Abstract
Purpose
This study evaluates whether the fracture level alters the outcomes of minimally invasive hybrid stabilization (MIHS) with double-threaded, uncemented polyaxial screws for unstable osteoporotic vertebral fractures.
Methods
This prospective cohort study included 73 patients (71.23% females, mean age: 79.9 ± 8.8 years) with unstable OF 3–4 fractures treated by MIHS between Nov 2015-Jan 2018. Patient characteristics, operative data, clinical outcomes, complications, radiological outcomes, and midterm (24-month) follow-up regarding functionality, pain, and quality of life were analyzed.
Results
Patients had thoracolumbar (71.23%), thoracic (10.97%), and lumbar (17.8%) fractures. Operative time was < 120 min in 73.97% of patients, with blood loss < 500 ml in 97.25% of cases. No in-hospital mortality was recorded. Spine-associated complications occurred in 15.07% of patients, while 36.98% of patients had urinary tract infections (n = 12), pneumonia (n = 5), and electrolyte disturbances (n = 9). The mean length of hospital stay was 13.38 ± 7.20 days. Clinically-relevant screw loosening occurred in 1.7% of screws, and secondary adjacent fractures were diagnosed in 5.48% of patients. The alpha-angle improved significantly postoperatively (mean change: 5.4°) and remained stable for 24 months. The beta-angle improved significantly from 16.3° ± 7.5 to 10.8° ± 5.6 postoperatively but increased slightly to 14.1° ± 6.2 at midterm follow-up. Although no differences were seen regarding baseline data, clinical outcomes, and complications, fracture level significantly altered the COMI score at 24 months with no effect on pain score or quality-of-life.
Conclusion
MIHS using polyaxial screws is a safe treatment for single-level osteoporotic spinal fractures. Fracture level did not alter radiological reduction loss; however, it significantly altered patients’ function at 24 months.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Incidences of osteoporotic vertebral fractures (OVFs) rose markedly over the last two decades and OVFs are nowadays a leading cause of morbidity in the elderly [1, 2]. Suboptimal post-traumatic restoration of spinal alignment is a risk factor for additional spinal fractures [3]. Therefore, the target of surgical therapy is two-fold. First, it aims to achieve significant pain reduction. Second, it aims to improve spinal alignment.
Although therapeutic aims are clearly defined, treatment guidelines differ between institutions. The osteoporotic fractures (OF)-classification allows for the extraction of classification-adjusted treatment recommendations and is frequently utilized in Europe. Condensed, conservative therapy is indicated in patients with acute stable OVFs (OF types 0, 1, 2, and type OF 3 without relevant posterior cortex involvement) [4, 5]. In the case of persistent pain, impaired mobility, or increased kyphotic misalignment, minimal invasive cement-augmented therapy strategies are recommended. [6,7,8].
The current study focussed on unstable OVFs with posterior edge involvement (types OF 3 with pedicle involvement and OF 4). These fracture morphologies are prone to result in kyphotic deformities and subsequent spinal stenosis Intralesional stand-alone procedures such as kyphoplasty or vertebroplasty are believed to be insufficient to adequately restore spinal alignment and stability. Dorsal stabilization is frequently applied for these unstable OVFs. Short-segment posterior stabilization, without anterior support, is associated with hardware failure, loss of reduction, and the development of a postoperative kyphotic deformity. Long-segment posterior stabilization, on the other hand, seems to be too invasive for the geriatric population. More recently, successful minimal invasive hybrid stabilization (MIHS) techniques, including additional cement augmentation of the injured vertebra have been successfully introduced in patients with OVFs and without neurological deficits. [4, 5, 9]. Different modifications of MIHS for OVFs have been described in the literature. Both cement-augmented screws and cementless screws have been utilized, and the short-term clinical outcome is promising [10,11,12,13,14]. However, cemented screw augmentation can lead to complications, such as cement leakage [15], pulmonary embolism [16], and increased risk of infection [17].
