Abstract
Introduction
Emergency laparotomy is a considerable component of a colorectal surgeon’s workload and conveys substantial morbidity and mortality, particularly in older patients. Frailty is associated with poorer surgical outcomes. Frailty and sarcopenia assessment using Computed Tomography (CT) calculation of psoas major area predicts outcomes in elective and emergency surgery. Current risk predictors do not incorporate frailty metrics. We investigated whether sarcopenia measurement enhanced mortality prediction in over-65 s who underwent emergency laparotomy and emergency colorectal resection.
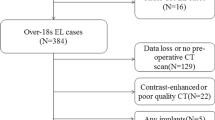
Methods
An analysis of data collected prospectively during the National Emergency Laparotomy Audit (NELA) was conducted. Psoas major (PM) cross-sectional area was measured at the L3 level and a ratio of PM to L3 vertebral body area (PML3) was calculated. Outcome measures included inpatient, 30-day and 90-day mortality. Statistical analysis was conducted using Mann–Whitney, Chi-squared and receiver operating characteristics (ROC). Logistic regression was conducted using P-POSSUM variables with and without the addition of PML3.
Results
Nine-hundred and forty-four over-65 s underwent emergency laparotomy from three United Kingdom hospitals were included. Median age was 76 years (IQR 70–82 years). Inpatient mortality was 21.9%, 30-day mortality was 16.3% and 90-day mortality was 20.7%. PML3 less than 0.39 for males and 0.31 for females indicated significantly worse outcomes (inpatient mortality 68% vs 5.6%, 30-day mortality 50.6% vs 4.0%,90-day mortality 64% vs 5.2%, p < 0.0001). PML3 was independently associated with mortality in multivariate analysis (p < 0.0001). Addition of PML3 to P-POSSUM variables improved area under the curve (AUC) on ROC analysis for inpatient mortality (P-POSSUM:0.78 vs P-POSSUM + PML3:0.917), 30-day mortality(P-POSSUM:0.802 vs P-POSSUM + PML3: 0.91) and 90-day mortality (P-POSSUM:0.79 vs P-POSSUM + PML3: 0.91).
Conclusion
PML3 is an accurate predictor of mortality in over-65 s undergoing emergency laparotomy. Addition of PML3 to POSSUM appears to improve mortality risk prediction.





Similar content being viewed by others
Availability of data and material
Data can be made available upon request.
References
Cooper Z, Scott JW, Rosenthal RA, Mitchell SL. Emergency major abdominal surgical procedures in older adults: a systematic review of mortality and functional outcomes. J Am Geriatr Soc. 2015;63(12):2563–71.
Saunders DI, Murray D, Pichel AC, Varley S, Peden CJ. UK emergency laparotomy network. Variations in mortality after emergency laparotomy: the first report of the UK emergency laparotomy network. Br J Anaesth. 2012;109(3):368–75.
Symons NR, Moorthy K, Almoudaris AM, Bottle A, Aylin P, Vincent CA, Faiz OD. Mortality in high-risk emergency general surgical admissions. Br J Surg. 2013;100(10):1318–25.
The Royal College of Surgeons of Great Britain and Ireland. The higher risk general surgical patient. Towards improved care for a forgotten group. 2011. https://www.rcseng.ac.uk/library-and-publications/rcs-publications/docs/the-higher-risk-general-surgical-patient/. Accessed May 2020.
London R.NELA project team. Second patient report of the national emergency laparotomy audit. 2016. http://www.nela.org.uk/reports. Accessed 28 Aug 2019.
Copeland GP, Jones D, Walters M. POSSUM: a scoring system for surgical audit. Br J Surg. 1991;78:355–60.
Kulkarni SV, Naik AS, Subramanian N Jr. APACHE-II scoring system in perforative peritonitis. Am J Surg. 2007;194:549–52.
Moonesinghe SR, Mythen MG, Das P, Rowan KM, Grocott MP. Risk stratification tools for predicting morbidity and mortality in adult patients undergoing major surgery: qualitative systematic review. Anaesthesiology. 2013;119(4):959–81.
