Abstract
Purpose
Mental health is shaped by social and economic contexts, which were altered during the COVID-19 pandemic. No study has systematically reviewed the literature on the relation between different assets and depression during the COVID-19 pandemic.
Methods
We conducted a systematic review of the literature on financial (e.g. income/savings), physical (e.g., home ownership), and social (e.g., marital status, educational attainment) assets and depression in U.S. adults. For each asset type, we created binary comparisons to report on the direction of the relationship and described if each study reported insignificant, positive, negative, or mixed associations.
Results
Among the 41 articles identified, we found that income was the most studied asset (n=34), followed by education (n=25), marital status (n=18), home ownership (n=5), and savings (n=4). 88%, 100%, and 100% of articles reported a significant association of higher income, home ownership, and higher savings, respectively, with less depression. The association between marital status and education with depression was more nuanced: 72% (13 of 18) studies showed that unmarried persons had greater risk of depression than married or cohabitating persons and 52% (13 of 25) of studies reported no significant difference in depression across educational groups.
Conclusion
This work adds to the literature a deeper understanding of how different assets relate to depression. In the context of largescale traumatic events, policies that maintain and protect access to social, physical, and financial assets may help to protect mental health.


Similar content being viewed by others
References
Breslau J, Finucane ML, Locker AR et al (2021) A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Prev Med 143:106362. https://doi.org/10.1016/j.ypmed.2020.106362
Ettman CK, Cohen GH, Abdalla SM et al (2022) Assets, stressors, and symptoms of persistent depression over the first year of the COVID-19 pandemic. Sci Adv 8:eabm9737. https://doi.org/10.1126/sciadv.abm9737
Cai C, Woolhandler S, Himmelstein DU, Gaffney A (2021) Trends in anxiety and depression symptoms during the COVID-19 pandemic: results from the US Census Bureau’s household pulse survey. J Gen Intern Med 36:1841–1843. https://doi.org/10.1007/s11606-021-06759-9
Ettman CK, Abdalla SM, Cohen GH et al (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open 3:e2019686. https://doi.org/10.1001/jamanetworkopen.2020.19686
Ettman CK, Cohen GH, Abdalla SM et al (2022) Persistent depressive symptoms during COVID-19: a national, population-representative, longitudinal study of U.S. adults. Lancet Reg Health Am 5:100091. https://doi.org/10.1016/j.lana.2021.100091
Twenge JM, McAllister C, Joiner TE (2021) Anxiety and depressive symptoms in U.S. Census Bureau assessments of adults: trends from 2019 to fall 2020 across demographic groups. J Anxiety Disord 83:102455. https://doi.org/10.1016/j.janxdis.2021.102455
Friedrich MJ (2017) Depression is the leading cause of disability around the world. JAMA 317:1517. https://doi.org/10.1001/jama.2017.3826
Greenberg PE, Fournier A-A, Sisitsky T et al (2021) The economic burden of adults with major depressive disorder in the United States (2010 and 2018). Pharmacoeconomics 39:653–665. https://doi.org/10.1007/s40273-021-01019-4
Kessler RC (2012) The costs of depression. Psychiatr Clin North Am 35:1–14. https://doi.org/10.1016/j.psc.2011.11.005
König H, König H-H, Konnopka A (2019) The excess costs of depression: a systematic review and meta-analysis. Epidemiol Psychiatr Sci 29:e30. https://doi.org/10.1017/S2045796019000180