To date, midterm (defined as 24-month) radiologic outcomes of MIHS and the impact on quality of life are currently unclear. In our hospital, double treated pedicle screws and titan rods are used to prevent multilevel cementation in the elderly. The current study was performed to determine midterm clinical and radiological outcomes of MIHS with double-threated uncemented pedicle screws for unstable osteoporotic vertebral fractures (OVFs).
Methods
Study design and ethical approval
A prospective cohort study was performed at the Department of Spine Surgery at the Rhein-Maas Clinic, an accredited spine center certified by the German Spine Community (DWG). Patients were enrolled in the study between November 1st, 2015, and January 1st, 2018. The protocol was approved by the regional Ethics Committee (file number: 2016448). Informed consent was obtained from all participants.
Cohort
All patients admitted to our institution for potential spinal injuries were examined clinically and received conventional radiographs. A routine magnetic resonance imaging (MRI) was performed in those patients without contraindications for MRI. Additionally, computer tomography (CT) was carried out in patients with moderate- and high-energy traumas and those individuals with contraindications for MRI. Spinal fracture stability was assessed using the Osteoporotic Fracture (OF) classification system [9]. The following inclusion criteria have been applied:
(1) age > 60 years, (2) a single-level unstable fracture, (3) a fracture at the level of the thoracic or lumbar spine, (4) fracture caused by low-energy trauma with osteoporosis, (5) a type OF 3 with pedicle involvement and 4 according to the OF classification [9].
Of note, according to our protocols, spine tissue sampling was performed and histological analysis was performed in all patients to rule out metastatic origin and to confirm local osteoporotic disease. Meanwhile, cases with metastatic as well as old fractures were excluded from the analysis.
Surgical technique
All patients were treated with MIHS. This procedure entails a kyphoplasty of the fractured vertebral body and fixation of the adjacent level above and below the fractured vertebral body with uncemented pedicel screws. In short, all interventions were performed under general anesthesia and in a prone position. A balloon-kyphoplasty is performed first. Subsequent minimal invasive pedicle-screw stabilization was done using dual-threated polyaxial screws without cement augmentation (Longitude II, Ballon Kyphon, Fa. Medtronic, Minneapolis, MN, USA). A detailed description of the protocol is attached as Appendix 1.
Postoperative management and follow-up
After surgery and mobilization, post-operative radiographs in a standing position were made in two planes. An additional CT scan was only made to control for correct screw placement or anatomic reduction in symptomatic patients.
Clinical and conventional radiological assessment was performed prior the intervention, after 3 months, and after 24 months of follow-up. Furthermore, anti-osteoporotic therapy was initiated directly after hospitalization.
Baseline parameters
The following parameters were collected:
Patient characteristics: gender, age, pre-operative ASA (American Society of Anesthesiologists)-score [18], and body mass index (BMI).
Injury characteristics: fracture classification and specific radiological fracture features, such as kyphosis angles, as described by Cobb, were independently determined by three investigators (MM, AA, and MT) using sagittal conventional X-ray imaging [19,20,21].
The Alpha Cobb-angle was determined by drawing lines parallel to the upper endplate of and the lower endplate of the fractured vertebral body. The angle between both lines reflected the Alpha Cobb-angle.
The Beta Cobb-angle was calculated by drawing lines parallel to the upper endplate of the vertebral body adjacent to the fractured and the lower endplate of the fractured vertebral body. The angle between these two lines was the Beta Cobb-angle.
Clinical outcome parameters
Both in-hospital and follow-up outcome data were collected and compared over time.
The following parameters were measured: operative time, estimated intra-operative blood loss, the need for blood transfusion therapy, the need for operative re-intervention/revision surgery [22], length of hospital stay (LOS), and complication rates (defined as Clavien-Dindo Grade 3 or higher) [23]. Examined complications included pneumonia, material outbreak, adjacent spine fractures, clinically relevant cement leakage, and screw loosening. Of note, the diagnostic criteria for screw loosening, in line with the literature, are partly subjective; however specific signs include:
-
A radiolucent area (> 1 mm) around the screw [14/4–9].
-
Presence of the 'double halo' sign [14/4,10].
