Abstract
Background
Massive hemoptysis (MH) is a rare but potentially life-threatening condition of patients with mainly advanced cystic fibrosis (CF). Morphological lung changes are aggravated with disease progression. The aim of this study was to determine whether morphological lung changes differ between patients with CF (pwCF) who have MH and pwCF without MH.
Methods
Chest computed tomography (CT) scans of pwCF and MH acquired at a maximum of 4 months prior to MH (1/2008 to 2/2015) were evaluated for morphological changes and bronchial artery (BA) diameters. Lung lobes with MH were compared with lobes without MH and with matched control patients with end-stage CF and no hemoptysis using the Helbich scoring system.
Results
The study included 26 patients with MH (PMH; 15 female, median age 29 years, interquartile range [IQR]: 25–33.75) and 17 matched control patients (11 male, median age 24 years, IQR: 19.5–30). No difference in Helbich score was detected between lobes with MH and matched control patients (p = 0.051). Higher scores were detected in lobes with MH compared to lobes without MH in PMH (p = 0.021), but no difference was detected in the subscores. The BA diameters were larger in PMH (p = 0.02); 85% of PMH had unilateral MH, with 65% of MH involving only one or two lobes.
Conclusion
Morphological changes are more severe in lobes with MH in the same patient, but there is no difference when compared with matched control patients. Besides abscess/sacculation, no specific changes for MH were identified. Other factors such as BA hypertrophy might play a pivotal role in the pathogenesis of MH in pwCF. Commonly used scores to evaluate chest CT in pwCF cannot be used to assess MH, and other factors, e.g., hypertrophied BA, not represented and not measured in these scores, might be more suitable for assessing the risk for MH.
Zusammenfassung
Hintergrund
Massive Hämoptysen (MH) sind selten, aber bei Patienten mit vorwiegend fortgeschrittener zystischer Fibrose (CF) potenziell lebensbedrohend. Die morphologischen Lungenveränderungen verschlimmern sich mit dem Krankheitsfortschritt. Ziel der vorliegenden Studie war es zu untersuchen, ob die morphologischen Lungenveränderungen sich zwischen Patienten mit CF (pwCF), bei denen MH bestehen, und pwCF ohne MH unterscheiden.
Methoden
Thorax-Computertomographie(CT)-Aufnahmen von pwCF mit MH, die maximal 4 Monate vor den MH (1/2008 bis 2/2015) angefertigt worden waren, wurden in Bezug auf morphologische Veränderung und Durchmesser der Bronchialarterien (BA) ausgewertet. Die Lungenlappen mit MH wurden verglichen mit Lungenlappen ohne MH und mit gematchten Kontrollpatienten mit CF im Endstadium, aber ohne Hämoptysen gemäß dem Helbich-Scoringsystem.
Ergebnisse
In die Studie wurden 26 Patienten mit MH (PMH; 15 weiblich, Durchschnittsalter 29 Jahre, Interquartilsabstand [IQR]: 25–33,75) und 17 gematchte Kontrollpatienten eingeschlossen (11 männlich, Durchschnittsalter 24 Jahre, IQR: 19,5–30). Es wurde kein Unterschied im Helbich-Score zwischen Lungenlappen mit MH und gematchten Kontrollpatienten festgestellt (p = 0,051). Höhere Scores fanden sich bei Lungenlappen mit MH im Vergleich zu Lungenlappen ohne MH bei PMH (p = 0,021), aber in den Subscores war kein Unterschied festzustellen. Die BA-Durchmesser waren bei PMH größer (p = 0,02); 85% der PMH wiesen unilateral eine MH auf, dabei betrafen 65% der MH nur einen oder 2 Lappen.
