Abstract
Purpose
This article reports experiences with 3T magnetic resonance imaging(MRI)-guided brachytherapy (BT) for cervical cancer focusing on late side effects.
Methods
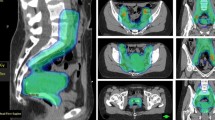
Between June 2012 and March 2017 a total of 257 uterovaginal BT administrations were performed in 61 consecutive patients with inoperable cervical cancer. All patients were treated with BT combined with external beam radiotherapy.
Results
The mean HR-CTV (high risk-clinical target volume) D90 was 87 ± 5.1 Gy equivalent dose corresponding to the conventional fractionation using 2 Gy per fraction (EQD2, range 70.7–97.9 Gy). The mean doses in OAR (organs at risk), namely rectum, sigmoid and bladder were D2 cm3rectum = 62.6 ± 6.9 Gy EQD2 (range 38.2–77.2 Gy), D2 cm3sigmoid = 66.2 ± 6.8 Gy EQD2 (43.2–78.6 Gy) and D2 cm3bladder = 75.1 ± 8.3 Gy EQD2 (58.2–92.6 Gy). There were no signs of late gastrointestinal (GI) toxicity in 49 patients, grade 3 toxicity was seen in 2 patients and grade 4 toxicity in 3 patients. There were no signs of late genitourinary (GU) toxicity in 41 patients, grade 3 toxicity was seen in 4 patients and no signs of grade 4 toxicity were seen. After the treatment, 60 patients (98.4%) achieved locoregional remission. In 54 patients (88.5%) the remission was complete, whereas in 6 patients (9.8%) remission was partial.
Conclusion
The use of 3T MRI-guided BT leads to achievement of high rates of local control with limited late morbidity as demonstrated in this series of patients.
Zusammenfassung
Zweck
Wir berichten über unsere Erfahrungen mit der 3T-MRT-gesteuerten Brachytherapie (BT) bei Gebärmutterhalskrebs, wobei wir uns auf späte Nebenwirkungen konzentrieren.
Methoden
Zwischen Juni 2012 und März 2017 haben wir bei 61 konsekutiven Patientinnen mit inoperablem Zervixkarzinom insgesamt 257 uterovaginale BT-Behandlungen durchgeführt. Alle Patientinnen wurden mit BT in Kombination mit perkutaner Strahlentherapie behandelt.
Ergebnisse
Die mittlere „high-risk clinical target volume“ (HR-CTV) D90 betrug 87 + 5,1 Gy EQD2 (Spanne 70,7–97,9). Die mittleren Dosen in „organs at risk“ (OAR), nämlich im Rektum, Sigmoideum und Blase, waren D2 cm3Rektum = 62,6 + 6,9 Gy EQD2 (Spanne von 38,2–77,2), D2 cm3Sigmoideum = 66,2 + 6,8 Gy EQD2 (Spanne 43,2–78,6) und D2 cm3Blase = 75,1 + 8,3 EQD2 (Spanne 58,2–92,6). Bei 49 Patientinnen traten keine Anzeichen einer späten gastrointestinalen (GI) Toxizität auf; bei 2 Patientinnen wurden Grad-3-Toxizitäten und bei 3 Patienten Grad-4-Toxizitäten beobachtet. Bei 41 Patientinnen traten keine Anzeichen einer späten urogenitalen (GU) Toxizität auf, bei 4 Patientinnen wurde eine Toxizität vom Grad 3 beobachtet; Anzeichen für eine Toxizität vom Grad 4 ergaben sich nicht. Nach der Behandlung erreichten 60 Patientinnen (98,4 %) lokoregionale Remission. Bei 54 Patientinnen (88,5 %) handelte sich um eine vollständige Remission, bei 6 Patientinnen (9,8 %) um eine partielle lokoregionale Remission.
Schlussfolgerungen
Die Anwendung von 3T-MRT-gesteuerter BT führt zu hohen lokalen Kontrollraten mit begrenzter Spätmorbidität, wie in unserer Patientengruppe gezeigt wurde.




