxidant contributions of vitamin E in vitamin E blended ultra-high molecular weight polyethylene for total knee replacement. J Mech Behav Biomed Mater 31:21–30
Wolf C, Krivec T, Blassnig J et al (2002) Examination of the suitability of alpha-tocopherol as a stabilizer for ultra-high molecular weight polyethylene used for articulating surfaces in joint endoprostheses. J Mater Sci Mater Med 13:185–189
Wolf C, Macho C, Lederer K (2006) Accelerated ageing experiments with crosslinked and conventional ultra-high molecular weight polyethylene (UHMW-PE) stabilised with alpha-tocopherol for total joint arthroplasty. J Mater Sci Mater Med 17:1333–1340
Morlock MM, Jäger M (2017) Endoprothetik des älteren Menschen; Biomaterialien: Implantatwahl, Verankerungstechnik. Orthopade 46(1):4–17. https://doi.org/10.1007/s00132-016-3361-7
Oral E, Ghali BW, Rowell SL et al (2010) A surface crosslinked UHMWPE stabilized by vitamin E with low wear and high fatigue strength. Biomaterials 31:7051–7060
Kurtz SM, Dumbleton J, Siskey RS et al (2009) Trace concentrations of vitamin E protect radiation crosslinked UHMWPE from oxidative degradation. J Biomed Mater Res A 90:549–563
Grupp TM, Holderied M, Mulliez MA, Streller R, Jäger M, Blömer W, Utzschneider S (2014) Biotribology of a vitamin E‑stabilized polyethylene for hip arthroplasty - Influence of artificial ageing and third-body particles on wear. Acta Biomater 10(7):3068–3078. https://doi.org/10.1016/j.actbio.2014.02.052
Bracco P, Oral E (2011) Vitamin E‑stabilized UHMWPE for total joint implants: a review. Clin Orthop Relat Res 469:2286–2293
Parth M, Aust N, Lederer K (2002) Studies on the effect of electron beam radiation on the molecular structure of ultra-high molecular weight polyethylene under the influence of alpha-tocopherol with respect to its application in medical implants. J Mater Sci Mater Med 13(10):917–921
Oral E, Greenbaum E, Malhi A, Muratoglu O (2005) Characterization of blends of α‑Tocopherol with UHMWPE. Biomaterials 26:6657–6663
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51:737–755
Nilsdotter AK, Lohmander LS, Klassbo M, Roos EM (2003) Hip disability and osteoarthritis outcome score (HOOS)--validity and responsiveness in total hip replacement. BMC Musculoskelet Disord 4:10
Rahman WA, Garbuz DS, Masri BA (2013) Total hip arhtroplasty in steroid-induced osteonecrosis: early functional and radiological outcomes. Can J Surg 56:41–46
Amstutz HC, Thomas BJ, Jinnah R et al (1984) Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J Bone Joint Surg Am 66:228–241
Canadian Joint Replacement Registry (2008) Hip and knee replacements in Canada. 2008 annual report. Canadian Institute for Health Information c2009, Ottawa – Ontario
Oral E, Muratoglu OK (2011) Vitamin E diffused, highly crosslinked UHMWPE: a review. Int Orthop 35(2):215–223. https://doi.org/10.1007/s00264-010-1161-y
Hodrick J, Severson E, McAlister D, Dahl B, Hofmann A (2008) Highly crosslinked polyethylene is safe fro use in total knee arthroplasty. Clin Orthop Relat Res 466:2806–2812. https://doi.org/10.1007/s11999-008-0472-4
Manning DW, Chiang PP, Martell JM, Galante JO, Harris WH (2005) In vivo comparative wear study of traditional and highly cross-linked polyethylene in total hip arthroplasty. J Arthroplasty 20(7):880–886. https://doi.org/10.1016/j.arth.2005.03.033
Sutula LC, Collier JP, Saum KA, Currier BH, Currier JH, Sanford WM, Mayor MB, Wooding RE, Sperling DK, Williams IR, Kasprzak DJ, Surprenant VA (1995) The Otto Aufranc Award. Impact of gamma sterilization on clinical performance of polyethylene in the hip. Clin Orthop Relat Res 319:28–40. https://doi.org/10.1097/00003086-199510000-00004
Yamamoto K, Tateiwa T, Takahashi Y (2017) Vitamin E‑stabilized highly crosslinked polyethylenes: The role and effectiveness in total hip arthroplasty. J Orthop Sci 22(3):384–390. https://doi.org/10.1016/j.jos.2017.01.012
Nebergall AK, Greene ME, Laursen MB, Nielsen PT, Malchau H, Troelsen A (2017) Vitamin E diffused highly cross-linked polyethylene in total hip arthroplasty at five years: a randomised controlled trial using radiostereometric analysis. Bone Joint J 99-B(5):577–584. https://doi.org/10.1302/0301-620X.99B5.37521
