Abstract
Aims/hypothesis
Information on the associations of long-term exposure to fine particulate matter (with an aerodynamic diameter less than 2.5 μm; PM2.5) with the development of type 2 diabetes is scarce, especially for south-east Asia, where most countries are experiencing serious air pollution. This study aimed to investigate the long-term effects of exposure to ambient PM2.5 on the incidence of type 2 diabetes in a population of Taiwanese adults.
Methods
A total of 147,908 participants without diabetes, at least 18 years of age, were recruited in a standard medical examination programme between 2001 and 2014. They were encouraged to take medical examinations periodically and underwent at least two measurements of fasting plasma glucose (FPG). Incident type 2 diabetes was identified as FPG ≥7 mmol/l or self-reported physician-diagnosed diabetes in the subsequent medical visits. The PM2.5 concentration at each participant’s address was estimated using a satellite-based spatiotemporal model with a resolution of 1 × 1 km2. The 2 year average of PM2.5 concentrations (i.e. the year of and the year before the medical examination) was treated as an indicator of long-term exposure to ambient PM2.5 air pollution. We performed Cox regression models with time-dependent covariates to analyse the long-term effects of exposure to PM2.5 on the incidence of type 2 diabetes. A wide range of covariates were introduced in the models to control for potential effects, including age, sex, education, season, year, smoking status, alcohol drinking, physical activity, vegetable intake, fruit intake, occupational exposure, BMI, hypertension and dyslipidaemia (all were treated as time-dependent covariates except for sex).
Results
Compared with the participants exposed to the first quartile of ambient PM2.5, participants exposed to the second, third and fourth quartiles of ambient PM2.5 had HRs of 1.28 (95% CI 1.18, 1.39), 1.27 (95% CI 1.17, 1.38) and 1.16 (95% CI 1.07, 1.26), respectively, for the incidence of type 2 diabetes. Participants who drank occasionally or regularly (more than once per week) or who had a lower BMI (<23 kg/m2) were more sensitive to the long-term effects of exposure to ambient PM2.5.
Conclusions/interpretation
Long-term exposure to ambient PM2.5 appears to be associated with a higher risk of developing type 2 diabetes in this Asian population experiencing high levels of air pollution.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
The escalating pandemic of type 2 diabetes presents an enormous public health challenge around the world. There were estimated to be 383 million diabetic individuals and around 1.4 million deaths due to diabetes worldwide in 2016 [1, 2]. These numbers are expected to continue to rise rapidly, especially in middle- and low-income countries [3]. Type 2 diabetes can lead to a series of chronic complications, including vision loss, renal diseases, stroke and cardiovascular diseases, that pose an overwhelming burden on healthcare systems [4,5,6]. Several traditional cardiovascular risk factors are also risk factors for the development of type 2 diabetes, including obesity, high blood pressure and unhealthy lifestyles and behaviours, which have all been well investigated [7].
Air pollution is the largest single environmental risk in the world and it has recently been regarded as a novel risk factor for cardiovascular diseases. The American Heart Association states that exposure to particulate matter (PM) with an aerodynamic diameter less than 2.5 μm (PM2.5) is causally associated with an increased risk of cardiovascular morbidity and mortality [8]. Given the close linkage between type 2 diabetes and cardiovascular disease, PM2.5 air pollution may also act as a risk factor for type 2 diabetes. Although a few studies have investigated long-term exposure to PM and the development, prevalence and mortality rate of diabetes [9,10,11,12], the results are inconsistent. Large-scale prospective cohort studies are necessary to provide stable results and precise estimates. Furthermore, most studies have been conducted in North America and Europe [13,14,15,16] and limited information is available from other regions, such as the WHO western Pacific and south-east Asia regions, where many countries are experiencing high levels of air pollution. At the same time, epidemics of type 2 diabetes are growing quickly in Asia. We therefore investigated the association of long-term exposure to PM2.5 with the development of type 2 diabetes in a large longitudinal cohort of 147,908 adults in Taiwan.
Methods
Study participants
This study was based on an ongoing large prospective cohort whose details were described previously [17,18,19,20]. In brief, this cohort study recruited more than 0.6 million participants between 1994 and 2014. A private firm, the MJ Health Management Institution, provided a standard medical screening programme. The participants were of Chinese descent residing in Taiwan. They were encouraged to visit the firm periodically through a paid membership and underwent a series of medical examinations at each visit, including anthropometric measurements, spirometry test, blood and urinary tests and imaging tests, and answered a standard self-administered questionnaire survey. This cohort is an open (dynamic) cohort with no end date. Each year there are around 20,000 new members recruited to the cohort, in addition to the revisits by existing members. Data generated from the medical examinations have been computerised since 1996. As of December 2014, the database contained around 0.59 million Taiwan participants and had counted 1.35 million medical visits. Around 43.5% of the participants had attended at least two medical visits (range 2–28 visits). Each participant was required to sign an informed consent form before participation. We obtained ethical approval for this study from the Joint Chinese University of Hong Kong, New Territories East Cluster Clinical Research Ethics Committee.