Schlussfolgerung
Innerhalb desselben Patienten mit MH sind die morphologischen Veränderungen in den Lungenlappen mit MH schwerer ausgeprägt, aber es besteht kein Unterschied, wenn man sie mit gematchten Kontrollpatienten vergleicht. Außer Abszess/Sakkulation wurden keine spezifischen Veränderungen für MH festgestellt. Andere Faktoren, wie eine BA-Hypertrophie, könnten eine entscheidende Rolle in der Pathogenese von MH bei pwCF spielen. Häufig verwendete Scores zur Auswertung einer Thorax-CT bei pwCF können nicht zur Beurteilung von MH eingesetzt werden, und andere Faktoren, z. B. hypertrophierte BA, die nicht in diesen Scores repräsentiert und gemessen werden, könnten zur Einschätzung des Risikos von MH besser geeignet sein.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with cystic fibrosis (pwCF) experience massive hemoptysis (MH) as a rare but potentially life-threatening complication with mortality rates as high as 75% [1, 2]. Overall, 1–4.1% of pwCF will experience MH with an annual incidence of approximately 1% [3]. Commonly, older patients with advanced disease are affected, but also patients with only minor impairment of lung function and even children can experience MH [3,4,5]. Many pwCF report blood-stained sputum and/or recurrent minor hemoptysis, which is in most cases self-limiting and does not require therapy [6, 7]. However, when MH occurs, it may create a medical emergency demanding immediate therapy to save the patient [3, 8]. Medical emergencies are often carried out in suboptimal conditions, perhaps at night and with reduced staff, patients must be transferred to a specialized center for bronchial artery embolization (BAE), and, equally important, the patient is likely to be in a severely compromised and unstable condition, which negatively influences outcome.
Cystic fibrosis is a chronic disease causing local and systemic inflammation that results in a variety of structural lung tissue changes over time. Upregulation of serum vascular endothelial growth factor is triggered by this inflammatory process promoting hypertrophy of bronchial arteries (BAs), which become enlarged, tortuous, and dilated vessels [9]. The BAs are localized submucosally in the bronchial wall. Flume et al. hypothesize that chronic and acute inflammation weakens the vessel walls and can lead to episodic or persistent bleeding into the bronchial lumen, with subsequent hemoptysis [3, 10]. According to this hypothesis, it would be expected that massive hemoptysis would occur in patients with more severe disease, yet the complication has been known to occur in patients with seemingly milder disease [3, 5, 11, 12].
Surveillance of lung tissue changes is possible with chest x‑ray, computed tomography scans (CT), commonly non-contrast-enhanced, and increasingly with magnetic resonance imaging (MRI), as MRI protocols and imaging quality are improving [13, 14]. Medical imaging is evaluated for morphological lung tissue changes and an overall point score of the lung is created to compare examinations over time and objectify disease progression. For the evaluation of chest CT scans in pwCF, different morphology scoring systems are applied, e.g., the Helbich score [15,16,17,18]. However, the existing scoring systems do not consider the anatomical distribution of morphological changes, nor do they take into account the side or separate lobes affected by MH. Although bronchiectasis has been described as a main risk factor for MH [19,20,21], data on risk factors for MH in CF are scarce [22,23,24] and data evaluating morphological changes of chest CT in pwCF and MH do not exist.
The aim of this study was to identify differences in morphological changes in lobes affected by MH and lobes not affected by MH in the same patient in comparison with patients who have end-stage CF but without MH, using the Helbich scoring system for chest CT assessment [16].
Material and methods
Patients with MH
Patients or public were not involved in the design, conduct, reporting, or dissemination plans of our research. This study is a secondary subsample analysis (n = 26) of a previously published multicenter study carried out between January 2008 and February 2021 measuring BA diameters in pwCF [24]. In the present study, morphological changes in pwCF and MH were evaluated, which was not part of the parent study.
All adult pwCF referred to our hospital for MH between January 2008 and February 2015 who underwent at least one super-selective BA coil embolization (ssBACE) were included in this retrospective multicenter study. Patients arrived at our institution with external chest CT scans from ten different hospitals across Germany. The CT scans therefore differed in terms of protocols and scanning devices. The gender and age of the patients, forced expiratory volume in 1 s in % predicted (ppFEV1), coagulation parameters, pulmonary exacerbation at the time of MH, and intervention data were documented. For all patients, the attending hospitals were contacted again in 2022 for follow-up.
If patients underwent more than one ssBACE procedure, the CT scans refer to the first intervention. Localization of the culprit lobe(s) was based on the patient’s perception and on digital subtraction angiography findings, and considered correct if hemostasis was obtained for at least 48 h [10, 25, 26]. Here, MH was defined as > 240 ml in 24 h or recurrent bleeding of substantial volume (> 100 ml/day) for several days or weeks [22, 26]. We followed a restrictive intervention protocol embolizing suspected culprit vessels only and treating a maximum of three lobes per intervention.
Control group
In total, 35 chest CT scans (dual-source CT scanner SOMATOM Force, Siemens, Erlangen, Germany) of patients with end-stage CF and no history of hemoptysis (Pcontrol_1) were evaluated retrospectively for morphological changes and BA diameter. We generated a subgroup of less affected and thus severity-matched control group patients (Pcontrol_2) for better comparison with PMH. The CT scans had been carried out between September 2007 and July 2021 to evaluate suitability for lung transplantation in all control patients. The gender, age of the patients, and ppFEV1 were documented.
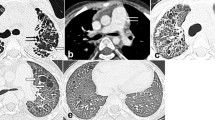
CT evaluation for morphological changes
All 26 CT scans of PMH were contrast enhanced. All CT scans in control groups 1 and 2 were carried out as CT angiography. Chest CT scans of PMH and Pcontrol_1 and Pcontrol_2 were assessed semi-quantitatively by consensus by two radiologists with 11 and 25 years of experience in chest CT (MD, HK) according to the Helbich scoring system [16]. Readers were not involved in BAE. Good intra- and interobserver agreement using this scoring system has been published previously [15, 27, 28]. Readers were blinded to patient data, the presence of hemorrhage, and the site of hemorrhage/ssBACE.
The Helbich scoring system was modified to segments per lobe instead of lobes per lung for parameters scored by the number of subunits involved (Table 1). The CT scans were evaluated for a total of 11 subscores (Table 2). A maximum of 30 points could be reached per lobe. Scores were calculated (a) as median for the right and left lung and (b) as median for lobes affected by MH and lobes not affected by MH. The lingula was counted as a separate lobe. Air trapping was not evaluated, as images in expiration had not been acquired. The BA diameters were measured in all contrast-enhanced CT scans in the mediastinum close to their origin in perpendicular orientation to the vessel.
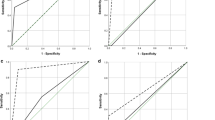
Statistical analysis
Data were highly skewed and are therefore presented as median/interquartile range. The Mann–Whitney U test for two independent groups was used to compare the Helbich scores of lung lobes with MH against lobes without MH in the same patient and against Pcontrol_1 and Pcontrol_2, and to calculate differences in BA diameters in PMH, Pcontrol_1 and Pcontrol_2. The Kruskal–Wallis test was used to compare the Helbich subscores in PMH, Pcontrol_1 and Pcontrol_2. Bonferroni correction of data was performed to adapt the significance levels. Statistical analysis was carried out using IBM SPSS Statistics Version 27. Values of p < 0.05 were considered statistically significant.
Ethics approval and consent to participate
This retrospective multicenter study has been approved by the ethics committee of the Aerztekammer Nordrhein according to § 15 registry number 2016/181 and by the ethics committee of the Medical School Hannover, registry number 10245_BO_K_2022, who also waived the need for informed consent from all patients. All methods were carried out in accordance with relevant guidelines and regulations.
Results
Patients with massive hemoptysis
A total of 34 consecutive pwCF who had undergone ssBACE for MH in our institution between January 2008 and February 2015 met the inclusion criteria of this study. Four patients had to be excluded as no CT scan prior to ssBACE had been carried out due to the urgency of the situation. Four patients had to be excluded because the time of the CT scan exceeded the 4‑month interval prior to intervention. Overall, 26 patients (15 female, median age 29 years, IQR: 25–33.75) had received CT scans 0 days to 4 months (IQR 9 days, 1.25–25.5) prior to embolization and were included for CT morphology evaluation and BA measurements. In seven patients, CT scans were carried out 0–1 day prior to MH. The intervention characteristics of PMH are listed in Table 3. The median ppFEV1 was 46.5% (37–63.7%). Coagulation parameters were normal in all patients. Eight patients (31%) died during the observation period 2008–2022. In the patient charts exacerbation of pulmonary infection was noted as “severe pulmonary infection” at time of hemoptysis in three cases and as “no current infection” in four cases. In the remaining 19 patients no information concerning pulmonary exacerbation at the time of MH was available, which led to the exclusion of pulmonary exacerbation for statistical analysis. In 17 patients (65%) MH occurred during the cold season in Germany from October to April. In two of three cases with pulmonary exacerbation, MH occurred during the cold season. In three of five cases without pulmonary exacerbation, MH occurred outside the cold season.
Control groups
In total, 35 Pcontrol_1 (21 male, median age 24.0 years, IQR, 18.5–33.5, ppFEV1 30% [25–43.5]) were included as control group patients Pcontrol_1. A total of 17 patients (11 male, median age 24 years (19.5–30), ppFEV1 45% [32–55]) were included in the severity-matched subgroup Pcontrol_2.