Richmond-Rakerd LS, D’Souza S, Milne BJ et al (2021) Longitudinal associations of mental disorders with physical diseases and mortality among 2.3 million New Zealand citizens. JAMA Netw Open 4:e2033448. https://doi.org/10.1001/jamanetworkopen.2020.33448
Ettman CK, Abdalla SM, Cohen GH et al (2021) Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. J Epidemiol Commun Health 75:501–508. https://doi.org/10.1136/jech-2020-215213
Bask M, Bask M (2015) Cumulative (Dis)advantage and the Matthew effect in life-course analysis. PLoS ONE 10:e0142447. https://doi.org/10.1371/journal.pone.0142447
Park C, Rosenblat JD, Brietzke E et al (2019) Stress, epigenetics and depression: a systematic review. Neurosci Biobehav Rev 102:139–152. https://doi.org/10.1016/j.neubiorev.2019.04.010
Ettman CK, Adam GP, Clark MA et al (2022) Wealth and depression: a scoping review. Brain and Behavior 12:e2486. https://doi.org/10.1002/brb3.2486
Ettman CK, Cohen GH, Vivier PM, Galea S (2021) Savings, home ownership, and depression in low-income US adults. Soc Psychiatry Psychiatr Epidemiol 56:1211–1219. https://doi.org/10.1007/s00127-020-01973-y
Pollack CE, Chideya S, Cubbin C et al (2007) Should health studies measure wealth?: A systematic review. Am J Prev Med 33:250–264. https://doi.org/10.1016/j.amepre.2007.04.033
Abdalla SM, Galea S (2021) The 3-D commission: forging a transdisciplinary synthesis at the intersection of social determinants of health, data, and decision-making. J Urban Health 98:1–3. https://doi.org/10.1007/s11524-021-00555-w
Allen J, Balfour R, Bell R, Marmot M (2014) Social determinants of mental health. Int Rev Psychiatry 26:392–407. https://doi.org/10.3109/09540261.2014.928270
Compton MT, Shim RS (2015) The social determinants of mental health. FOC 13:419–425. https://doi.org/10.1176/appi.focus.20150017
Patel V, Burns JK, Dhingra M et al (2018) Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry 17:76–89. https://doi.org/10.1002/wps.20492
Muntaner C, Eaton WW, Miech R, O’Campo P (2004) Socioeconomic position and major mental disorders. Epidemiol Rev 26:53–62. https://doi.org/10.1093/epirev/mxh001
Ridley M, Rao G, Schilbach F, Patel V (2020) Poverty, depression, and anxiety: causal evidence and mechanisms. Science 370:eaay0214. https://doi.org/10.1126/science.aay0214
Assari S (2018) High income protects whites but not African Americans against risk of depression. Healthcare 6:37. https://doi.org/10.3390/healthcare6020037
Himmelstein KEW, Lawrence JA, Jahn JL et al (2022) Association between racial wealth inequities and racial disparities in longevity among US adults and role of reparations payments, 1992 to 2018. JAMA Netw Open 5:e2240519. https://doi.org/10.1001/jamanetworkopen.2022.40519
Derenoncourt E, Kim CH, Kuhn M, Schularick M (2022) Wealth of Two Nations: The U.S. Racial Wealth Gap, 1860–2020. National Bureau of Economic Research, Cambridge, MA
Wilkinson LR (2016) Financial strain and mental health among older adults during the great recession. J Gerontol Series B 71:745–754. https://doi.org/10.1093/geronb/gbw001
Tsai AC (2015) Home foreclosure, health, and mental health: a systematic review of individual, aggregate, and contextual associations. PLoS ONE 10:e0123182. https://doi.org/10.1371/journal.pone.0123182
Stimpson JP, Wilson FA, Peek MK (2012) Marital status, the economic benefits of marriage, and days of inactivity due to poor health. Int J Pop Res 2012:1–6. https://doi.org/10.1155/2012/568785
Dahmann SC, Schnitzlein DD (2019) No evidence for a protective effect of education on mental health. Soc Sci Med 241:112584. https://doi.org/10.1016/j.socscimed.2019.112584
Lorant V, Deliège D, Eaton W et al (2003) Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol 157:98–112. https://doi.org/10.1093/aje/kwf182