Pain and functional outcomes were also determined at 24 months of follow-up. Additional stratification of these midterm outcomes was performed to determine the impact of fracture localization. Three subgroups were investigated: thoracic fractures (fracture above the vertebral body Th11), thoracolumbar fractures (the involvement of the vertebral body Th11-L2), and fractures of the lumbar spine (L3-5). The following parameters were determined and compared:
Visual Analog Scale (VAS): pain assessment was performed using an 11-point numeric rating scale, where zero indicates no pain, and 10 indicates the most intense pain possible [24].
The Core Outcome Measures Index (COMI)-back: a brief instrument for assessing the main outcome in patients with back problems (pain, function, symptom-related well-being, quality of life, and overall disability) [25]. The COMI-back was developed during the 'Spine Tango'-project and is a validated outcome assessment tool for patients with back problems. A higher COMI-back reflects an inferior outcome [26].
European Quality of Life-5 Dimensions (EQ-5D)-score: represents a validated questionnaire-based quality-of-life assessment tool. The EQ-5D consists of different domains determining a respondent’s current health status. Mobility, self-care, activities, pain/discomfort, and anxiety/depression were scored [27, 28].
Histopathological data
Osteoporotic changes in included patients were confirmed by the histopathological examination which showed cancellous trabeculae in between there is bone marrow with blood formation cells (blue dots) and fat cells (white holes). Figure 1 shows two tissue samples consistent with these changes. Although very compressed, fragmented, and pushed together with artifacts, bleeding and signs of tissue remodeling were evident by the partially fibrotic marrow in between the cancellous trabeculae.
Radiologic outcome parameters
The following radiological parameters were studied over time (pre-operatively, post-operatively, and after 24 months):
-
Changes in the Alpha Cobb-angle.
-
Changes the Beta Cobb-angle.
Statistical analysis
Statistical analysis was performed using SPSS 22.0 for Windows (Chicago, IL, USA). A descriptive summary of baseline demographic data was provided in the form of mean (standard deviation) for continuous data and numbers (percentages) for binary/categorical data. For skewed data, the median and interquartile range (IQR) were provided. The differences between groups were calculated using chi-square or Fisher’s exact test for the ordinal data. Either paired or unpaired T-tests or the Mann-Whitney U test were used to analyze continuous data, depending on the assumption of normal distribution. When comparing clinical and outcome data in different spinal fracture levels (thoracolumbar, thoracic, and lumber), the one-way analysis of variance (ANOVA) test was used for continuous outcomes. P-values < 0.05 were considered statistically significant.
Results
Patient and fracture characteristics
Patients’ characteristics are shown in Table 1. A total of 73 patients were included. As anticipated, female predominance was seen as 52 (71.23%) female and 20 (28.77%) male individuals were included. Patients had a mean age of 79.9 ± 8.8 years. Patients had an overall preoperative mean ASA-score of 3 ± 0.57 and a mean BMI of 28.0 ± 5.20 kg/m2. Most patients were diagnosed with thoracolumbar fractures (N = 52, 71.23%), while isolated lumber and thoracic spinal fractures were seen in 13 (17.81%) and 8 (10.96%) patients, respectively. Patients had a mean preoperative alpha-angle of 13.7°± 6.5 and a beta-angle of 16.3°± 7.5. Stratification of baseline data based on fracture level did not reveal any significant changes between groups in terms of age, gender, ASA score, BMI, OF class, and radiological data.
Operative data
Operative time varied between 60 and 120 min in 54 (73.97%) patients and was less than one hour in 14 (19.17%) cases. Prolonged interventions (> 120 min) were reported in five (6.84%) patients, of whom one (1.37%) intervention took more than three hours. A total of 292 pedicle screws were placed in 52 patients. Intra-operative blood loss was < 100 ml in 35 patients (47.94%), 100–500 ml in 36 (49.31%) patients, and > 500 ml in two (2.74%) patients.
Table 2 summarizes operative time and intraoperative blood loss stratified by the level of spinal fracture. No significant differences were noted in operative time (P = 0.095) and blood loss (P = 0.454) based on the level of spinal fracture.