Morphological CT scan evaluation
Helbich score
The median modified Helbich score in PMH including all lobes was lower with 76.5 points (67.25–88.5), than in control group 1 patients (Pcontrol_1) with 98 points (79–110), and comparable to the severity-matched control group 2 (Pcontrol_2) with 76 points (69–92). There was no difference in median Helbich score of the right lung at 39 points (34.25–45.25) compared to the left lung with 39 points (33–46.5) in PMH (p = 1.0), and neither in Pcontrol_1 with 50 points (IQR, 41–56) for the right lung and 48 points (IQR, 38.5–53) for left lung (p = 1.0) nor in Pcontrol_2 with 40 points (35–45) for the right lung compared to 37 points (35–43) for the left lung (p = 1.0). In patients with unilateral MH (n = 22), the median Helbich point score for lungs with MH was 39 points (IQR, 33.25–42.75) and 39 points (IQR 33–44.75) of lungs not affected by MH (p = 0.75). The median lobar score of PMH was 13 (11–16). In PMH, the median lobar score of all lobes with MH was 14 (12–16), and the median lobar score of all lobes without MH was 13 (11–15; p = 0.021). The median lobar score of Pcontrol_1 was 16 (13–18) and thus higher than in lobes with MH (p = 0.004). The median lobar score in Pcontrol_2 was 13 (11–15) and there was no difference compared to lobes with MH (p = 0.051) and compared to PMH (p = 0.87). The median subscores “severity of bronchiectasis” (p = 0.34) and “bronchial wall thickening” (p = 0.122) were both higher in lobes with MH than in lobes without MH but this did not reach statistical significance. The severity of bronchiectasis was significantly lower in lobes with MH compared to Pcontrol_1 (p = 0.001; Table 4) and Pcontrol_2 (p = 0.003; Table 5). The subscore “ground glass infiltrate” was significantly lower in PMH than in Pcontrol_1 (p = 0.01) but not in Pcontrol_2 (p = 1.0) and there was no difference in lobes with MH compared to Pcontrol_1 (p = 0.14) and to Pcontrol_2 (p = 1.0). In the seven CT scans carried out directly at the time of MH, this subscore showed a distribution independent of lobes with MH in all but one patient. The subscore “emphysema” was higher in Pcontrol_1 than in lobes with MH (p = 0.09) and PMH (p = 0.07), but no difference was detected in lobes with MH compared to lobes without MH (p = 1.0) and to Pcontrol_2 (p = 1.0). The subscore “sacculation/abscess” was significantly higher in lobes with MH than in Pcontrol_2 (p = 0.05) but there was no difference when compared to Pcontrol_1 (p = 0.18), and no difference was found between lobes with MH and lobes without MH in PMH (p = 0.23; Table 4). The subscore “generations of bronchial divisions involved in bronchiectasis/mucus plugging” was higher in Pcontrol_1 than in lobes with MH (p = 0.07) but there was no difference between lobes with and without MH (p = 1.0) and there was also no difference between lobes with MH and Pcontrol_2 (p = 0.51). All other Helbich subscores did not show significant differences, neither between lobes with MH and without MH in PMH nor compared to Pcontrol_1 or Pcontrol_2. The median Helbich subscores of lobes with and without MH in PMH, Pcontrol_1, and Pcontrol_2 are listed in Tables 4 and 5. The median Helbich lobar subscores are shown in Table 2 for PMH, in Table 6 for Pcontrol_1, and in Table 7 for Pcontrol_2.
In PMH, “severity of bronchiectasis” was most marked in the right upper lobe and the left lower lobe in lobes with MH (Table 2). The maximum lobar score was reached for the right upper and left lower lobe in lobes with MH and in the left upper lobe in lobes without MH (Table 8). In Pcontrol_1 and Pcontrol_2, both upper lobes reached the highest median lobar point scores (Table 8).
Bronchial artery diameters
The BA diameter measurements in PMH showed a median of 3.9 mm (3.3–4.3) and were higher than BA diameters of Pcontrol_1 with a median of 3.2 mm (2.6–3.7) (p = 0.008) and higher than BA diameters in Pcontrol_2 with 3.0 mm (2.6–3.6) (p = 0.02).
Discussion
This retrospective multicenter study on chest CT findings in pwCF found no difference in the severity of morphological changes in lobes with MH in patients with MH when compared to control patients without MH. However, median lobar scores were higher in lobes with MH compared to lobes without MH in the same patient but without any difference when compared with severity-matched control patients. The subscore “sacculation/abscess” was higher in lobes with MH compared to severity-matched control patients but with overlapping interquartile ranges and without any difference when compared with lobes without MH. The subscores “severity of bronchiectasis,” “emphysema,” “ground glass opacity,” and “generations of bronchial divisions involved in bronchiectasis/mucus plugging” were significantly higher in Pcontrol_1 and Pcontrol_2 than in PMH and in lobes with MH. None of the subscores showed significant differences between lobes with MH and lobes without MH. The BA diameters were significantly higher in PMH than in both control groups.
Although there is common agreement on BAs being the culprit vessels in MH, there is debate about why and when and in whom BAs rupture or erode and cause MH [3, 12, 25]. The results of our study put into question the hypothesis of severe morphological changes inducing MH in pwCF. Prevailing theories for the development of hemoptysis suggest combined inflammatory and mechanical stress weakens the walls of hypertrophied and friable submucosal BAs, which then erode and bleed into the airways [3, 10]. This hypothesis seemed corroborated by the fact that MH occurred mainly in advanced disease with major morphological lung changes [1, 3, 8, 29]. Thompson et al. described older age and more severe pulmonary impairment as risk factors for MH [29].
In our cohort we found morphological changes predominantly in the upper lobes and in the right lung, a common finding in CF [18], with equal distribution in PMH and in both control groups. Furthermore, MH also predominantly occurred in the right lung, in the upper lobes, and with older age in our cohort, as was also described in the literature [3, 4, 23]. On the other hand, hemoptysis and MH also occur in young patients and children as well as in patients with well-preserved lung function independent of the severity of lung disease [5, 12].
In our study, no difference was detected in total lung score of PMH compared to Pcontrol_1 nor compared to the severity-matched control group Pcontrol_2using a common scoring system. Moreover, when evaluated separately for lungs with and lungs without hemoptysis in patients with unilateral MH, no difference in point score was found. When evaluated on a lobar level, the median lobar score in lobes with MH was not higher than in the severity-matched Pcontrol_2. However, median lobar scores in lobes with MH were significantly higher than in lobes without MH, indicating that morphological changes contribute at least in part to MH, but no specific subscores were identified. The subscore “severity of bronchiectasis” was significantly less severe in PMH and in lobes with MH than in both control groups that did not suffer from MH. This is especially interesting as bronchiectasis has been described as a main risk factor for MH in a variety of lung conditions [19,20,21].
Contrary to common practice, which includes treating all enlarged BAs, we followed a protocol of prudent embolization, exclusively treating lobes affected by MH. This enabled us to identify lobes with MH and lobes without MH for scoring. However, this information is not available from routine chest CT. But as most patients are able to localize the bleeding site [10, 25, 26], this important clinical information might be integrated in assessing the risk for MH together with chest CT findings. For the clinician to use chest CT evaluation for MH risk estimate, it would be necessary to carry out chest CT interpretation on a lobar level and to identify lobes with the highest score or rapid progression in the same patient. However, the hypothesis of morphological changes correlating with or even causing MH might be reconsidered, since morphological changes were not more severe in lobes with MH compared to Pcontrol_2 with comparable global Helbich scores as PMH.
Exacerbation of pulmonary infection has been described to be associated with MH [10, 23, 30]. Efrati et al. described exacerbation of a pulmonary infection as the most common precipitating factor for a hemoptysis event in 90% of study patients [5]. It was found that MH occurred more often during winter months when infections are more common [23]. In our cohort, data concerning pulmonary exacerbation from patient charts were too scarce for statistical evaluation, but MH occurred during the cold season in 65% of patients. Interestingly, the subscore “ground glass infiltrate” was significantly more marked in Pcontrol_1 than in PMH, but no difference was noted between lobes with and lobes without MH, also when compared to Pcontrol_2. Repetitive aspiration of coughed-up blood might lead to the redistribution of intraluminal blood to various lobes possibly explaining why the subscore “ground glass infiltrate,” often seen as a correlate of hemoptysis, did not show higher scores in lobes with MH than in lobes without MH. This higher subscore in Pcontrol_1 but not in Pcontrol_2 might be explained by more advanced disease in Pcontrol_1. Also in line with this finding, the subscore “consolidation,” a correlate for pulmonary infection, did not show any difference between PMH and control patients nor between lobes affected by MH and lobes not affected by MH. We believe more severe findings in control patients reflect more severe disease. Of note, the subscore “abscess/sacculation” was higher in lobes with MH compared to Pcontrol_2, but not higher than in lobes without MH. However, this subscore should be considered as a possible risk factor for MH, especially when found in an area targeted by the patient for hemoptysis. Interestingly, 65% of patients undergoing ssBACE required intervention in only one or two lobes. In 85% of patients, MH was unilateral and 50% of these patients underwent a single-lobe intervention.