NELA and Possum differences. National emergency laparotomy audit. https://www.nela.org.uk/NELA-POSSUM-Differences. Accessed 28 Aug 2019)
Wakabayashi H, Sano T, Yachida S, Okano K, Izuishi K, Suzuki Y. Validation of risk assessment scoring systems for an audit of elective surgery for gastrointestinal cancer in elderly patients: an audit. Int J Surg. 2007;5(5):323–7.
Loc PTB, du Montcel ST, Duron JJ, Levard H, Suc B, Descottes B, et al. Elderly POSSUM, a dedicated score for prediction of mortality and morbidity after major colorectal surgery in older patients. Br J Surg. 2010;97(3):396–403.
Fried LP, Xue QL, Cappola AR, Ferrucci L, Chaves P, Varadhan R, Guralnik JM, Leng SX, Semba RD, Walston JD, Blaum CS, Bandeen-Roche K. Nonlinear multisystem physiological dysregulation associated with frailty in older women: implications for etiology and treatment. J Gerontol A Bio Sci Med Sci. 2009;64:1049–57.
Clegg A, Young J, Iliffe S, Rikkert MC, Rockwood K. Frailty in elderly people. The Lancet. 2013;381(9868):752–62.
Tosato M, Marzetti E, Cesari M, Savera G, Miller RR, Bernabei R, Landi F, Calvani R. Measurement of muscle mass in sarcopenia: from imaging to biochemical markers. Aging Clin Exp Res. 2017;29(1):19–27.
Simpson G, Manu N, Magee C, Wilson J, Moug S5 Vimalachandran D. Measuring sarcopenia on pre-operative CT in older adults undergoing emergency laparotomy: a comparison of three different calculations. Int J Colorectal Disease. 2020 Mar 25.
Jones KI, Doleman B, Scott S, Lund JN, Williams JP. Simple psoas cross-sectional area measurement is a quick and easy method to assess sarcopenia and predicts major surgical complications. Colorectal Dis. 2015;1:O20–6.
Drudi LM, Phung K, Ades M, Zuckerman J, Mullie L, Steinmetz OK, Obrand DI, Afilalo J. Psoas muscle area predicts all- cause mortality after endovascular and open aortic aneurysm repair. Eur J Vasc Endovasc Surg. 2016;52:764–9.
Shirai H, Kaido T, Hamaguchi Y, et al. Preoperative low muscle mass and low muscle quality negatively impact on pulmonary function in patients undergoing hepatectomy for hepatocellular carcinoma. Liver Cancer. 2018;7(1):76–89.
Smith AB, Deal AM, Yu H, Boyd B, Matthews J, Wallen EM, et al. Sarcopenia as a predictor of complications and survival following radical cystectomy. J Urol. 2014;191(6):1714–20.
Dirks RC, Edwards BL, Tong E, Schaheen B, Turrentine FE, Shada A, et al. Sarcopenia in emergency abdominal surgery. J Surg Res. 2017;207:13–21.
Hajibandeh S, Hajibandeh S, Jarvis R, Bhogal T, Dalmia S. Meta-analysis of the effect of sarcopenia in predicting postoperative mortality in emergency and elective abdominal surgery. Surgeon. 2019;17(6):370–80 (pii: S1479-666X(18)30119-7).
Agha R, Abdall-Razak A, Crossley E, Dowlut N, Iosifidis C, Mathew G, for the STROCSS Group. The STROCSS 2019 guideline: strengthening the reporting of cohort studies in surgery. Int J Surg. 2019;72:156–65.
Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: a review. Eur J Intern Med. 2016;31:3–10.
Parmar KL, Law J, Carter B, Hewitt J, Boyle JM, Casey P, et al. Frailty in older patients undergoing emergency laparotomy: results from the UK observational Emergency Laparotomy and Frailty (ELF) Study. Ann Surg. 2019;7(10):e017928.
Joseph B, Zangbar B, Pandit V, Fain M, Mohler MJ, Kulvatunyou N, et al. Emergency general surgery in the elderly: too old or too frail? J Am Coll Surg. 2016;222(5):805–13.
Orouji Jokar T, Ibraheem K, Rhee P, Kulavatunyou N, Haider A, Phelan HA, et al. Emergency general surgery specific frailty index: a validation study. J Trauma Acute Care Surg. 2016;81(2):254–60.
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J. Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc. 2015;74(4):355–66.
Montgomery v Lanarkshire Health Board. 2015. SC 11 [2015] 1 AC 1430.
