Abstract
Introduction
Current treatment guidelines for patients with severe TBI (sTBI) are aimed at preventing secondary brain injury targeting specific endpoints of intracranial physiology to avoid the development of metabolic crisis. We sought to identify factors contributing to development of metabolic crisis in the setting of a Multi-modality Monitoring and Goal-Directed Therapy (MM&GDTP) approach to patients with severe TBI.
Methods
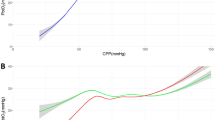
Prospective monitoring of sTBI patients was performed, with retrospective data analysis. MM&GDTP was targeted to intracranial pressure (ICP) ≤ 20 mmHg, cerebral perfusion pressure (CPP) ≥ 60 mmHg, brain tissue oxygen pressure (PbtO2) ≥ 20 mmHg, and cerebral oxygen extraction measured by bi-frontal Near infrared Spectroscopy (NIRS) > 55%. Brain flow abnormality was defined by one of the following combinations: CPP < 60 mmHg with NIRS < 55% (Type 1), CPP < 60 mmHg with PbtO2 < 20 mmHg (Type 2), or PbtO2 < 20 mmHg with NIRS < 55% (Type 3). Cerebral micro-dialysate was analyzed hourly for glucose, lactate, pyruvate, glutamate, glycerol, and lactate/pyruvate ratio (LPR). Statistical analysis was performed with student t-test, chi-square and Pearson’s tests as applicable.
Results
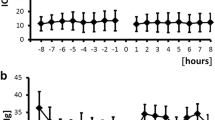
A total of 109,474 consecutive minutes of recorded multimodality monitoring was available for analysis. There was a significant difference in the number of minutes of brain flow abnormalities between survivors and non-survivors: 0.8% (875) versus 7.49% (8,199), respectively (p < 0.05). The duration of Type 1–3 flow abnormality per patient was higher in non-survivors (5.7 ± 2.5 h) compared to survivors (0.7 ± 0.6 h) as well as the duration of metabolic crisis, namely, 5.2 ± 2.2 versus 0.6 ± 1.0 h per patient. The occurrence of severe metabolic crisis was associated with a Type 2 flow abnormality (CPP < 60 mmHg and PbtO2 < 20 mmHg), r = 0.97, p < 0.001, but not with Type 1 and 3.
Conclusions
Metabolic crisis can occur despite a MM&GDTP approach aimed at optimizing cerebral blood flow. Severe metabolic crisis is associated to failure to maintain CPP and PbtO2 above 60 and 20 mmHg, respectively. The occurrence of severe metabolic crisis portends a poor prognosis in patients with sTBI.

Similar content being viewed by others
References
Langlois J, Rutland-Brown W, Wald M. The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil. 2006;21(5):375–8.
Thurman D, Alverson C, Dunn K, Guerrero J, Sniezek J. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14(6):602–15.
Brain Trauma Foundation American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe head injury. J Neurotrauma. 2007;24:S1–106.
Bratton SL, Chestnut RM, Ghajar J, McConnell HFF, Harris OA, Hartl R, Manley GT, Nemecek A, Newell DW, Rosenthal G, et al. Guidelines for the management of severe traumatic brain injury. X. Brain oxygen monitoring and thresholds. J Neurotrauma. 2007;24(Suppl 1):S65–70.
Brenner M, Stein DM, Hu PF, Aarabi B, Sheth K, Scalea TM. Traditional systolic blood pressure targets underestimate hypotension-induced secondary brain injury. J Trauma. 2012;72:1135–9.
MRC CrasH Collaborators. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336:425–9.
Stein SC, Georgoff P, Meghan S, Mirza KL, Falaky EI. Relationship of aggressive monitoring and treatment to improved outcomes in severe traumatic brain injury. J Neurosurg. 2010;112(5):1105–12.
Stein SC, Georgoff P, Meghan S, Mizra K, Sonnad SS. 150 years of treating severe traumatic brain injury: a systematic review of progress in mortality. J Neurotrauma. 2010;27(7):1343–53.
Stiefel MF, Udouteuk JD, Spiotta AM, Gracias VH, Goldberg A, Maloney-Wilensky E, Bloom S, LeRoux PD. Conventional neurocritical care and cerebral oxygenation after traumatic brain injury. J Neurosurg. 2006;105:568–75.
Bardt TF, Unterberg AW, Hartl R, Kiening KL, Schneider GH, Lanksch WR. Monitoring of brain tissue PO2 in traumatic brain injury: effect of cerebral hypoxia on outcome. Acta Neurochir Suppl. 1998;71:153–6.
Chang JJ, Youn TS, Benson D, Mattick H, Andrade N, Harper CR, Moore CB, Madden CJ, Diaz-Arrastia RR. Physiologic, functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37(1):283–90.
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS. Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med. 1998;26(9):1576–81.
Greer DM, Funk SE, Reaven NL, Ouzounelli M, Uman GC. Impact of fever on outcome in patients with stroke and neurological injury. Stroke. 2008;39:3029–35.
Siegal J, Kohli C. Correlation of noninvasive cerebral oximetry with cerebral perfusion in the severe head injured patient: a pilot study. J Trauma. 2002;52:40–6.
Hartl R, Gerber LM, Ni Q, Ghajar JG. Effect of early nutrition on deaths due to severe traumatic brain injury. J Neurosurg. 2008;109:50–6.
Timofeev I, Carpenter KLH, Nortje J, Al-Rawi PG, O’Connell MT, Czosnyka M, Smielewski P, Pickard JD, Menon DK, Kirkpatrick PJ, et al. Cerebral extracellular chemistry and outcome following traumatic brain injury: a Microdialysis study of 223 patients. Brain. 2011;1:1–11.
Stein NR, McArthur DL, Etchepare M, Vespa PM. Early cerebral metabolic crisis after TBI influences outcome despite adequate hemodynamic resuscitation. Neurocrit Care. 2012;17:49–57.
Nelson DW, Thornquist B, MacCallum RM, Nyström H, Holst A, Rudehill A, Wanacek M, Bellander BM, Weitzberg E. Analyses of cerebral microdialysis in patients with traumatic brain injury: relations to intracranial pressure, cerebral perfusions pressure and catheter placement. BMC Medicine. 2011;9:21.
Hutchinson PJ, Gupta AK, Fryer TF, Al-Rawi PG, Chatfield DA, Coles JP, O’Connell MT, Kett-White R, Minhas PS, Aigbirhio FI, et al. Correlation between cerebral blood flow, substrate delivery, and metabolism in head injury: a combined microdialysis and triple oxygen positron emission tomography study. J Cereb Blood Flow Metab. 2002;22(6):735–45.
Menon DK, Coles JP, Gupta AK, Fryer TD, Smielewski P, Chatfield DA, Aigbirhio F, Skepper JN, Minhas PS, Hutchinson PJ, et al. Diffusion limited oxygen delivery following head injury. Crit Care Med. 2004;32(6):1384–90.
Asgari S, Vespa P, Hu X. Is there any association between cerebral vasoconstriction/vasodilatation and microdialysis lactate to pyruvate ratio increase? Neurocrit Care. 2013;19(1):56–64.
Reinstrup P, Nordström CH. Prostacyclin infusion may prevent secondary damage in pericontusional brain tissue. Neurocrit Care. 2011;14:441–6.
Author information
Authors and Affiliations
Contributions
Design: CPM. Data acquisition: CS. Analysis: CPM. Interpretation of data: CPM. Drafting of the manuscript: CPM, KP, PP. Critical revision: CPM, PP, JM, VDD.
Corresponding author
Ethics declarations
Conflict of interest
Corrado P. Marini, Christy Stoller, John McNelis, Vito Del Deo, Kartik Prabhakaran, and Patrizio Petrone declare that they have not conflict of interest.
Informed consent
This study is a retrospective chart review, and as such, there is no need for an informed consent. The New York Medical College Institutional Review Board approved the study design and methodology.
Rights and permissions
About this article
Cite this article
Marini, C.P., Stoller, C., McNelis, J. et al. Correlation of brain flow variables and metabolic crisis: a prospective study in patients with severe traumatic brain injury. Eur J Trauma Emerg Surg 48, 537–544 (2022). https://doi.org/10.1007/s00068-020-01447-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-020-01447-5