Clinical outcomes and complications
In-hospital mortality did not occur and 39 (53.42%) patients had an uncomplicated clinical course. Eleven (15.07%) patients suffered from spine-associated complications and 27 (36.98%) individuals had a total of 37 relevant general complications. Urinary tract infection (n = 12), pneumonia (n = 5), and electrolyte disturbance (n = 9) were the most frequent complications. No cases of neurological impairment or cement leakage were observed. A mean LOS of 13.38 days (SD: 7.20) was reported. Clinically relevant screw loosening was observed in 5 (1.7%) of 292 implanted screws, all of whom required revision surgery. Furthermore, in four (5.48%) patients, secondary adjacent fractures were diagnosed during the follow-up period. Clinical outcomes are shown in Table 3, and complications are displayed in Table 4. Importantly, no significant difference in either clinical outcomes or complications were observed between groups according to the level of spinal fracture.
Radiological outcomes
The alpha-angle improved significantly after intervention with a mean of 5. 4° (4.1). No significant reduction loss (as determined by the alpha-angle changes) was encountered up to 24 months postoperatively (P = 0.18). Beta angles also improved significantly after surgery from 16.3 (7.5) to 10.8 (5.6). Midterm radiological follow-up demonstrated a significant increase in beta-angles with a value of 14.1 (6.2). Of note, no significant differences in the alpha and beta angles were observed between different spinal fracture levels at all follow-up time points (Table 5).
Midterm follow-up: functionality, pain, and quality of life after MIHS
After 24 months of follow-up, a COMI-back of 4.71 (2.65) was observed. VAS-back was higher than VAS-legs with values of 3.88 (2.39) vs. 2.5 (2.92), respectively. An EQ-5D-score of 0.57 (0.34) was found in the cohort. As displayed in Table 6, COMI-back was significantly higher in patients with fractures of the lumbar spine than in patients with more cranial fracture localizations.
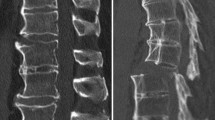
Clinical example
To illustrate the application and outcomes of the minimally invasive hybrid stabilization (MIHS) with double-threaded uncemented polyaxial screws, we present the following clinical case. A 76-year-old female patient presented with severe back pain following a minor fall. Radiological evaluation, including MRI and CT scans, revealed an unstable osteoporotic vertebral fracture classified as OF 4 involving the thoracolumbar region. The patient had a history of osteoporosis and was previously managed conservatively for similar issues. The patient underwent MIHS using double-threaded uncemented polyaxial screws. Under general anesthesia and in a prone position, a balloon-kyphoplasty was performed to restore vertebral height. This was followed by the fixation of the adjacent level above and below the fractured vertebra with double-threaded polyaxial screws (Longitude II Ballon Kyphon, Medtronic, Minneapolis, MN, USA). The screws were polyaxial and double-threaded (45 mm with cobalt-chromium alloy; Φ 6.5 mm) that provide better anchorage in cortical bone to reduce risk of implant loosening (Supplementary Fig. 1).
The procedure was completed in 90 min with minimal blood loss (< 100 ml). Intraoperative fluoroscopy confirmed appropriate placement and alignment of the screws and rods. Postoperative standing radiographs and CT scans showed satisfactory alignment and no evidence of screw loosening or cement leakage. The patient was mobilized on the second postoperative day and discharged home on postoperative day 10 with significant pain relief. At the 24-month follow-up, the patient reported a significant improvement in functionality and quality of life, with a VAS-back score of 2 and a COMI-back score of 3. Postoperative radiographs maintained the correction of kyphotic deformity with stable alpha and beta angles.
Noteworthy, for low-energy trauma cases, during initial evaluation, x-ray (showing fracture), CT, and MRIs (if T2 oedema in the vertebral body was noted, this indicated fresh/acute fracture) were done. After fixation and during the postoperative period, follow-up CT scans were done (X-ray was not routinely performed) to measure the alpha and beta angles.