Singh A, Daniel L, Baker E, Bentley R (2019) Housing Disadvantage and poor mental health: a systematic review. Am J Prev Med 57:262–272. https://doi.org/10.1016/j.amepre.2019.03.018
Kawachi I, Adler NE, Dow WH (2010) Money, schooling, and health: mechanisms and causal evidence. Ann N Y Acad Sci 1186:56–68. https://doi.org/10.1111/j.1749-6632.2009.05340.x
Pearlin LI, Johnson JS (1977) Marital status, life-strains and depression. Am Sociol Rev 42:704–715. https://doi.org/10.2307/2094860
Kessler RC, Essex M (1982) Marital status and depression: the importance of coping resources. Soc Forces 61:484–507. https://doi.org/10.2307/2578238
Bulloch AGM, Williams JVA, Lavorato DH, Patten SB (2017) The depression and marital status relationship is modified by both age and gender. J Affect Disord 223:65–68. https://doi.org/10.1016/j.jad.2017.06.007
Grundström J, Konttinen H, Berg N, Kiviruusu O (2021) Associations between relationship status and mental well-being in different life phases from young to middle adulthood. SSM - Population Health 14:100774. https://doi.org/10.1016/j.ssmph.2021.100774
Sbarra DA, Emery RE, Beam CR, Ocker BL (2014) Marital dissolution and major depression in midlife: a propensity score analysis. Clin Psychol Sci 2:249–257. https://doi.org/10.1177/2167702613498727
Barnes DM, Bates LM (2017) Do racial patterns in psychological distress shed light on the black-white depression paradox? A systematic review. Soc Psychiatry Psychiatr Epidemiol 52:913–928. https://doi.org/10.1007/s00127-017-1394-9
Wallace BC, Small K, Brodley CE, et al (2012) Deploying an interactive machine learning system in an evidence-based practice center: abstrackr. In: Proceedings of the 2nd ACM SIGHIT International Health Informatics Symposium. Association for Computing Machinery, New York, NY, USA, pp 819–824
Rathbone J, Hoffmann T, Glasziou P (2015) Faster title and abstract screening? Evaluating Abstrackr, a semi-automated online screening program for systematic reviewers. Syst Rev 4:80. https://doi.org/10.1186/s13643-015-0067-6
Berkowitz SA, Basu S (2021) Unmet social needs and worse mental health after expiration of COVID-19 federal pandemic unemployment compensation. Health Aff 40:426–434. https://doi.org/10.1377/hlthaff.2020.01990
Birditt KS, Turkelson A, Fingerman KL et al (2021) Age differences in stress, life changes, and social ties during the COVID-19 pandemic: implications for psychological well-being. Gerontologist 61:205–216. https://doi.org/10.1093/geront/gnaa204
Czeisler MÉ, Lane RI, Petrosky E, et al (2020) Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 69:1049–1057. https://doi.org/10.15585/mmwr.mm6932a1
Daly M, Sutin AR, Robinson E (2020) Depression reported by US adults in 2017–2018 and March and April 2020. J Affect Disord 278:131–135. https://doi.org/10.1016/j.jad.2020.09.065
Daly M, Robinson E (2021) Psychological distress and adaptation to the COVID-19 crisis in the United States. J Psychiatr Res 136:603–609. https://doi.org/10.1016/j.jpsychires.2020.10.035
Hearne BN (2021) Psychological distress across intersections of race/ethnicity, gender, and marital status during the COVID-19 pandemic. Ethnicity Health. https://doi.org/10.1080/13557858.2021.1969537
Donnelly R, Farina MP (2021) How do state policies shape experiences of household income shocks and mental health during the COVID-19 pandemic? Soc Sci Med 269:113557. https://doi.org/10.1016/j.socscimed.2020.113557
Holingue C, Kalb LG, Riehm KE et al (2020) Mental distress in the United States at the beginning of the COVID-19 pandemic. Am J Public Health 110:1628–1634. https://doi.org/10.2105/AJPH.2020.305857