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
GS: data collection, analysis, write up of article. JW: data collection, study design, write up of article. DV: write up of article, study design. FM: data collection, write up of article. CM: supervising author, study design, write up of article.
Corresponding author
Ethics declarations
Conflict of interest
No conflicts of interest or competing interests to declare.
Ethics approval
No ethical approval required as study of a retrospective, observational design. No intervention made in patients care.
Consent to participate
Consent to participate has been gained.
Appendix
Appendix
Multivariate analysis of pre-operative factors and mortality.
Inpatient mortality | 30-day mortality | 90-day mortality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Sig | OR | 95% CI | Sig | OR | 95% CI | Sig | OR | 95% CI | ||||
Critical care stay (days) | 0.916 | 1.040 | 0.496 | 2.181 | 0.967 | 0.984 | 0.452 | 2.139 | 0.751 | 0.886 | 0.418 | 1.875 |
Time to theatre (hours) | 0.889 | 1.003 | 0.968 | 1.038 | 0.482 | 1.012 | 0.979 | 1.046 | 0.836 | 0.996 | 0.959 | 1.034 |
PML3 | 0.000 | 11.031 | 5.359 | 16.272 | 0.000 | 10.125 | 5.612 | 17.702 | 0.000 | 11.243 | 5.481 | 16.956 |
ASA | 0.000 | 0.000 | 0.000 | |||||||||
ASA 1 (ref) | ||||||||||||
ASA 2 | 0.293 | 0.346 | 0.048 | 2.500 | 0.129 | 0.217 | 0.030 | 1.557 | 0.227 | 0.298 | 0.042 | 2.126 |
ASA 3 | 0.488 | 0.509 | 0.075 | 3.437 | 0.193 | 0.285 | 0.043 | 1.884 | 0.553 | 0.565 | 0.086 | 3.727 |
ASA 4 | 0.487 | 1.966 | 0.293 | 13.208 | 0.797 | 1.278 | 0.197 | 8.286 | 0.460 | 2.036 | 0.309 | 13.405 |
ASA 5 | 0.179 | 4.776 | 0.488 | 46.754 | 0.164 | 4.965 | 0.520 | 47.362 | 0.140 | 5.528 | 0.571 | 53.512 |
Age | 0.403 | 1.017 | 0.978 | 1.056 | 0.614 | 1.010 | 0.954 | 1.053 | 0.937 | 1.002 | 0.963 | 1.042 |
Blood loss | 0.031 | 0.006 | 0.010 | |||||||||
< 100 ml (ref) | ||||||||||||
101–500 ml | 0.021 | 2.225 | 1.126 | 4.396 | 0.001 | 3.670 | 1.675 | 8.042 | 0.004 | 2.814 | 1.389 | 5.702 |
501–999 ml | 0.316 | 2.071 | 0.498 | 8.603 | 0.148 | 3.022 | 0.674 | 13.546 | 0.210 | 2.556 | 0.589 | 11.096 |
> 1000 ml | 0.014 | 10.183 | 1.597 | 64.949 | 0.014 | 9.348 | 1.569 | 55.708 | 0.012 | 11.221 | 1.704 | 73.887 |
Soiling | 0.084 | 0.084 | 0.332 | |||||||||
None (ref) | ||||||||||||
Serous fluid | 0.292 | 1.502 | 0.705 | 3.202 | 0.255 | 1.611 | 0.709 | 3.663 | 0.473 | 1.327 | 0.612 | 2.876 |
Localised pus | 0.362 | 0.574 | 0.174 | 1.894 | 0.750 | 1.211 | 0.373 | 3.936 | 0.532 | 0.689 | 0.215 | 2.213 |
Free pus, blood or bowel content | 0.044 | 2.029 | 1.020 | 4.035 | 0.216 | 1.581 | 0.765 | 3.270 | 0.146 | 1.680 | 0.835 | 3.380 |
Malignancy | 0.453 | 0.221 | 0.608 | |||||||||
None (ref) | ||||||||||||
Primary only | 0.567 | 0.771 | 0.317 | 1.876 | 0.047 | 0.328 | 0.109 | 0.987 | 0.761 | 0.873 | 0.363 | 2.099 |
Nodal metastases | 0.742 | 1.294 | 0.278 | 6.023 | 0.778 | 1.253 | 0.261 | 6.013 | 0.853 | 1.161 | 0.239 | 5.638 |
Distant metastases | 0.160 | 2.175 | 0.735 | 6.429 | 0.557 | 0.683 | 0.192 | 2.435 | 0.207 | 2.042 | 0.674 | 6.183 |
Multivariate analysis of P-POSSUM variables with PML3.