These findings indicate that MH is, at least in the majority of patients, a localized process not reflected in common scoring systems. Although morphological CT changes and MH occur in the same region and in pwCF with older age, CT morphology assessed with the Helbich score, or other common scores [15,16,17,18], does not seem to reflect bleeding risk, as the global morphology score and several subscores were highest in Pcontrol_1. Severe morphological changes and changes leading to MH might both progress over time, possibly both triggered by chronic inflammation, but they might not be linked and might not induce each other, instead constituting parallel processes. Data on possible factors causing MH are scarce and the pathogenesis of MH is yet unknown [3]. Presumably, the presence of other factors such as significant BA hypertrophy, which is not automatically found in patients with advanced disease, or the presence of Staphylococcus aureus, might play a role in the pathogenesis of MH [24, 29]. We demonstrated that BA diameters were significantly larger in PMH than in Pcontrol_1 and Pcontrol_2, which suggests that BA hypertrophy plays a key role in MH in pwCF. Interestingly, BA diameters were significantly smaller in Pcontrol_1, who suffered more severe morphological changes than PMH. Since severe morphological changes and only minor hypertrophy of BAs are present in patients without MH, severe morphological changes might not be an important risk factor for MH. On the contrary, the presence of less severe morphological changes and significantly larger BA in PMH might indicate BA hypertrophy to be a more pivotal contributing factor to MH. These results are corroborated by the fact that female patients have significantly smaller BA diameters [24] and 58% of PMH were females compared to only 35% of females in matched Pcontrol_2.
Routine chest CT in pwCF is carried out without contrast agents, thus rendering assessment and measurement of BA impossible, and BA diameters are not part of any scoring system for CF [19,20,21].
Limitations
The retrospective observational character of the study is a clear limitation as it is highly prone to bias. We tried to minimize these effects by blinding readers to patient characteristics and by mixing the CT scans of PMH and Pcontrol for reading. Both readers were not involved in BAE and could therefore not identify images or patients. In addition, MH in pwCF is a rare complication and the number of patients enrolled in this study would be very difficult to obtain in a prospective study design. Another limitation is the difference in global Helbich score and in ppFEV1 between PMH and Pcontrol‑1, with both parameters more severe in Pcontrol_1, indicating more severe disease. We aimed to minimize this effect by choosing a severity matched sub-control group Pcontrol_2 that was comparable in global Helbich score and ppFEV1. The results from this subgroup confirmed the findings. However, both control groups were slightly younger than the PMH group possibly creating a bias in BA diameters as BA diameters increase with age [24]. Older patients with more advanced lung disease more commonly develop MH [3, 4]. Higher morphology scores would therefore have been expected in lobes with MH in the older PMH when compared to the younger Pcontrol_1 and Pcontrol_2, which was not the case. On the other hand, the control groups comprised more male patients, with males having significantly larger BAs, which was not the case either [24].
Then, MH might have influenced the subscores “ground glass infiltrate” and “mucus plugging” as intraluminal blood might have been misinterpreted, but only seven of 23 CT scans were carried out on the day before or on the day of the MH itself and both subscores were within normal range. However, this uncertainty remains.
Another, albeit minor, limitation was the fact that due to the multicenter study design, CT protocols of PMH differed according to the transferring hospital. Mostly, PMH arrived with external medical imaging at our center. However, the diagnostic value of all CT scans met high-quality standards. Chest CT of control patients was carried out as CT angiography. We did not consider this difference to influence the assessment of structural changes of lung parenchyma enough to create significant bias.
Practical conclusion
-
The results of our study put into question the prevailing hypothesis of severe morphological changes in patients with cystic fibrosis (pwCF) preceding major hemoptysis (MH).
-
The severity of morphological changes was not higher in patients with MH (PMH) nor in lobes with MH than in matched control patients without MH. However, lobes affected by MH had higher Helbich scores compared to lobes without MH, which is why chest computed tomography (CT) assessment on a lobar level might be a better tool when assessing for impending MH.
-
Several subscores were significantly higher in control patients but no difference was found between lobes with MH and lobes without MH. However, the subscore “abscess/sacculation” might need special attention as it was higher in lobes with MH than in a severity-matched control group.
-
Bronchial artery (BA) diameters were significantly higher in PMH compared to the more severely affected control group and the severity-matched control group, indicating that BA plays a pivotal role in MH.
-
The results of this study indicate that although morphological changes and MH both occur with older age and in the same lung region, they might not be linked but may be parallel processes due to chronic inflammation.
-
Our data provide an argument that commonly used scores to evaluate morphological CT changes in pwCF are not able to assess MH, and other factors, e.g., hypertrophied BA, not represented and not measured in these scores, might be more suitable for assessing the risk for MH.
-
Scoring would need to be adapted to a lobar level to provide important clinical information when estimating the risk for MH, as MH seems to be a rather localized process.
-
Further prospective studies combining, e.g., lobar CT evaluation, the patient’s perception of frail lung regions, and the actual occurrence of MH might help to identify important risk factors for MH and possibly predict MH in pwCF.
Availability of data and materials
The data that support the findings of this study are available from the authors of this article but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of the different institutions where patients are affiliated. Contact corresponding author MD for data request.
Abbreviations
- BA:
-
bronchial artery
- BAE:
-
bronchial artery embolization
- CF:
-
cystic fibrosis
- CT:
-
computed tomography
- MH:
-
massive hemoptysis
- PMH :
-
patients with massive hemoptysis
- Pcontrol‑1 :
-
control group 1 patients without hemoptysis
- Pcontrol‑2 :
-
severity-matched control group 2 patients without hemoptysis
- pwCF:
-
patients with cystic fibrosis
- ssBACE:
-
super-selective bronchial artery coil embolization
References
Marshall B (2022) Cystic fibrosis foundation patient registry 2021 annual data report. Bethesda
Crocco JA, Rooney JJ, Fankushen DS, DiBenedetto RJ, Lyons HA (1968) Massive hemoptysis. Arch Intern Med 121(6):495–498
Flume PA, Yankaskas JR, Ebeling M, Hulsey T, Clark LL (2005) Massive hemoptysis in cystic fibrosis. Chest 128(2):729–738
O’Dell CM, Gill AE, Hawkins CM (2017) Bronchial artery embolization for the treatment of acute hemoptysis. Tech Vasc Interv Radiol 20(4):263–265
Efrati O, Harash O, Rivlin J, Bibi H, Meir MZ, Blau H et al (2008) Hemoptysis in Israeli CF patients—prevalence, treatment, and clinical characteristics. J Cyst Fibros 7(4):301–306
di Sant’agnese PA, Davis PB (1979) Cystic fibrosis in adults. 75 cases and a review of 232 cases in the literature. Am J Med 66(1):121–132
Cystic Fibrosis Foundation https://www.cff.org/about-us/annual-report
FitzSimmons SC (1993) The changing epidemiology of cystic fibrosis. J Pediatr 122(1):1–9
McColley SA, Stellmach V, Boas SR, Jain M, Crawford SE (2000) Serum vascular endothelial growth factor is elevated in cystic fibrosis and decreases with treatment of acute pulmonary exacerbation. Am J Respir Crit Care Med 161(6):1877–1880
Brinson GM, Noone PG, Mauro MA, Knowles MR, Yankaskas JR, Sandhu JS et al (1998) Bronchial artery embolization for the treatment of hemoptysis in patients with cystic fibrosis. Am J Respir Crit Care Med 157(6):1951–1958
Garcia B, Flume PA (2019) Pulmonary complications of cystic fibrosis. Semin Respir Crit Care Med 40(6):804–809
Barben JU, Ditchfield M, Carlin JB, Robertson CF, Robinson PJ, Olinsky A (2003) Major haemoptysis in children with cystic fibrosis: a 20-year retrospective study. J Cyst Fibros 2(3):105–111
Sileo C, Corvol H, Boelle PY, Blondiaux E, Clement A, Ducou Le Pointe H (2014) HRCT and MRI of the lung in children with cystic fibrosis: comparison of different scoring systems. J Cyst Fibros 13(2):198–204
Leutz-Schmidt P, Eichinger M, Sommerburg O, Stahl M, Triphan SMF, Gehlen S et al (2020) Magnetresonanztomographie der Lunge bei Mukoviszidose. Radiologe 60(9):813–822
Bhalla M, Turcios N, Aponte V, Jenkins M, Leitman BS, McCauley DI et al (1991) Cystic fibrosis: scoring system with thin-section CT. Radiology 179(3):783–788
Helbich TH, Heinz-Peer G, Eichler I, Wunderbaldinger P, Götz M, Wojnarowski C et al (1999) Cystic fibrosis: CT assessment of lung involvement in children and adults. Radiology 213(2):537–544
de Jong PA, Tiddens HAWM (2007) Cystic fibrosis specific computed tomography scoring. Proc Am Thorac Soc 4(4):338–342