Holman EA, Thompson RR, Garfin DR, Silver RC (2020) The unfolding COVID-19 pandemic: a probability-based, nationally representative study of mental health in the United States. Sci Adv 6:eabd5390. https://doi.org/10.1126/sciadv.abd5390
Kantor BN, Kantor J (2020) Mental health outcomes and associations during the COVID-19 Pandemic: a cross-sectional population-based study in the United States. Front Psychiatry 11:569083. https://doi.org/10.3389/fpsyt.2020.569083
Kim HH-S, Laurence J (2020) COVID-19 restrictions and mental distress among American adults: evidence from Corona impact survey (W1 and W2). J Public Health 42:704–711. https://doi.org/10.1093/pubmed/fdaa148
Kim D (2021) Financial hardship and social assistance as determinants of mental health and food and housing insecurity during the COVID-19 pandemic in the United States. SSM Population Health 16:100862. https://doi.org/10.1016/j.ssmph.2021.100862
Lee H, Singh GK (2021) Monthly trends in self-reported health status and depression by race/ethnicity and socioeconomic status during the COVID-19 pandemic, United States, April 2020–May 2021. Ann Epidemiol 63:52–62. https://doi.org/10.1016/j.annepidem.2021.07.014
Lueck JA (2021) Help-seeking intentions in the U.S. population during the COVID-19 pandemic: examining the role of COVID-19 financial hardship, suicide risk, and stigma. Psychiatry Res 303:114069. https://doi.org/10.1016/j.psychres.2021.114069
Zhang W, Walkover M, Wu YY (2021) The challenge of COVID-19 for adult men and women in the United States: disparities of psychological distress by gender and age. Public Health 198:218–222. https://doi.org/10.1016/j.puhe.2021.07.017
McGinty EE, Presskreischer R, Han H, Barry CL (2022) Trends in psychological distress among US adults during different phases of the COVID-19 pandemic. JAMA Netw Open 5:e2144776. https://doi.org/10.1001/jamanetworkopen.2021.44776
McGinty EE, Presskreischer R, Han H, Barry CL (2020) Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA 324:93. https://doi.org/10.1001/jama.2020.9740
McGinty EE, Presskreischer R, Anderson KE et al (2020) Psychological distress and COVID-19–related stressors reported in a longitudinal cohort of US Adults in April and July 2020. JAMA 324:2555. https://doi.org/10.1001/jama.2020.21231
Nelson-Coffey SK, O’Brien MM, Braunstein BM et al (2021) Health behavior adherence and emotional adjustment during the COVID-19 pandemic in a US nationally representative sample: the roles of prosocial motivation and gratitude. Soc Sci Med 284:114243. https://doi.org/10.1016/j.socscimed.2021.114243
Park J, Kim B (2021) Associations of small business closure and reduced urban mobility with mental health problems in COVID-19 pandemic: a national representative sample study. J Urban Health 98:13–26. https://doi.org/10.1007/s11524-020-00511-0
Riehm KE, Holingue C, Smail EJ et al (2021) Trajectories of mental distress among U.S. adults during the COVID-19 Pandemic. Ann Behav Med 55:93–102. https://doi.org/10.1093/abm/kaaa126
Sances MW, Campbell AL (2021) State policy and mental health outcomes under COVID-19. J Health Polit Policy Law 46:811–830. https://doi.org/10.1215/03616878-9155991
Tham WW, Sojli E, Bryant R, McAleer M (2021) Common mental disorders and economic uncertainty: evidence from the COVID-19 pandemic in the U.S. PLoS ONE 16:e0260726. https://doi.org/10.1371/journal.pone.0260726
Wanberg CR, Csillag B, Douglass RP et al (2020) Socioeconomic status and well-being during COVID-19: a resource-based examination. J Appl Psychol 105:1382–1396. https://doi.org/10.1037/apl0000831
Das A, Singh P, Bruckner TA (2022) State lockdown policies, mental health symptoms, and using substances. Addict Behav 124:107084. https://doi.org/10.1016/j.addbeh.2021.107084
Wilson JM, Lee J, Shook NJ (2021) COVID-19 worries and mental health: the moderating effect of age. Aging Ment Health 25:1289–1296. https://doi.org/10.1080/13607863.2020.1856778
Topazian RJ, Levine AS, McGinty EE et al (2022) Civic engagement and psychological distress during the COVID-19 pandemic. BMC Public Health 22:869. https://doi.org/10.1186/s12889-022-13289-4
MacDonald JJ, Baxter-King R, Vavreck L et al (2022) Depressive symptoms and anxiety during the COVID-19 pandemic: large, longitudinal, cross-sectional survey. JMIR Ment Health 9:e33585. https://doi.org/10.2196/33585
Reading Turchioe M, Grossman LV, Myers AC et al (2021) Correlates of mental health symptoms among US adults during COVID-19, March–April 2020. Public Health Rep 136:97–106. https://doi.org/10.1177/0033354920970179
Bushman G, Mehdipanah R (2022) Housing and health inequities during COVID-19: findings from the national household pulse survey. J Epidemiol Community Health 76:121–127. https://doi.org/10.1136/jech-2021-216764
Shen X, MacDonald M, Logan SW et al (2022) Leisure engagement during COVID-19 and its association with mental health and wellbeing in US Adults. IJERPH 19:1081. https://doi.org/10.3390/ijerph19031081
Twenge JM, Joiner TE (2020) Mental distress among U.S. adults during the COVID-19 pandemic. J Clin Psychol 76:2170–2182. https://doi.org/10.1002/jclp.23064
Samuels J, Holingue C, Nestadt PS et al (2021) An investigation of COVID-19 related worry in a United States population sample. J Psychiatr Res 144:360–368. https://doi.org/10.1016/j.jpsychires.2021.10.036
Zhou Y, MacGeorge EL, Myrick JG (2020) Mental health and its predictors during the early months of the COVID-19 pandemic experience in the United States. IJERPH 17:6315. https://doi.org/10.3390/ijerph17176315
Vahratian A, Blumberg SJ, Terlizzi EP, Schiller JS (2021) Symptoms of anxiety or depressive disorder and use of mental health care among adults during the COVID-19 pandemic—United States, August 2020–February 2021. MMWR Morb Mortal Wkly Rep 70:490–494. https://doi.org/10.15585/mmwr.mm7013e2
Leung CMC, Ho MK, Bharwani AA et al (2022) Mental disorders following COVID-19 and other epidemics: a systematic review and meta-analysis. Transl Psychiatry 12:1–12. https://doi.org/10.1038/s41398-022-01946-6
Yuan K, Zheng Y-B, Wang Y-J et al (2022) A systematic review and meta-analysis on prevalence of and risk factors associated with depression, anxiety and insomnia in infectious diseases, including COVID-19: a call to action. Mol Psychiatry 27:3214–3222. https://doi.org/10.1038/s41380-022-01638-z
Ettman CK, Fan AY, Subramanian M et al (2023) Prevalence of depressive symptoms in U.S. adults during the COVID-19 pandemic: a systematic review. SSM Population Health 21:101348. https://doi.org/10.1016/j.ssmph.2023.101348
Wang Y, Kala MP, Jafar TH (2020) Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: a systematic review and meta-analysis. PLoS ONE 15:e0244630. https://doi.org/10.1371/journal.pone.0244630
Kourouklis D, Verropoulou G, Tsimbos C (2020) The impact of wealth and income on the depression of older adults across European welfare regimes. Ageing Soc 40:2448–2479. https://doi.org/10.1017/S0144686X19000679
Ettman CK, Fan AY, Philips AP et al (2023) Financial strain and depression in the U.S.: a scoping review. Transl Psychiatry. https://doi.org/10.1038/s41398-023-02460-z
Long H, Dam AV, Fowers A, Shapiro L The covid-19 recession is the most unequal in modern U.S. history. In: Washington Post. https://www.washingtonpost.com/graphics/2020/business/coronavirus-recession-equality/. Accessed 23 Aug 2023