Inpatient mortality | 30-day mortality | 90-day mortality | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
Sig | OR | 95% CI | Sig | OR | 95% CI | Sig | OR | 95% CI | ||||
Age | 0.091 | 1.028 | 0.996 | 1.061 | 0.301 | 1.018 | 0.984 | 1.053 | 0.780 | 1.005 | 0.972 | 1.038 |
Creatinine | 0.001 | 1.006 | 1.002 | 1.010 | 0.048 | 1.004 | 1.000 | 1.007 | 0.001 | 1.006 | 1.003 | 1.010 |
Sodium | 0.199 | 1.030 | 0.985 | 1.076 | 0.227 | 1.029 | 0.982 | 1.078 | 0.079 | 1.042 | 0.995 | 1.092 |
Potassium | 0.658 | 0.916 | 0.621 | 1.350 | 0.956 | 1.012 | 0.670 | 1.528 | 0.416 | 0.847 | 0.568 | 1.263 |
Urea | 0.281 | 1.009 | 0.993 | 1.026 | 0.301 | 1.009 | 0.992 | 1.027 | 0.316 | 1.009 | 0.992 | 1.026 |
Haemoglobin | 0.021 | 0.988 | 0.978 | 0.998 | 0.334 | 0.995 | 0.984 | 1.005 | 0.036 | 0.989 | 0.979 | 0.999 |
WCC | 0.663 | 0.996 | 0.979 | 1.014 | 0.648 | 0.996 | 0.978 | 1.014 | 0.717 | 0.997 | 0.980 | 1.014 |
Pulse | 0.254 | 1.007 | 0.995 | 1.020 | 0.687 | 1.003 | 0.989 | 1.016 | 0.446 | 1.005 | 0.992 | 1.018 |
BP | 0.434 | 0.996 | 0.987 | 1.006 | 0.019 | 0.988 | 0.978 | 0.998 | 0.381 | 0.996 | 0.986 | 1.005 |
GCS | 0.349 | 0.940 | 0.825 | 1.070 | 0.371 | 0.943 | 0.828 | 1.073 | 0.340 | 0.937 | 0.821 | 1.071 |
ECG | 0.279 | 0.115 | 0.309 | |||||||||
Normal (ref) | ||||||||||||
AF, rate 60–90 | 0.154 | 1.840 | 0.796 | 4.254 | 0.039 | 2.495 | 1.047 | 5.945 | 0.187 | 1.794 | 0.753 | 4.272 |
Any other abnormality | 0.750 | 0.911 | 0.512 | 1.619 | 0.748 | 1.103 | 0.606 | 2.009 | 0.693 | 0.887 | 0.488 | 1.610 |
Cardiac | 0.603 | 0.118 | 0.628 | |||||||||
No cardiac failure (ref) | ||||||||||||
Diuretic, digoxin, Rx for angina/HTN | 0.283 | 1.347 | 0.783 | 2.318 | 0.038 | 1.818 | 1.033 | 3.199 | 0.193 | 1.452 | 0.828 | 2.546 |
Peripheral oedema, warfarin, borderline cardiomyopathy | 0.770 | 0.884 | 0.386 | 2.023 | 0.643 | 0.813 | 0.338 | 1.956 | 0.757 | 1.144 | 0.488 | 2.678 |
Raised JVP, cardiomegaly | 0.763 | 0.804 | 0.195 | 3.325 | 0.770 | 1.234 | 0.302 | 5.050 | 0.902 | 1.095 | 0.259 | 4.633 |
Respiratory | 0.007 | 0.021 | 0.016 | |||||||||
No dyspnoea | ||||||||||||
Dyspnoea on exertion, mild COAD | 0.516 | 0.824 | 0.460 | 1.477 | 0.260 | 0.699 | 0.375 | 1.303 | 0.873 | 0.952 | 0.524 | 1.732 |
Limiting dyspnoea, moderate COAD | 0.105 | 1.749 | 0.890 | 3.437 | 0.188 | 1.598 | 0.795 | 3.211 | 0.148 | 1.675 | 0.833 | 3.368 |
Dyspnoea at rest, pulmonary fibrosis | 0.005 | 3.878 | 1.510 | 9.956 | 0.031 | 2.812 | 1.100 | 7.193 | 0.004 | 4.086 | 1.560 | 10.698 |