Similar content being viewed by others
References
Ferlay J, Soerjomataram I, Dikshit R et al (2015) Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136(5):E359–E386
Viswanathan AN, Thomadsen B, American Brachytherapy Society Cervical Cancer Recommendations Committee, American Brachytherapy Society (2012) American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part I: General principles. Brachytherapy 11(1):33–46
Green JA, Kirwan JM, Tierney JF et al (2001) Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: A systematic review and meta-analysis. Lancet 358(9284):781–786
Shin KH, Kim TH, Cho JK et al (2006) CT-guided intracavitary radiotherapy for cervical cancer: Comparison of conventional point A plan with clinical target volume-based three-dimensional plan using dose-volume parameters. Int J Radiat Oncol Biol Phys 64(1):197–204
Dolezel M, Vanásek J, Odrázka K, Tichý M (2008) The progress in the treatment of cervical cancer-3D brachytherapy CT/MR-based planning. Ceska Gynekol 73(3):144–149
Haie-Meder C, Pötter R, Van Limbergen E et al (2005) Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol 74(3):235–245
Pötter R, Haie-Meder C, Van Limbergen E et al (2006) Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol 78(1):67–77
Pötter R, Dimopoulos J, Bachtiary B et al (2006) 3D conformal HDR-brachy- and external beam therapy plus simultaneous cisplatin for high-risk cervical cancer: Clinical experience with 3 year follow-up. Radiother Oncol 79(1):80–86
Pötter R, Dimopoulos J, Georg P et al (2007) Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol 83(2):148–155
Dimopoulos JC, Lang S, Kirisits C et al (2009) Dose-volume histogram parameters and local tumor control in magnetic resonance image-guided cervical cancer brachytherapy. Int J Radiat Oncol Biol Phys 75(1):56–63
Vojtíšek R, Mouryc F, Cechová D et al (2014) MRI based 3D brachytherapy planning of the cervical cancer – Our experiences with the use of the uterovaginal Vienna Ring MR CT applicator. Klin Onkol 27(1):45–51
Viswanathan AN, Beriwal S, De Los Santos JF et al (2012) American Brachytherapy Society consensus guidelines for locally advanced carcinoma of the cervix. Part II: High-dose-rate brachytherapy. Brachytherapy 11(1):47–52
Lang S, Kirisits C, Dimopoulos J et al (2007) Treatment planning for MRI assisted brachytherapy of gynecologic malignancies based on total dose constraints. Int J Radiat Oncol Biol Phys 69(2):619–627
National Cancer Institute (2010) Common terminology criteria for adverse events (CTCAE). Version 4.0 (v4.03: June 14, 2010)
Pötter R, Federico M, Sturdza A, Fotina I, Hegazy N, Schmid M, Kirisits C, Nesvacil N (2016) Value of magnetic resonance imaging without or with applicator in place for target definition in cervix cancer brachytherapy. Int J Radiat Oncol Biol Phys 94(3):588–597
Viswanathan AN, Erickson B, Gaffney DK, Beriwal S, Bhatia SK, Lee Burnett O 3rd et al (2014) Comparison and consensus guidelines for delineation of clinical target volume for CT- and MR-based brachytherapy in locally advanced cervical cancer. Int J Radiat Oncol Biol Phys 90(2):320–328
Krishnatry R, Patel FD, Singh P, Sharma SC, Oinam AS, Shukla AK (2012) CT or MRI for image-based brachytherapy in cervical cancer. Jpn J Clin Oncol 42(4):309–313
Viswanathan AN, Dimopoulos J, Kirisits C, Berger D, Pötter R (2007) Computed tomography versus magnetic resonance imaging-based contouring in cervical cancer brachytherapy: Results of a prospective trial and preliminary guidelines for standardized contours. Int J Radiat Oncol Biol Phys 68(2):491–498
Roh HJ, Kim KB, Lee JH, Kim HJ, Kwon YS, Lee SH (2018) Early cervical cancer: Predictive relevance of preoperative 3‑Tesla multiparametric magnetic resonance imaging. Int J Surg Oncol. https://doi.org/10.1155/2018/9120753
Dappa E, Elger T, Hasenburg A, Düber C, Battista MJ, Hötker AM (2017) The value of advanced MRI techniques in the assessment of cervical cancer: A review. