Abstract
Introduction
Emergency laparotomy in patients over the age of 80 is associated with high morbidity and mortality. Accurate risk prediction in this patient population is desirable. Sarcopenia has been shown to be associated with outcome in multiple clinical settings and the psoas major muscle as measured on computed tomography (CT) imaging has been demonstrated as a marker of sarcopenia. We aim to assess the use of psoas major measurement on pre-operative CT as a prognostic indicator in over-80s undergoing emergency laparotomy and compare this measurement to P-POSSUM.
Methods
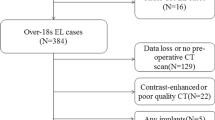
A retrospective interrogation of the prospectively collected National Emergency Laparotomy Database including all over-80s undergoing emergency laparotomy between January 2014 and September 2016 was conducted. Demographic, operative data and P-POSSUM data were collected and analysed. Computed tomography (CT) images were accessed and analysed, and cross-sectional areas of psoas major and the corresponding lumbar vertebral body at the level of the L3 inferior end plate were calculated. The ratio of psoas major-to-L3 cross-sectional area (PM:L3) was calculated for each patient. Mann–Whitney U test and receiver-operating characteristics (ROC) curves were used for statistical analysis.
Results
One hundred and three over-80s underwent emergency laparotomy. Male:female ratio was 60:43. Median age was 84 years (range 80–98 years). 30-day mortality was 19.4%.90-day mortality was 25.2%. Median PM:L3 ratio in patients who died as an inpatient was 0.3 and PM:L3 ratio in patients who survived to discharge was 0.52 (p < 0.0001). Median PM:L3 ratio in patient who died within 30 days post-op was 0.28 and 0.48 in those patients who survived to 30 days (p < 0.0001). Median PM:L3 ratio in patient who died within 90 days post-op was 0.28 and 0.51 in those patients who survived to 90 days (p < 0.0001). ROC analysis gave an area under the curve (AUC) of 0.85 for in-patient mortality, 0.86 for 30-day mortality, and 0.88 for 90-day mortality. ROC analysis for P-POSSUM in this data set demonstrated an AUC of 0.51 for in-patient mortality and 0.75 for 30- and 90-day mortality.
Conclusion
CT imaging of the abdomen and pelvis is routinely used in over-80s prior to emergency laparotomy making PM:L3 calculation feasible for the majority of patients in this group. PM:L3 ratio is a useful prognostic indicator for prediction of mortality in patients over the age of 80. PM:L3 is superior to the P-POSSUM score in this series.


Similar content being viewed by others
References
Cooper Z, Scott JW, Rosenthal RA, Mitchell SL. Emergency major abdominal surgical procedures in older adults: a systematic review of mortality and functional outcomes. J Am Geriatr Soc. 2015;63(12):2563–71.
Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ, UK Emergency Laparotomy Network. Variations in mortality after emergency laparotomy: the first report of the UK Emergency Laparotomy Network. Br J Anaesth. 2012;109(3):368–75.
Symons NR, Moorthy K, Almoudaris AM, Bottle A, Aylin P, Vincent CA, Faiz OD. Mortality in high-risk emergency general surgical admissions. Br J Surg. 2013;100(10):1318–25.
Fried LP, Xue QL, Cappola AR, Ferrucci L, Chaves P, Varadhan R, Guralnik JM, Leng SX, Semba RD, Walston JD, Blaum CS, Bandeen-Roche K. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol A Bio Sci Med Sci. 2009;64:1049–57.
Clegg A, Young J, Iliffe S, Rikkert MC, Rockwood K. Frailty in elderly people. Lancet. 2013;381(9868):752–62.
Gale C, Cooper C, Sayer AA. Prevalence of frailty and disability: findings from the English Longitudinal Study of Ageing. Age Ageing. 2015;44:162–5.
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, et al. Sarcopenia: European consensus on definition and diagnosis: report of the European Working Group on Sarcopenia in older people. Age Ageing. 2010;39:412–23.
Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, Landi F, Calvani R. Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res. 2017;29(1):19–27.
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355–66.
Lippi G, Sanchis-Gomar F, Montagnana M. Biological markers in older people at risk of mobility limitations. Curr Pharm Des. 2014;20(19):3222–44.
Rutten IJ, Ubachs J, Kruitwagen RF, et al. The influence of sarcopenia on survival and surgical complications in ovarian cancer patients undergoing primary debulking surgery. Eur J Surg Oncol. 2017;43(4):717–24.
Nyers ES, Brothers TE. Perioperative psoas to lumbar vertebral index does not successfully predict amputation-free survival after lower extremity revascularization. J Vasc Surg. 2017;66(6):1820–5.
Hawkins RB, Mehaffey JH, Charles EJ, Kern JA, Lim DS, Teman NR, Ailawadi G. Psoas muscle size predicts risk-adjusted outcomes after surgical aortic valve replacement. Ann Thorac Surg. 2018.
Paknikar R, Friedman J, Cron D, et al. Psoas muscle size as a frailty measure for open and transcatheter aortic valve replacement. J Thorac Cardiovasc Surg. 2016;151(3):745–51.
Jones KI, Doleman B, Scott S, Lund JN, Williams JP. Simple psoas cross-sectional area measurement is a quick and easy method to assess sarcopenia and predicts major surgical complications. Colorectal Dis. 2015;1:O20–6.
Drudi LM, Phung K, Ades M, Zuckerman J, Mullie L, Steinmetz OK, Obrand DI, Afilalo J. Psoas muscle area predicts all-cause mortality after endovascular and open aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2016;52:764–9.
Shirai H, Kaido T, Hamaguchi Y, et al. Preoperative low muscle mass and low muscle quality negatively impact on pulmonary function in patients undergoing hepatectomy for hepatocellular carcinoma. Liver Cancer. 2018;7(1):76–89.
Benjamin AJ, Buschmann MM, Zhang SQ, Wroblewski K, Kindler HL, Roggin KK, Dale W. The impact of changes in radiographic sarcopenia on overall survival in older adults undergoing different treatment pathways for pancreatic cancer. J Geriatr Oncol. 2018;9(4):367–72.
Hawkins RB, Mehaffey JH, Charles EJ, Kern JA, Lim DS, Teman NR, Ailawadi G. Psoas muscle size predicts risk-adjusted outcomes after surgical aortic valve replacement. Ann Thorac Surg. 2018;106(1):39–45.
Trotter J, Johnston J, Ng A, Gatt M, MacFie J, McNaught C. Is sarcopenia a useful predictor of outcome in patients after emergency laparotomy? A study using the NELA database. Ann R Coll Surg Engl. 2018 27:1–5.
Wagner D, DeMarco MM, Amini N, Buttner S, Segev D, Gani F, Pawlik TM. Role of frailty and sarcopenia in predicting outcomes among patients undergoing gastrointestinal surgery. World J Gastrointest Surg. 2016;8(1):27–40.
Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–60.
Kulkarni SV, Naik AS, Subramanian N Jr. APACHE-II scoring system in perforative peritonitis. Am J Surg. 2007;194:549–52.
Moonesinghe SR, Mythen MG, Das P, Rowan KM, Grocott MP. Risk stratification tools for predicting morbidity and mortality in adult patients undergoing major surgery: qualitative systematic review. Anaesthesiology. 2013;119(4):959–81.
Teixeira IM, Teles AR, Castro JM, Azevedo LF, Mourão JB. Physiological and operative severity score for the enumeration of mortality and morbidity (POSSUM) system for outcome prediction in elderly patients undergoing major vascular surgery. J Cardiothorac Vasc Anesth. 2018;32(2):960–7.
Sharrock AE, McLachlan J, Chambers R, Bailey IS, Kirkby-Bott J. Emergency abdominal surgery in the elderly: can we predict mortality? World J Surg. 2017;41(2):402–9.
NELA Risk Calculator. http://Data.nela.org.uk/riskcalculator. Accessed 2 Sep 2018.
Dirks RC, Edwards BL, Tong E, Schaheen B, Turrentine FE, Shada A, Smith PW. Sarcopenia in emergency abdominal surgery. J Surg Res. 2017;207:13–21.
Kaplan SJ, Pham TN, Arbabi S, et al. Association of radiologic indicators of frailty with 1-year mortality in older trauma patients: opportunistic screening for sarcopenia and osteopenia. JAMA Surg. 2017;152(2):e164604.
Ebbeling L, Grabo DJ, Shashaty M, et al. Psoas:lumbar vertebra index: central sarcopenia independently predicts morbidity in elderly trauma patients. Eur J Trauma Emerg Surg. 2014;40(1):57–65.
Margadant CC, Bruns ER, Sloothaak DA, et al. Lower muscle density is associated with major postoperative complications in older patients after surgery for colorectal cancer. Eur J Surg Oncol. 2016;42(11):1654–9.
Namm JP, Thakrar KH, Wang CH, et al. A semi-automated assessment of sarcopenia using psoas area and density predicts outcomes after pancreaticoduodenectomy for pancreatic malignancy. J Gastrointest Oncol. 2017;8(6):936–44.
Joglekar S, Asghar A, Mott SL, et al. Sarcopenia is an independent predictor of complications following pancreatectomy for adenocarcinoma. J Surg Oncol. 2015;111(6):771–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mr Gregory Simpson states that he has no conflict of interest. Mr Alex Parker states that he has no conflict of interest. Mr Philip Hopley states that he has no conflict of interest. Mr Jeremy Wilson states that he has no conflict of interest. Mr Conor Magee states that he has no conflict of interest.
Research involving human participants and/or animals
For this type of study, formal consent is not required.
Informed consent
Institutional review board and informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Simpson, G., Parker, A., Hopley, P. et al. Pre-operative psoas major measurement compared to P-POSSUM as a prognostic indicator in over-80s undergoing emergency laparotomy. Eur J Trauma Emerg Surg 46, 215–220 (2020). https://doi.org/10.1007/s00068-018-1025-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-1025-5