Tsai J, Huang M (2019) Systematic review of psychosocial factors associated with evictions. Health Soc Care Community 27:e1–e9. https://doi.org/10.1111/hsc.12619
Matthews T, Danese A, Caspi A et al (2019) Lonely young adults in modern Britain: findings from an epidemiological cohort study. Psychol Med 49:268–277. https://doi.org/10.1017/S0033291718000788
Hsu T-L, Barrett AE (2020) The association between marital status and psychological well-being: variation across negative and positive dimensions. J Fam Issues 41:2179–2202. https://doi.org/10.1177/0192513X20910184
Soulsby LK, Bennett KM (2015) Marriage and psychological wellbeing: the role of social support. Psychology 6:1349–1359. https://doi.org/10.4236/psych.2015.611132
Birditt KS, Sherman CW, Polenick CA et al (2020) So close and yet so irritating: negative relations and implications for well-being by age and closeness. J Gerontol B Psychol Sci Soc Sci 75:327–337. https://doi.org/10.1093/geronb/gby038
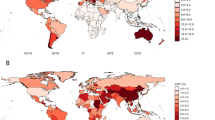
Santomauro DF, Herrera AMM, Shadid J et al (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 398:1700–1712. https://doi.org/10.1016/S0140-6736(21)02143-7
Zajacova A, Lawrence EM (2018) The relationship between education and health: reducing disparities through a contextual approach. Annu Rev Public Health 39:273–289. https://doi.org/10.1146/annurev-publhealth-031816-044628
Karg RS, Bose J, Batts KR, et al (2012) Past Year Mental Disorders among Adults in the United States: Results from the 2008–2012 Mental Health Surveillance Study. In: CBHSQ Data Review. Substance Abuse and Mental Health Services Administration (US), Rockville (MD)
Ettman CK, Goicoechea EB, Stuart EA (2023) Evolution of depression and anxiety over the COVID-19 pandemic and across demographic groups in a large sample of U.S. adults. AJPM Focus. https://doi.org/10.1016/j.focus.2023.100140
Bjelland I, Krokstad S, Mykletun A et al (2008) Does a higher educational level protect against anxiety and depression? The HUNT study. Soc Sci Med 66:1334–1345. https://doi.org/10.1016/j.socscimed.2007.12.019
Miech RA, Shanahan MJ (2000) Socioeconomic status and depression over the life course. J Health Soc Behav 41:162–176. https://doi.org/10.2307/2676303
Osypuk TL, Joshi P, Geronimo K, Acevedo-Garcia D (2014) Do social and economic policies influence health? A review. Curr Epidemiol Rep 1:149–164. https://doi.org/10.1007/s40471-014-0013-5
Evans L, Lund C, Massazza A et al (2022) The impact of employment programs on common mental disorders: a systematic review. Int J Soc Psychiatry 68:1315–1323. https://doi.org/10.1177/00207640221104684
Leifheit KM, Pollack CE, Raifman J et al (2021) Variation in state-level eviction moratorium protections and mental health among US adults during the COVID-19 pandemic. JAMA Netw Open 4:e2139585. https://doi.org/10.1001/jamanetworkopen.2021.39585
Acknowledgements
The authors would like to thank Priya Dohlman for editorial assistance.
Author information
Authors and Affiliations
Contributions
CKE conceptualized the project. MS, AYF, and CKE analyzed the data. GPA provided guidance on methodology. CKE, MS, and AYF drafted the manuscript. SMA provided editing of the manuscript. EAS and SG supervised the project. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ettman, C.K., Subramanian, M., Fan, A.Y. et al. Assets and depression in U.S. adults during the COVID-19 pandemic: a systematic review. Soc Psychiatry Psychiatr Epidemiol 59, 571–583 (2024). https://doi.org/10.1007/s00127-023-02565-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-023-02565-2