Brody AS, Klein JS, Molina PL, Quan J, Bean JA, Wilmott RW (2004) High-resolution computed tomography in young patients with cystic fibrosis: distribution of abnormalities and correlation with pulmonary function tests. J Pediatr 145(1):32–38
Abdulmalak C, Cottenet J, Beltramo G, Georges M, Camus P, Bonniaud P et al (2015) Haemoptysis in adults: a 5-year study using the French nationwide hospital administrative database. Eur Respir J 46(2):503–511
Stern RC, Wood RE, Boat TF, Matthews LW, Tucker AS, Doershuk CF (1978) Treatment and prognosis of massive hemoptysis in cystic fibrosis. Am Rev Respir Dis 117(5):825–828
Fellows KE, Khaw KT, Schuster S, Shwachman H (1979) Bronchial artery embolization in cystic fibrosis; technique and long-term results. J Pediatr 95(6):959–963
Flume PA, Mogayzel PJ, Robinson KA, Rosenblatt RL, Quittell L, Marshall BC et al (2010) Cystic fibrosis pulmonary guidelines: pulmonary complications: hemoptysis and pneumothorax. Am J Respir Crit Care Med 182(3):298–306
Dohna M, Renz DM, Stehling F, Dohna-Schwake C, Sutharsan S, Neurohr C et al (2021) Coil embolisation for massive haemoptysis in cystic fibrosis. BMJ Open Respir Res 8(1):e985
Dohna M, Kühl H, Sutharsan S, Dohna-Schwake C, Vo Chieu VD, Hellms S et al (2022) Bronchial artery diameter in massive hemoptysis in cystic fibrosis. BMC Pulm Med ;22(1):424
Monroe EJ, Pierce DB, Ingraham CR, Johnson GE, Shivaram GM, Valji K (2018) An interventionalist’s guide to hemoptysis in cystic fibrosis. Radiographics 38(2):624–641
Tonkin ILD, Hanissian AS, Boulden TF, Baum SL, Gavant ML, Gold RE et al (1991) Bronchial arteriography and embolotherapy for hemoptysis in patients with cystic fibrosis. Cardiovasc Intervent Radiol 14(4):241–246
Padley SP, Adler BD, Hansell DM, Müller NL (1993) Bronchiolitis obliterans: high resolution CT findings and correlation with pulmonary function tests. Clin Radiol 47(4):236–240
de Jong PA, Ottink MD, Robben SGF, Lequin MH, Hop WCJ, Hendriks JJE et al (2004) Pulmonary disease assessment in cystic fibrosis: comparison of CT scoring systems and value of bronchial and arterial dimension measurements. Radiology 231(2):434–439
Thompson V, Mayer-Hamblett N, Kloster M, Bilton D, Flume PA (2015) Risk of hemoptysis in cystic fibrosis clinical trials: A retrospective cohort study. J Cyst Fibros 14(5):632–638
Schidlow DV, Taussig LM, Knowles MR (1993) Cystic fibrosis foundation consensus conference report on pulmonary complications of cystic fibrosis. Pediatr Pulmonol 15(3):187–198
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
MD was responsible for conceptualization and study design, investigation, writing of the original draft, visualization, data curation and analysis and interpretation of patient data. HK was responsible for data analysis, critical review of the original draft and contributed resources. SS was responsible for conceptualization of the study and contributed resources. NB was responsible for study design, data analysis and interpretation, statistics as well as critical review of the original draft. VDVC, SH and NK contributed resources and critical review of the original draft. MM was responsible for conceptualization and supervision of the study, data analysis and interpretation, and review and editing of the original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
M. Dohna, H. Kühl, S. Sutharsan, N. Bruns, V.D. Vo Chieu, S. Hellms, N. Kornemann and M.J. Montag declare that they have no competing interests.
This multicenter study has been approved by the ethics committee of Aerztekammer Nordrhein according to § 15 registry number 2016/181 and by the ethics committee of Medical School Hannover, registry number 10245_BO_K_2022 who also waived the need for informed consent from all patients. All methods were carried out in accordance with relevant guidelines and regulations.
The supplement containing this article is not sponsored by industry.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.

Scan QR code & read article online
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dohna, M., Kühl, H., Sutharsan, S. et al. Morphological chest CT changes in cystic fibrosis and massive hemoptysis. Radiologie (2024). https://doi.org/10.1007/s00117-024-01266-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00117-024-01266-4