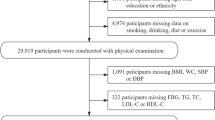
The participant selection in this study is presented in ESM Fig. 1. In total, 418,811 participants at least 18 years of age with fasting plasma glucose (FPG) measurements were recruited during 2001–2014, when data on PM2.5 concentration were available. We excluded 52,365 participants with incomplete information (2861 with PM2.5 data due to a missing address and 49,504 based on the covariates). We further excluded 15,008 participants with self-reported physician-diagnosed cancer or cardiovascular diseases at their first medical visit because of the possible effects of comorbidities on type 2 diabetes. Among the remaining 351,438 participants, 194,975 were excluded because they visited the institution and received medical examination only once. For those who had at least two medical examination visits, 5488 participants were excluded because they had diabetes (defined as FPG ≥7 mmol/l, or self-reported physician-diagnosed diabetes) at their first visit [21]. Because the development of type 2 diabetes is a chronic process, we further excluded 3067 participants with a follow-up duration of less than 2 years. Finally, 147,908 participants with 548,429 FPG measurements were included in the present analysis. Compared with those participants excluded because of attending only one medical visit, the 147,908 participants included in the present study had similar baseline distributions of general characteristics (ESM Table 1). The follow-up duration of the 147,908 participants ranged from 2 to 13.9 years (mean 6.7 years). The number of medical visits ranged from 2 to 23 with a median of 3.0. The mean visit interval was 1.2 years (SD 4.1).
Exposure assessment
We have described the detailed method for estimating PM2.5 exposure in previous publications [17, 19, 22, 23]. In brief, the ambient PM2.5 exposure at each participant’s address was estimated by a satellite-based spatial-temporal model with high resolution (1 × 1 km2) using the aerosol optical depth (AOD) data derived from the Moderate Resolution Imaging Spectroradiometer carried on US National Aeronautics and Space Administration satellites. The sample size for AOD data was around 300, which was similar to the general average level worldwide [24]. To address the issues of missing data and temporal limitation, we derived a correction factor using ground observations [23]. To calibrate the satellite-derived AOD data, we collected the ground observation of AOD from the aerosol robotic network (AERONET) in Taipei (EPA-NCU station, 24.97°N and 121.19°E), the capital city of Taiwan. Finally, we validated the model by comparing the estimated PM2.5 exposure with the monitoring data from more than 70 ground-level air pollution monitoring stations. The correlation coefficients for yearly average concentration ranged from 0.72 to 0.83 [17, 18].
The address of each participant (either residential or business) was noted during each medical visit so that the medical report could be mailed to them. Thus, any change of address was recorded. If a participant reported a change of his/her address in a follow-up medical visit, the PM2.5 concentration at the new address since the follow-up time point was applied in the data analysis. There were 29,032 (19.6%) participants who changed their address during this study. We geocoded each participant’s address into latitude and longitude data, which were used to calculate the address-specific yearly average PM2.5 concentration. The 2 year average concentration was then calculated based on the concentrations from the year of and the year before the medical examination as an indicator of long-term exposure to ambient PM2.5 air pollution.
Outcome measurement
Detailed information on the medical examination and quality control has been described in previous publications and in the Technical Reports published by the MJ Health Research Foundation [17, 18, 25]. An overnight fasting blood sample was taken in the morning and the plasma glucose level was measured enzymatically with a Hitachi 7150 analyser (Tokyo, Japan) if before 2005 or Toshiba C8000 analyser (Tokyo, Japan) if since 2005.
The health outcome in this study was incident type 2 diabetes. After the baseline assessment at the first visit, all the 147,908 non-diabetic participants were followed up, and incident type 2 diabetes was identified by medical assessment (defined as FPG ≥7 mmol/l, or self-reported physician-diagnosed diabetes) in subsequent visits [21]. The endpoint was the first occurrence of type 2 diabetes or the last visit if type 2 diabetes did not occur.
Contextual variables
We collected information on the participants’ demographic and socioeconomic characteristics, lifestyle and medical history by using a standard self-administered questionnaire at each visit. Height and weight were measured with participants wearing light indoor clothing without shoes. Seated blood pressure was measured using an auto-sphygmomanometer (CH-5000; Citizen, Tokyo, Japan). An overnight fasting blood sample was taken in the morning and a lipid profile was documented.
Based on previous literature [7, 26], we included the following factors as covariates in this study: age (years), sex (male or female), education (lower than high school [<10 years], high school [10–12 years], college or university [13–16 years] or postgraduate [>16 years]), smoking status (never, former or current), alcohol drinking (seldom [less than once per week], occasional [1–3 times/week] or regular [>3 times/week]), physical activity (defined as the product of metabolic equivalent value [MET; 1 MET = 1 kJ h−1 [kg bodyweight]−1] and duration of exercise [h] [27]: inactive [<3.75 MET-h], low [3.75–7.49 MET-h], medium [7.50–16.49 MET-h], high [16.50–25.49 MET-h] or very high [≥25.50 MET-h]), vegetable intake (seldom [<1 serving/day], moderate [1–2 servings/day] or frequent [>2 servings/day]), fruit intake (seldom [<1 serving/day], moderate [1–2 servings/day] or frequent [>2 servings/day]), occupational exposure to dust or organic solvents in the workplace (yes or no; as obtained by asking, ‘Are there any occupational hazards in your workplace?’), BMI (calculated as weight [kg] divided by the square of height [m]), hypertension (defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥90 mmHg or self-reported hypertension), dyslipidaemia (defined as total cholesterol ≥13.3 mmol/l, triacylglycerol ≥11.1 mmol/l or HDL-cholesterol <2.2 mmol/l), season of each visit (spring [March–May], summer [June–August], autumn [September–November], winter [December to February]) and calendar year at baseline.
Data analysis
We used Cox regression models with time-dependent covariates to analyse the associations between long-term exposure to ambient PM2.5 and the development of type 2 diabetes. The timescale used in the models was time-in-study (i.e. follow-up time). A crude model and three multivariable models were developed to compare the effects of covariates: Model 1 had no adjustment; Model 2 adjusted for demographic factors (age, sex and education), season and calendar year; Model 3 further adjusted for lifestyle factors (smoking status, alcohol drinking, physical activity, vegetable intake and fruit intake) and occupational exposure and Model 4 further adjusted for cardiovascular risk factors (BMI, hypertension and dyslipidaemia). All covariates were treated as time-dependent covariates except for sex. We estimated the HR with 95% CI as the risk of incident diabetes for PM2.5 quartiles (first to fourth quartile [μg/m3], respectively): <21.7, 21.7–<24.1, 24.1–<28.0, ≥28.0). We tested the linearity using likelihood ratio test and results showed that the associations deviated from linearity (χ2 = 35.2, p< 0.05). Therefore, we applied deciles to show the concentration–response associations between ambient PM2.5 and incident type 2 diabetes (first to tenth deciles [μg/m3], respectively: 5.7–<19.8, 19.8–<21.2, 21.2–<22.2, 22.2–<23.2, 23.2–<24.1, 24.1–<25.2, 25.2–<26.5, 26.5–<32.7, 32.7–<39.9 and 39.9–50.3).
We performed stratified analyses based on the following characteristics of the participants at baseline: sex (male vs female); education (<13 years vs ≥13 years); smoking status (never vs ever); alcohol drinking (seldom vs occasional/regular); physical activity (<7.5 MET-h vs ≥7.5 MET-h); BMI (<23 kg/m2 vs ≥23 kg/m2) [28]; hypertension (no vs yes) and dyslipidaemia (no vs yes). We stratified the participants into two subgroups according to the baseline cut off values of the aforementioned characteristics. We then performed data analyses separately within each subgroup using the Cox regression models with time-dependent covariates to derive the stratum-specific HR.
To test the stability of the associations, we further conducted sensitivity analyses by: (1) including participants with a follow-up of less than 2 years; (2) including only participants enrolled before 2005 whose FPG and lipids were measured with the Hitachi 7150; (3) including only the participants enrolled since 2005 whose FPG and lipids were measured with the Toshiba C8000; (4) excluding the participants with a business address to eliminate the potential misclassification of PM2.5 exposure due to different types of addresses; (5) using annual average PM2.5 concentration as an indicator for long-term exposure to PM2.5; (6) excluding those participants who were younger than 30 years old to better distinguish between type 1 and type 2 diabetes; (7) further adjusting for region of participant’s location (including five municipalities [Taipei, Taoyuan, Taichung, Tainan and Kaoshiung], ten counties [Hsinchu, Miaoli, Changhua, Nantou, Yunlin, Chiayi, Pingtung, Ilan, Hualien and Taitung] and one county-level city [Keelong]) to consider the effects of different regions; and (8) only including those participants with annual medical visit (interval of the medical visits ranged from 8 months to 16 months) to avoid delayed diagnosis of the disease.
All the statistical analyses were performed using R 3.3.2. (R Core Team, Vienna, Austria). The exposure and interaction effects were regarded as statistically significant at a two-tailed test level of 0.05 and 0.1, respectively.
Results
Table 1 shows the characteristics of all participants and participants with incident diabetes. The mean age of the participants was 38.3 years (SD 11.5 years) at baseline. The majority were well-educated, non-smokers and seldom drank alcohol; 4781 participants developed diabetes. At baseline, the participants who developed diabetes were generally older, had a lower level of education and were more likely to smoke and drink alcohol. They also had a higher prevalence of cardiovascular risk. The cumulative incidence was 3.2% with an incidence rate of 3.5 per 1000 person-years.
The locations of the participants are shown in Fig. 1. The participants mainly lived in the western part of Taiwan. In general, the south-western areas were the most heavily polluted and the middle and eastern areas were the least heavily polluted. The spatial pattern of exposure contrast throughout the island generally remained stable during the study period. The PM2.5 concentrations increased slightly from 2001 to 2004 (the mean 2 year PM2.5 was 24.8, 26.2, 28.7 and 29.6 μg/m3, respectively, for participants enrolled in 2001, 2002, 2003 and 2004) and then declined gradually from 2005 to 2014 (the mean 2 year PM2.5 was 27.4, 26.9, 26.9, 26.7, 26.8, 25.8, 25.6, 25.0, 23.7 and 24.4 μg/m3, respectively, for 2005, 2006, 2007, 2008, 2009, 2010, 2011, 2012, 2013 and 2014). The overall mean was 26.5 μg/m3 (SD 7.4 μg/m3) with an interquartile range of 21.7–28.0 μg/m3.
Table 2 shows the associations between ambient PM2.5 and the development of type 2 diabetes. Exposure to PM2.5 was significantly associated with a higher risk of incident type 2 diabetes. Compared with the participants exposed to the first quartile of ambient PM2.5, those exposed to the second, third and fourth quartiles of PM2.5 were associated with HRs (95% CI) of 1.28 (1.18, 1.39), 1.27 (1.17, 1.38) and 1.16 (1.07, 1.26), respectively, for incident type 2 diabetes after adjusting for a wide range of covariates. The concentration–response association is presented in Fig. 2. No obvious effect threshold was observed.
The concentration–response association between ambient PM2.5 and incident type 2 diabetes in the Taiwanese participants. The data are presented as estimated HR (95% CI) associated with PM2.5 concentration deciles. The association was adjusted for age, sex, education, season, year, smoking status, alcohol drinking, physical activity, vegetable intake, fruit intake, occupational exposure, BMI, hypertension and dyslipidaemia. The PM2.5 range (μg/m3) of the first to tenth deciles, respectively, was: 5.7–<19.8, 19.8–<21.2, 21.2–<22.2, 22.2–<23.2, 23.2–<24.1, 24.1–<25.2, 25.2–<26.5, 26.5–<32.7, 32.7–<39.9 and 39.9–50.3
The results of stratified analyses are presented in Table 3. Significant modified effects were observed for the categories of BMI and alcohol drinking. Long-term PM2.5 exposure had a stronger association with the development of diabetes in participants with BMI <23 kg/m2 or a habit of occasional or regular alcohol consumption. No significant modifying effects were observed for the other factors. Sensitivity analyses generally yielded similar results (ESM Table 2).
The associations between covariates and incident type 2 diabetes are presented in ESM Table 3.
Discussion
The results of this large prospective cohort study show that long-term exposure to ambient PM2.5 appears to be associated with a higher risk of developing type 2 diabetes after controlling for a wide range of covariates. The associations remain robust in the stratified and sensitivity analyses.
Our results are in line with those of some previous studies [16, 29,30,31]. Three studies, in Canada, Denmark and the USA, found that a 10 μg/m3 increase in PM2.5 was associated with a higher risk of incident diabetes with the HR ranging from 1.11 to 1.52 [16, 29, 30]. In a Hong Kong elderly population, a significant association with an HR of 1.15 per interquartile range (3.2 μg/m3) was also observed by Qiu et al [31]. The larger HR in the Hong Kong study was possibly due to its elderly participants who were potentially more vulnerable. There are limited cohort studies in Asia but a few large-scale cross-sectional studies showed that PM2.5 was significantly associated with higher risk of prevalence of diabetes [12, 32], supporting our findings. Several previous studies also found that traffic-related air pollution or other air pollutants, including NO2 and O3, were associated with incident diabetes [14, 33,34,35]. However, five previous studies did not find that PM significantly affected the development of diabetes [26, 35,36,37,38]. Many factors may contribute to this inconsistency, including the heterogeneity of the study populations, study regions, chemical components of PM, research methods and diagnostic criteria. Our study targeted a population in Taiwan, in which the PM2.5 levels were higher than those in North America and Europe. One advantage of this study is that the exposure contrast among our participants was relatively large. The accuracy of the exposure estimate may also play an important role in the inconsistency among the studies. Some previous studies estimated PM exposure based on the proximity of residences to fixed monitoring stations, with the same exposure level assigned to an entire community (district, county or city). Such community-level exposure assessment (ecological fallacy) may mask the true spatial variation or introduce misclassification of exposure, thus leading to the inconsistent results. Finally, the effect sizes of PM2.5 on incident type 2 diabetes are small. Thus, a large sample size is necessary to provide sufficient statistical power, yet many previous studies had relatively small sample sizes.
In this study, we categorised PM2.5 into quartiles. It seems the HR values decreased slightly in participants with higher quartile exposure (HR 1.28, 1.27 and 1.16 for the second, third and fourth quartile, respectively). We do not know the exact reasons for this phenomenon, but we speculate that the use of category variable might lead to a loss of information and an increase in uncertainty. Because the likelihood ratio test show that the association marginally deviated from linearity (χ2 = 35.2, p < 0.001), we used PM2.5 deciles to draw the concentration–response association (Fig. 2). The HR values decreased in the sixth to ninth deciles and jumped in the tenth decile. It is difficult to interpret this phenomenon but the non-linearity association might also be due to the heterogeneities of the populations in different cities/areas and other unidentified confounders (e.g. some factors might affect the health of people living in the same city but this may vary across the city). The high HR in the tenth decile of PM2.5 concentration could be partially explained by the larger PM2.5 concentration range (39.9–50.3 μg/m3) and the relatively smaller number of incident diabetes cases (there were 416 cases in the tenth decile, while the number in each of the first nine deciles ranged from 450 to 521). Nonetheless, further studies to illustrate the concentration–response relationship between PM2.5 and type 2 diabetes are warranted.
The biological mechanism underlying the association between long-term exposure to PM2.5 and the development of type 2 diabetes is not completely understood. Animal experiments have shown that PM2.5 can produce hypothalamic inflammation and induce metabolic disorders, including autonomic imbalance, visceral adipose inflammation, endothelial dysfunction, insulin resistance and overt diabetes [39, 40]. One in vivo study noted that long-term exposure to PM2.5 can further cause metabolic disorders by triggering the unfolded protein response and macrophage infiltration [41]. In addition, cardiovascular disease and diabetes may have similar mechanistic pathways (systematic inflammation and oxidative stress) [42]. Our previous study clearly showed that PM2.5 may induce systemic inflammation [17, 43]. Thus, the systematic inflammation and oxidative stress induced by PM2.5 may be the main mediators between PM2.5 exposure and diabetes by disrupting insulin signalling [44, 45].
We also explored the potential modifying effects of a range of factors. Although no significant modifying effects were observed for sex, education, smoking status, physical activity, hypertension and dyslipidaemia, statistical significance was observed for the modifying effect of alcohol drinking. Presently, however, there is little information on the modifying effects of alcohol drinking. BMI was another significant modifier in this study. Interestingly, the participants with a lower BMI had a higher risk of developing diabetes due to PM2.5 exposure, even though BMI is a significant risk factor for diabetes development. This phenomenon has also been observed in previous studies but the modifying effects were generally insignificant [29, 32, 33, 46]. Further studies are warranted to assess the different modifying effects.
This study has several important strengths. First, it targeted a large general population in Asia, where type 2 diabetes epidemics are growing quickly and people are generally experiencing serious air pollution. Second, it used a longitudinal study design, and most incidences of type 2 diabetes were identified by FPG measurements. In comparison with self-reported diabetes, the FPG test is a relatively time-efficient way to minimise diagnostic misclassification and lessen the likelihood of underestimating the incidence of type 2 diabetes [34]. The longitudinal study design also enabled us to account for the effects related to the change of PM2.5 exposure and a wide range of covariates. The associations did not change materially after including these covariates in the models. Third, the large sample size and the relatively long follow-up duration gave the study sufficient power to detect the small effects of ambient PM2.5 on the development of type 2 diabetes. The large sample size also allowed us to generate stable results and precise estimates. Finally, we used a novel model based on satellite-derived AOD data with high resolution (1 × km2) to estimate individual exposure at the participants’ addresses. This technology permitted us to overcome the spatial coverage limitation that typically occurs when using data obtained only from monitoring stations. The exposure data at individual level also enabled us to avoid ecological fallacies.
This study also has several limitations. First, we did not have information on indoor and gaseous pollutants. However, we included smoking as a covariate as it is an important source of household air pollution in developed economies. The generally high correlations between gaseous pollutants and PM2.5 suggest that we should analyse their effects separately [16]. Second, the PM2.5 exposure levels were calculated at the fixed addresses of the participants, and their daily activity patterns were not considered. More advanced technologies are needed for more accurate assessment of exposure in future studies. Third, we did not account for noise exposures due to the information being unavailable. Noise may be regarded as a potential risk of cardiovascular disease [47]. Fourth, it is difficult to distinguish between type 1 and type 2 diabetes in a large-scale epidemiological study with around 0.15 million participants. However, the targeted population were non-diabetic participants aged 18 years or above and therefore the majority of individuals who developed diabetes were likely to develop type 2 diabetes. The sensitivity analysis that excluded participants with a baseline age of <30 years yielded similar results (ESM Table 2), which further supported the association between PM2.5 and the development of type 2 diabetes. Fifth, the follow-up frequency and interval of medical examinations varied among the participants. Thus, it is difficult to identify the exact onset date of the disease for those participants with a long interval between medical examinations. However, the sensitivity analysis that only included the participants with annual medical examination yielded similar results. Finally, the participants were relatively healthy and were educated to a high level. Therefore, we should be cautious when generalising the results to other populations.
In conclusion, we found long-term exposure to ambient PM2.5 to be significantly associated with a higher risk of developing type 2 diabetes in a population from Asia, in which people in many of the region’s countries are generally experiencing high levels of air pollution and the prevalence of diabetes is rising rapidly. We advocate urgent strategies to reduce global air pollution that can aid in preventing the current pandemic of type 2 diabetes.
Data availability
The datasets generated and/or analysed during the current study are available upon request.
Abbreviations
- AOD:
-
Aerosol optical depth
- FPG:
-
Fasting plasma glucose
- MET:
-
Metabolic equivalent value
- PM:
-
Particulate matter
- PM2.5 :
-
Particulate matter with an aerodynamic diameter less than 2.5 μm
References
Hay S (2017) Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:49
Steel N (2017) Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 390:1151–1210
World Health Organization (2016) Global report on diabetes. World Health Organization, Geneva
Donnelly R, Emslie-Smith AM, Gardner ID, Morris AD (2000) ABC of arterial and venous disease: vascular complications of diabetes. BMJ 320(7241):1062–1066. https://doi.org/10.1136/bmj.320.7241.1062
Sjølie AK, Stephenson J, Aldington S et al (1997) Retinopathy and vision loss in insulin-dependent diabetes in Europe: the EURODIAB IDDM Complications Study. Ophthalmology 104(2):252–260. https://doi.org/10.1016/S0161-6420(97)30327-3
Perneger TV, Brancati FL, Whelton PK, Klag MJ (1994) End-stage renal disease attributable to diabetes mellitus. Ann Intern Med 121(12):912–918. https://doi.org/10.7326/0003-4819-121-12-199412150-00002
Zimmet P, Alberti K, Shaw J (2001) Global and societal implications of the diabetes epidemic. Nature 414(6865):782–787. https://doi.org/10.1038/414782a
Brook RD, Rajagopalan S, Pope CA et al (2010) Particulate matter air pollution and cardiovascular disease. Circulation 121(21):2331–2378. https://doi.org/10.1161/CIR.0b013e3181dbece1
Wang B, Xu D, Jing Z, Liu D, Yan S, Wang Y (2014) Effect of long-term exposure to air pollution on type 2 diabetes mellitus risk: a systemic review and meta-analysis of cohort studies. Eur J Endocrinol 171(5):R173–R182. https://doi.org/10.1530/EJE-14-0365
Park SK, Wang W (2014) Ambient air pollution and type 2 diabetes: a systematic review of epidemiologic research. Curr Environ Health Rep 1(3):275–286. https://doi.org/10.1007/s40572-014-0017-9
Balti EV, Echouffo-Tcheugui JB, Yako YY, Kengne AP (2014) Air pollution and risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Diabetes Res Clin Pract 106(2):161–172. https://doi.org/10.1016/j.diabres.2014.08.010
Yang B-Y, Qian ZM, Li S et al (2018) Ambient air pollution in relation to diabetes and glucose-homoeostasis markers in China: a cross-sectional study with findings from the 33 communities Chinese health study. Lancet Planet Health 2(2):e64–e73. https://doi.org/10.1016/S2542-5196(18)30001-9
Honda T, Puna VC, Manjourides J, Suh H (2017) Associations between long-term exposure to air pollution, glycosylated hemoglobin and diabetes. Int J Hyg Environ Health 220(7):1124–1132. https://doi.org/10.1016/j.ijheh.2017.06.004
Jerrett M, Brook R, White LF et al (2017) Ambient ozone and incident diabetes: a prospective analysis in a large cohort of African American women. Environ Int 102:42–47. https://doi.org/10.1016/j.envint.2016.12.011
Eze IC, Foraster M, Schaffner E et al (2017) Long-term exposure to transportation noise and air pollution in relation to incident diabetes in the SAPALDIA study. Int J Epidemiol 46(4):1115–1125. https://doi.org/10.1093/ije/dyx020
Hansen AB, Ravnskjaer L, Loft S et al (2016) Long-term exposure to fine particulate matter and incidence of diabetes in the Danish nurse cohort. Environ Int 91:243–250. https://doi.org/10.1016/j.envint.2016.02.036
Zhang Z, Chang L-Y, Lau AK et al (2017) Satellite-based estimates of long-term exposure to fine particulate matter are associated with C-reactive protein in 30 034 Taiwanese adults. Int J Epidemiol 46(4):1126–1136. https://doi.org/10.1093/ije/dyx069
Lao XQ, Zhang Z, Lau AKH et al (2018) Exposure to ambient fine particulate matter and semen quality in Taiwan. Occup Environ Med 75(2):148–154. https://doi.org/10.1136/oemed-2017-104529
Zhang Z, Guo C, Lau AK et al (2018) Long-term exposure to fine particulate matter, blood pressure, and incident hypertension in Taiwanese adults. Environ Health Perspect 126(1):017008. https://doi.org/10.1289/EHP2466
Wu X, Tsai SP, Tsao CK et al (2017) Cohort profile: the Taiwan MJ cohort: half a million Chinese with repeated health surveillance data. Int J Epidemiol 46(6):1744–1744g. https://doi.org/10.1093/ije/dyw282
American Diabetes Association (2014) Diagnosis and classification of diabetes mellitus. Diabetes Care 37(Supplement_1):S81–S90. https://doi.org/10.2337/dc14-S081
Lin C, Li Y, Yuan Z, Lau AK, Li C, Fung JC (2015) Using satellite remote sensing data to estimate the high-resolution distribution of ground-level PM2.5. Remote Sens Environ 156:117–128. https://doi.org/10.1016/j.rse.2014.09.015
Lin C, Li Y, Lau AKH et al (2016) Estimation of long-term population exposure to PM2.5 for dense urban areas using 1-km MODIS data. Remote Sens Environ 179:13–22. https://doi.org/10.1016/j.rse.2016.03.023
Liu Y (2014) Monitoring PM2.5 from space for health: past, present, and future directions. EM (Pittsburgh Pa) 6:6–10
Wang ML (2016) MJ Health Research Foundation, MJ Health Resource Center, Technical Report. Available from www.mjhrf.org/file/en/report/MJHRF-TR-01MJ%20Health%20Database.pdf. Accessed 20 Jan 2018
Puett RC, Hart JE, Schwartz J, Hu FB, Liese AD, Laden F (2011) Are particulate matter exposures associated with risk of type 2 diabetes? Environ Health Perspect 119(3):384–389. https://doi.org/10.1289/ehp.1002344
Lao XQ, Deng HB, Liu X et al (2018) Increased leisure-time physical activity associated with lower onset of diabetes in 44,828 adults with impaired fasting glucose. Brit J Sport Med [Article online]. Available from http://bjsm.bmj.com/content/early/2018/01/12/bjsports-2017-098199. Accessed 28 April 2018
Pan W-H, Flegal KM, Chang H-Y, Yeh W-T, Yeh C-J, Lee W-C (2004) Body mass index and obesity-related metabolic disorders in Taiwanese and US whites and blacks: implications for definitions of overweight and obesity for Asians. Am J Clin Nutr 79(1):31–39. https://doi.org/10.1093/ajcn/79.1.31
Chen H, Burnett RT, Kwong JC et al (2013) Risk of incident diabetes in relation to long-term exposure to fine particulate matter in Ontario, Canada. Environ Health Perspect 121(7):804–810. https://doi.org/10.1289/ehp.1205958
Coogan PF, White LF, Yu J et al (2016) PM2.5 and diabetes and hypertension incidence in the Black Womenʼs Health Study. Epidemiol 27:202–210
Qiu H, Schooling CM, Sun S et al (2018) Long-term exposure to fine particulate matter air pollution and type 2 diabetes mellitus in elderly: a cohort study in Hong Kong. Environ Int 113:350–356. https://doi.org/10.1016/j.envint.2018.01.008
Liu C, Yang C, Zhao Y et al (2016) Associations between long-term exposure to ambient particulate air pollution and type 2 diabetes prevalence, blood glucose and glycosylated hemoglobin levels in China. Environ Int 92:416–421
Andersen ZJ, Raaschou-Nelsen O, Ketzel M et al (2012) Diabetes incidence and long-term exposure to air pollution: a cohort study. Diabetes Care 35(1):92–98. https://doi.org/10.2337/dc11-1155
Krämer U, Herder C, Sugiri D et al (2010) Traffic-related air pollution and incident type 2 diabetes: results from SALIA cohort study. Environ Health Perspect 118(9):1273–1279. https://doi.org/10.1289/ehp.0901689
Coogan PF, White LF, Jerrett M et al (2012) Air pollution and incidence of hypertension and diabetes mellitus in black women living in Los Angeles. Circulation 125(6):767–772. https://doi.org/10.1161/CIRCULATIONAHA.111.052753
Park SK, Adar SD, O’Neill MS et al (2015) Long-term exposure to air pollution and type 2 diabetes mellitus in a multiethnic cohort. Am J Epidemiol 181(5):327–336. https://doi.org/10.1093/aje/kwu280
OʼDonovan G, Chudasama Y, Grocock S et al (2017) The association between air pollution and type 2 diabetes in a large cross-sectional study in Leicester: the CHAMPIONS study. Environ Int 104:41–47. https://doi.org/10.1016/j.envint.2017.03.027
Weinmayr G, Hennig F, Fuks K et al (2015) Long-term exposure to fine particulate matter and incidence of type 2 diabetes mellitus in a cohort study: effects of total and traffic-specific air pollution. Environ Health 14:1–8
Rajagopalan S, Brook RD (2012) Air pollution and type 2 diabetes: mechanistic insights. Diabetes 61(12):3037–3045. https://doi.org/10.2337/db12-0190
Ying Z, Xu X, Bai Y et al (2014) Long-term exposure to concentrated ambient PM2.5 increases mouse blood pressure through abnormal activation of the sympathetic nervous system: a role for hypothalamic inflammation. Environ Health Perspect 122(1):79–86. https://doi.org/10.1289/ehp.1307151
Mendez R, Zheng Z, Fan Z, Rajagopalan S, Sun Q, Zhang K (2013) Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am J Transl Res 5:224–234
Pereira Filho M, Pereira L, Arbex FF et al (2008) Effect of air pollution on diabetes and cardiovascular diseases in São Paulo, Brazil. Braz J Med Biol Res 41(6):526–532. https://doi.org/10.1590/S0100-879X2008005000020
Zhang Z, Hoek G, Chang L-Y et al (2017) Particulate matter air pollution, physical activity and systemic inflammation in Taiwanese adults. Int J Hyg Environ Health 221:41–47
Sun Q, Yue P, Deiuliis JA et al (2009) Ambient air pollution exaggerates adipose inflammation and insulin resistance in a mouse model of diet-induced obesity. Circulation 119(4):538–546. https://doi.org/10.1161/CIRCULATIONAHA.108.799015
Houstis NE, Rosen ED, Lander ES (2006) Reactive oxygen species play a causal role in multiple forms of insulin resistance. Nature 440(7086):944–948. https://doi.org/10.1038/nature04634
Coogan PF, White LF, Yu J et al (2016) Long term exposure to NO2 and diabetes incidence in the Black Womenʼs Health Study. Environ Res 148:360–366. https://doi.org/10.1016/j.envres.2016.04.021
Münzel T, Gori T, Babisch W, Basner M (2014) Cardiovascular effects of environmental noise exposure. Eur Heart J 35(13):829–836. https://doi.org/10.1093/eurheartj/ehu030
Acknowledgements
We appreciate the MJ Health Research Foundation for authorising the use of its health data (authorisation code: MJHR2015002A). We are grateful to the anonymous reviewers and the editors for their valuable comments.
Funding
This work was in part supported by the Environmental Health Research Fund of the Chinese University of Hong Kong (7104946). CG and YB are supported by the PhD Studentship of the Chinese University of Hong Kong.
Author information
Authors and Affiliations
Contributions
XQL conceived and designed the study and obtained the funding. L-YC, AKHL and XQL supervised this study. L-YC, AKHL and XQL acquired the data. CG, YB and ZZ searched the literature. ZZ, YB, YCC and WKJ cleaned the data. CL and AKHL estimated the PM2.5 concentration. CG analysed the data. CG, XQL, TT, C-YL and TCC interpreted the results. CG and XQL drafted the manuscript. XQL, CG, TT, C-YL and TCC revised the manuscript. All authors contributed to the content and critical revision of the manuscript and agreed to submit the manuscript for publication. XQL is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
The authors declare that there is no duality of interest associated with this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM
(PDF 156 kb)
Rights and permissions
About this article
Cite this article
Lao, X.Q., Guo, C., Chang, Ly. et al. Long-term exposure to ambient fine particulate matter (PM2.5) and incident type 2 diabetes: a longitudinal cohort study. Diabetologia 62, 759–769 (2019). https://doi.org/10.1007/s00125-019-4825-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-019-4825-1