Discussion
The current study is the first to demonstrate that MIHS with double-threated, uncemented screws for unstable osteoporotic vertebral fractures (OF 3 and 4) is associated with (1) adequate post-operative improvement of kyphosis as well as proper 2-year radiological follow-up results, (2) satisfactory midterm functional outcome, pain scores, and quality of life, and (3) low rates of spine-related complications, despite many systemic complications in this investigated geriatric population. Therefore, MIHS with double-treated pedicle screws should be considered a safe and feasible treatment concept for unstable OF-3 and 4 vertebral fractures. This paves the way for more widespread implementation of this cementless pedicle screw technique in the treatment of unstable OVFs.
Different surgical strategies for unstable OVFs have been described in the literature, and treatment guidelines differ between institutions [4, 5], with MIHS being the most commonly used surgical strategy (Table 7) based on the results of the EOFTT study [29]. In our institution, MIHS is considered as the treatment of choice for all patients suffering from unstable OVFs (defined as OF 3 with pedicle involvement and OF 4). Given the limitations of the OF-score for higher-grade injuries, it is not routinely performed nor integrated into our treatment guidelines [9]. Importantly, OF 5 fractures are generally treated with long-segment stabilization constructs.
It is believed that hybrid stabilization procedure optimizes construct stability, without requiring invasive anterior spine surgery. This construct functionally acts as a 360°-stabilization, which is indicated to avoid shear forces in patients with posterior cortex lesions and is associated with promising outcomes in most patients [30,31,32,33,34]. This study further shows that minimal invasive posterior spine surgery for OVFs is associated with short operative time, minimal blood loss, minimal postoperative pain, and short post-operative recovery times. Post-operative restoration of vertebral height in the current study was alike other studies on MIHS for OVFs [23, 32, 35, 36].In addition to others, we managed to further demonstrate adequate 2-year retainment of vertebral height and kyphosis correction.
The safety of MIHS for patients with unstable OVFs in our hands is underlined by the absence of neurological complications and postoperative mortality. Intervention-related complications, however, did occur. In 8 patients irrelevant cement leakage was diagnosed, although no leakage into the medullary canal was seen and no neurological deficits or indications for re-interventions/conversion existed. Screw loosening was diagnosed in 1.7% of screws. To avoid leakage as well as screw malpositioning we recommend probing all pedicles carefully in all quadrants. In addition, the instillation of cement should be performed under fluoroscopic control [32].
Osteoporosis largely affects pedicle screw fixation strength and bone marrow density correlates with pull-out strength [37,38,39]. To overcome these issues, augmentation of pedicle screws with cement has been introduced already in the 1980s [40]. Fenestrated pedicle screw cement augmentation was approved by the US Food and Drug Administration (FDA) in 2016 and is considered a safe and effective method to increase screw fixation strength in osteoporotic bone. Interestingly, despite the availability of a bulk of evidence on the biomechanical benefits of this technique, few proper studies report its safety and efficiency in a clinical setting [14, 41]. In addition, fenestrated screws are associated with increased epidural cement leakage, without increasing pull-out strength as compared with solid screws in a cadaveric model from Becker et al. [42]. Chen et al. further showed that fenestrated screws have inferior pull-out strengths than regular screws with pre-filling of the vertebra with PMMA [43]. This may be due to suboptimal cement distribution upon administration via fenestrated screws as they also observed that most of the cement left the fenestrated screw from the proximal fenestrations [41, 43]. Cement-augmented screw placement is associated with cement leakage as well. Rates of cement leakage vary between 20 and 93% [37, 38]. A systematic review reported risks of pulmonary embolisms up to 23% [44]. No consensus exists on the treatment of cement extravasation [45].
To prevent cement-related complications in MIHS we decided not to use cement-augmented screws and to focus on optimal design of other components of the fixation construct. To do so, we decided to focus on screw design and rod material. Regarding screw design, we utilized dual lead osteoporotic-specific pedicle screws as these screws demonstrated optimal pull-out properties in multiple biomechanical studies [46,47,48].