Operative severity | 0.784 | 1.072 | 0.653 | 1.760 | 0.402 | 1.249 | 0.743 | 2.098 | 0.813 | 0.940 | 0.565 | 1.565 |
No. of operations | 0.619 | 0.710 | 0.507 | |||||||||
One (ref) | ||||||||||||
Two | 0.633 | 0.832 | 0.391 | 1.772 | 0.843 | 0.923 | 0.417 | 2.041 | 0.672 | 0.845 | 0.387 | 1.846 |
More than 2 | 0.423 | 2.687 | 0.239 | 30.170 | 0.438 | 2.467 | 0.252 | 24.149 | 0.300 | 3.663 | 0.315 | 42.611 |
Blood loss | 0.020 | 0.012 | 0.005 | |||||||||
< 100mls (ref) | ||||||||||||
101–500 mls | 0.062 | 1.679 | 0.974 | 2.894 | 0.006 | 2.320 | 1.277 | 4.213 | 0.014 | 2.041 | 1.152 | 3.617 |
501–999 mls | 0.825 | 1.158 | 0.314 | 4.268 | 0.915 | 1.077 | 0.278 | 4.166 | 0.791 | 1.200 | 0.312 | 4.612 |
> 1000 mls | 0.004 | 9.641 | 2.106 | 44.133 | 0.020 | 7.039 | 1.352 | 36.643 | 0.002 | 12.044 | 2.536 | 57.200 |
Peritoneal soiling | 0.180 | 0.391 | 0.288 | |||||||||
No soiling(ref) | ||||||||||||
Minor soiling | 0.559 | 1.195 | 0.657 | 2.175 | 0.239 | 1.482 | 0.770 | 2.851 | 0.434 | 1.282 | 0.688 | 2.391 |
Local pus | 0.636 | 0.787 | 0.292 | 2.119 | 0.947 | 1.037 | 0.357 | 3.012 | 0.777 | 0.862 | 0.308 | 2.413 |
Free bowel content, pus or blood | 0.061 | 1.793 | 0.974 | 3.302 | 0.117 | 1.672 | 0.880 | 3.176 | 0.086 | 1.740 | 0.925 | 3.273 |
Malignancy | 0.194 | 0.045 | 0.055 | |||||||||
Not malignant (ref) | ||||||||||||
Primary malignancy only | 0.281 | 0.672 | 0.326 | 1.385 | 0.005 | 0.289 | 0.122 | 0.686 | 0.280 | 0.663 | 0.315 | 1.398 |
Malignancy + nodal mets | 0.469 | 1.535 | 0.481 | 4.901 | 0.514 | 0.652 | 0.181 | 2.355 | 0.891 | 0.918 | 0.270 | 3.124 |
Malignancy + distant mets | 0.110 | 2.014 | 0.853 | 4.757 | 0.683 | 0.821 | 0.320 | 2.112 | 0.017 | 2.884 | 1.209 | 6.881 |
PML3 | 0.000 | 12.782 | 7.900 | 18.462 | 0.000 | 10.716 | 6.735 | 17.273 | 0.000 | 13.135 | 7.974 | 20.995 |
*Age, creatinine, sodium, potassium, urea, haemoglobin, WCC, pulse, BP and GCS included as ordinal data. ECG, cardiac and respiratory findings, operative severity, no. of operation, blood loss, peritoneal soiling, malignancy and PML3 included as nominal data. Cut-off for PML3 was 0.35.
Rights and permissions
About this article
Cite this article
Simpson, G., Wilson, J., Vimalachandran, D. et al. Sarcopenia estimation using psoas major enhances P-POSSUM mortality prediction in older patients undergoing emergency laparotomy: cross-sectional study. Eur J Trauma Emerg Surg 48, 2003–2012 (2022). https://doi.org/10.1007/s00068-021-01669-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-021-01669-1