Salemyr M, Muren O, Ahl T, Bodén H, Chammout G, Stark A, Sköldenberg O (2015) Vitamin‑E diffused highly cross-linked polyethylene liner compared to standard liners in total hip arthroplasty. A randomized, controlled trial. Int Orthop 39(8):1499–1505. https://doi.org/10.1007/s00264-015-2680-3
Wyatt M, Weidner J, Pfluger D, Beck M (2017) The RM Pressfit vitamys: 5‑year Swiss experience of the first 100 cups. Hip Int 27(4):368–372. https://doi.org/10.5301/hipint.5000469
Weiss RJ, Hailer NP, Stark A, Kärrholm J (2012) Survival of uncemented acetabular monoblock cups: evaluation of 210 hips in the Swedish Hip Arthroplasty Register. Acta Orthop 83(3):214–219. https://doi.org/10.3109/17453674.2012.688726
Sculco TP (2002) The acetabular component: an elliptical monoblock alternative. J Arthroplasty 17:118–120
Scemama C, Anract P, Dumaine V, Babinet A, Courpied JP, Hamadouche M (2017) Does vitamin E‑blended polyethylene reduce wear in primary total hip arthroplasty: a blinded randomised clinical trial. Int Orthop 41(6):1113–1118. https://doi.org/10.1007/s00264-016-3320-2
Otto-Lambertz C, Yagdiran A, Wallscheid F, Eysel P, Jung N (2017) Periprosthetic infection in joint replacement. Dtsch Arztebl Int 114(20):347–353. https://doi.org/10.3238/arztebl.2017.0347
Wetters NG, Murray TG, Moric M, Sporer SM, Paprosky WG, Della Valle CJ (2013) Risk factors for dislocation after revision total hip arthroplasty. Clin Orthop Relat Res 471:410–416
Karachalios T, Komnos G, Koutalos A (2018) Total hip arthroplasty: Survival and modes of failure. EFORT Open Rev 3(5):232–239. https://doi.org/10.1302/2058-5241.3.170068
Bozic KJ, Kurtz SM, Lau E, Ong K, Vail TP, Berry DJ (2009) The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am 91(1):128–133
Ullmark G (2016) The unstable total hip arthroplasty. Efort Open Rev 1(4):83–88. https://doi.org/10.1302/2058-5241.1.000022
Funding
The study is financially supported by B. Braun-Aesculap AG, Tuttlingen, Germany; trial registration: NCT01713062.
Members of the Vitas group
Jäger M (Klinik für Orthopädie, Unfall- und Wiederherstellungschirurgie, St. Marienhospital Mülheim, Contilia Gruppe für die Universität Duisburg-Essen, Germany), Landgraeber S, Serong S (Department of Orthopaedics, University of Saarland, Saarbrücken, Germany), Haversath M, von Wasen A (Department of Orthopaedics and Trauma Surgery, University of Duisburg-Essen, Essen, Germany), Windhagen H, Flörkemeier T, Budde S, Kubilay J, Noll Y (Klinik für Orthopädie, Diakovere Annastift, Medizinische Hochschule Hannover, Hannover, Germany), Delank KS, Baghdadi J (Klinik für Orthopädie und Unfallchirurgie, Universität Halle, Halle, Germany), Willburger R (Orthopädie und Unfallchirurgie, Katholisches Klinikum Bochum, Ruhr-Universität Bochum, Bochum, Germany), Dücker M (Klinik für Orthopädie, Marienhaus Klinikum St. Josef, Bendorf, Germany), Wilke A, Hütter F (Orthopädie, Unfall‑, Hand- und Wiederherstellungschirurgie, Elisabeth-Klinik, Bigge-Olsberg, Germany)
Author information
Authors and Affiliations
Consortia
Contributions
All authors ensured that they had furnished a substantial contribution to the article and that they are in agreement with the form and contents of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
A. Busch, M. Haversath, VITAS group, A. Wegner and M. Jäger declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. All patients consented to publish personal data in an anonymized form. The study was approved by the local ethics committee (11-4845-BO). The study was registered on Clinicaltrials.gov. (registration number NCT01713062).
Additional information
Availability of data and materials
All patient-related data were collected by file research from the archives of the participating centers.
All authors were fully involved in the study and preparation of the manuscript.
The members of the Vitas group are listed at the end of the article.
Rights and permissions
About this article
Cite this article
Busch, A., Jäger, M., VITAS group. et al. Vitamin E-blended versus conventional polyethylene liners in prostheses. Orthopäde 49, 1077–1085 (2020). https://doi.org/10.1007/s00132-019-03830-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-019-03830-6
Keywords
- Biomaterials
- Antioxidant
- Patient-related outcome measurement
- Total hip replacement
- Prosthesis durability