Different types of rod materials are available for spine surgery; however, cobalt-chrome rods are superior to titanium rods in corrective spinal surgery regarding postoperative stability. Therefore, cobalt-chrome rods are favoured in our institution for trauma cases as well [49]. PEEK devices have been used in the past, although due to high failure rates, we decided to phase out these rods before the start of this study [50].
Strengths and limitations
This study’s strengths lie in its large sample size of geriatric patients, which enhances the generalizability of our results, and the long follow-up period of 24 months, ensuring comprehensive understanding of long-term outcomes. Additionally, the availability of histopathological data enriches our analysis by correlating clinical outcomes with underlying biological mechanisms. These factors contribute to the robustness and clinical relevance of our findings, supporting the potential for MIHS with double-treated, uncemented screws to become a widely adopted treatment strategy for unstable osteoporotic vertebral fractures in elderly patients. However, our study is not without limitations. We were not able to add a control group to our dataset. Consequently, no comparative analysis has been performed. Therefore, upcoming multicentre studies should compare the outcome between different treatment protocols (incl. cemented screws and long-segment stabilizations) and further investigate the impact of spinal segmentation on the outcome. Especially for geriatric patients, in which follow-up studies are hard to perform. Furthermore, we did not compare the quality-of-life and functional outcomes of our patients with other geriatric patients without spinal fractures. Therefore, the natural course of spinal degeneration in elderly individuals was not adjusted for.
Conclusion
This prospective study is the first to demonstrate that MIHS is a safe and feasible treatment modality for unstable OVFs (OF 3 and 4) in the elderly. Complication rates are low, while radiological outcomes and midterm functional outcomes are satisfactory. The outcome of uncemented double-threated screws further equals the outcome of studies on cemented screws. These findings pave the way for more widespread implementation of MIHS with cementless pedicle screws in the treatment of unstable OVFs in elderly patients.
Data availability
Analyzed data in this research can be provided by the corresponding author upon reasonable request.
References
Ballane G, et al. Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int. 2017;28(5):1531–42.
Johnell O, Kanis JA. An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int. 2006;17(12):1726–33.
Widmer J, et al. Biomechanical contribution of spinal structures to stability of the lumbar spine-novel biomechanical insights. Spine J. 2020;20(10):1705–16.
Chmielnicki M, et al. Surgical and non-surgical treatment of vertebral fractures in Elderly. Z Orthop Unfall. 2019;157(6):654–67.
Kim SH, et al. A Randomized, endoscopist-blinded, prospective trial to compare the efficacy and patient tolerability between Bowel preparation protocols using sodium picosulfate magnesium citrate and polyethylene-glycol (1 L and 2 L) for colonoscopy. Gastroenterol Res Pract. 2020;2020:9548171.
Filippiadis DK, et al. Percutaneous vertebroplasty and kyphoplasty: current status, new developments and old controversies. Cardiovasc Intervent Radiol. 2017;40(12):1815–23.
Wei P, et al. Percutaneous kyphoplasty assisted with/without mixed reality technology in treatment of OVCF with IVC: a prospective study. J Orthop Surg Res. 2019;14(1):255.
Yan D, et al. Comparative study of percutaneous vertebroplasty and kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Arch Orthop Trauma Surg. 2011;131(5):645–50.
Schnake KJ, et al. Classification of osteoporotic thoracolumbar spine fractures: recommendations of the spine section of the German Society for Orthopaedics and Trauma (DGOU). Global Spine J. 2018;8(2 Suppl):s46-9.
Pingel A, Kandziora F, Hoffmann C-H. Osteoporotic L1 burst fracture treated by short-segment percutaneous stabilization with cement-augmented screws and kyphoplasty (hybrid technique). Eur Spine J. 2014;23(9):2022.
Rerikh VV, Sinyavin VD. Comparative radiological analysis of hybrid and circular stabilization methods for the treatment of osteoporotic vertebral burst fractures. Хирургия позвоночника. 2023;20(3):26–33.
Spiegl UJ, et al. Which anatomic structures are responsible for the reduction loss after hybrid stabilization of osteoporotic fractures of the thoracolumbar spine? BMC Musculoskelet Disord. 2020;21:1–8.
Spiegl UJ, et al. Hybrid stabilization of unstable osteoporotic thoracolumbar vertebral body fractures: clinical and radiological outcome after a mean of 4 years. Eur Spine J. 2019;28:1130–7.
Spiegl UJ, et al. Comparison of combined posterior and anterior spondylodesis versus hybrid stabilization in unstable burst fractures at the thoracolumbar spine in patients between 60 and 70 years of age. Arch Orthop Trauma Surg. 2018;138(10):1407–14.
Mueller JU, et al. Cement leakage in pedicle screw augmentation: a prospective analysis of 98 patients and 474 augmented pedicle screws. J Neurosurg: Spine. 2016;25(1):103–9.
Janssen I, et al. Risk of cement leakage and pulmonary embolism by bone cement-augmented pedicle screw fixation of the thoracolumbar spine. Spine J. 2017;17(6):837–44.
Mengis-Palleck CL, et al. Surgical site infection after polymethyl methacrylate pedicle screw augmentation in osteoporotic spinal vertebrae: a Series of 537 cases. Int J Spine Surg. 2023;17(4):587–97.
Doyle DJ, et al. American Society of Anesthesiologists Classification. Treasure Island: StatPearls; 2021.
Ulmar B, et al. Inter- and intraobserver reliability of the vertebral, local and segmental kyphosis in 120 traumatic lumbar and thoracic burst fractures: evaluation in lateral X-rays and sagittal computed tomographies. Eur Spine J. 2010;19(4):558–66.
Kuklo TR, et al. Measurement of thoracic and lumbar fracture kyphosis: evaluation of intraobserver, interobserver, and technique variability. Spine (Phila Pa 1976). 2001;26(1):61–5.
Cobb J. Outl Study Scoliosis. 1948;5:261–75.
Wu X, et al. Pedicle screw loosening: the value of radiological imagings and the identification of risk factors assessed by extraction torque during screw removal surgery. J Orthop Surg Res. 2019;14(1):6.
Clavien PA, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Chiarotto A, et al. Measurement properties of visual analogue scale, numeric rating scale, and pain severity subscale of the brief pain inventory in patients with low back pain: a systematic review. J Pain. 2019;20(3):245–63.
Mannion AF, et al. The Core Outcome measures Index (COMI) is a responsive instrument for assessing the outcome of treatment for adult spinal deformity. Eur Spine J. 2016;25(8):2638–48.
Ferrer M, et al. Validation of a minimum outcome core set in the evaluation of patients with back pain. Spine (Phila Pa 1976). 2006;31(12):1372–9.
Hong JY, et al. Quality of life analysis and smoking correlation in symptomatic spine osteoarthritis: a Nationwide Health Survey Analysis of an Elderly Population with EQ-5D. PLoS One. 2016;11(3):e0151315.
Mueller B, Carreon LY, Glassman SD. Comparison of the EuroQOL-5D with the Oswestry Disability Index, back and leg pain scores in patients with degenerative lumbar spine pathology. Spine (Phila Pa 1976). 2013;38(9):757–61.
Ullrich BW, et al. Georg Schmorl prize of the German spine society (DWG) 2022: current treatment for inpatients with osteoporotic thoracolumbar fractures—results of the EOFTT study. Eur Spine J. 2023;32(5):1525–35.
Spiegl U, et al. Osteoporotic vertebral body fractures of the thoracolumbar spine: indications and techniques of a 360°-stabilization. Eur J Trauma Emerg Surg. 2017;43(1):27–33.
Zairi F, et al. Minimally invasive management of thoraco-lumbar fractures: combined percutaneous fixation and balloon kyphoplasty. Orthop Traumatol Surg Res. 2012;98(6 Suppl):S105–11.
Hu X, et al. Posterior short segment fixation including the fractured vertebra combined with kyphoplasty for unstable thoracolumbar osteoporotic burst fracture BMC Musculoskelet Disord. 2020;21(1):1–6.
Fuentes S, et al. Percutaneous pedicle screw fixation and kyphoplasty for management of thoracolumbar burst fractures. Neurochirurgie. 2007;53(4):272–6.
Bironneau A, et al. Percutaneous internal fixation combined with kyphoplasty for neurologically intact thoracolumbar fractures: a prospective cohort study of 24 patients with one year of follow-up. Orthop Traumatol Surg Res. 2011;97(4):389–95.
Fuentes S, et al. Percutaneous kyphoplasty and pedicle screw fixation for the management of thoraco-lumbar burst fractures. Eur Spine J. 2010;19(8):1281–7.
Zairi F, et al. Minimally invasive percutaneous stabilization plus balloon kyphoplasty for the treatment of type a thoraco lumbar spine fractures: minimum 4 year’s follow-up. J Neurosurg Sci. 2014;58(3):169–75.
Hu SS. Internal fixation in the osteoporotic spine. Spine (Phila Pa 1976). 1997;22(24 Suppl):s43–8.
Halvorson TL, et al. Effects of bone mineral density on pedicle screw fixation. Spine (Phila Pa 1976). 1994;19(21):2415–20.
Bullmann V, et al. [Pedicle screw augmentation from a biomechanical perspective]. Orthopade. 2010;39(7):673–8.
Shea TM, et al. Designs and techniques that improve the pullout strength of pedicle screws in osteoporotic vertebrae: current status. Biomed Res Int. 2014;2014:748393.
Hirano T, et al. Structural characteristics of the pedicle and its role in screw stability. Spine (Phila Pa 1976). 1997;22(21):2504–9.
Becker S, et al. Assessment of different screw augmentation techniques and screw designs in osteoporotic spines. Eur Spine J. 2008;17(11):1462–9.
Chen LH, et al. Pullout strength of pedicle screws with cement augmentation in severe osteoporosis: a comparative study between cannulated screws with cement injection and solid screws with cement pre-filling. BMC Musculoskelet Disord. 2011;12:33.
Krueger A, et al. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009;18(9):1257–65.
Kerry G, Ruedinger C, Steiner HH. Cement embolism into the venous system after pedicle screw fixation: case report, literature review, and prevention tips. Orthop Rev (Pavia). 2013;5(3):e24.
Mehta H, et al. Biomechanical analysis of pedicle screw thread differential design in an osteoporotic cadaver model. Clin Biomech (Bristol Avon). 2012;27(3):234–40.
Seng WRD, et al. Pedicle screw designs in spinal surgery: is there a difference? A biomechanical study on primary and revision pull-out strength. Spine (Phila Pa 1976). 2019;44(3):E144–9.
Brasiliense LB, et al. Characteristics of immediate and fatigue strength of a dual-threaded pedicle screw in cadaveric spines. Spine J. 2013;13(8):947–56.
Shega FD, et al. Comparison of effectiveness between cobalt chromium rods versus titanium rods for treatment of patients with spinal deformity: a systematic review and meta-analysis. Adv Orthop. 2020;2020:p8475910.
Li C, et al. Clinical and biomechanical researches of polyetheretherketone (PEEK) rods for semi-rigid lumbar fusion: a systematic review. Neurosurg Rev. 2018;41(2):375–89.
Funding
Open Access funding enabled and organized by Projekt DEAL. This research did not receive financial support from any institutional or non-institutional organizations.
Author information
Authors and Affiliations
Contributions
M.A.M and M.T. were responsible for the conceptualization of this research, supervision, data accuracy checking, revising and editing the manuscript. A.A., M.G., and U.M. collected the data and conducted the data analysis, data visualization, and interpretation. C.H., C.B., M.P., and F.H. reviewed patients’ medical record, did the coding for the analysis, and designed the study Tables and Figures. S.O. and R.S. wrote the original draft of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Ethical approval
The study protocol was approved by the regional Ethics Committee of the study center (file number: 2016448).
Consent to participate
An informed consent was retrieved from all eligible individuals prior to participation in this research.
Consent for publication
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mahmoud, M.A., Afifi, A., Ghandour, M. et al. Satisfactory 2-year outcome of minimal invasive hybrid stabilization with double treated screws for unstable osteoporotic spinal fractures. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02645-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02645-1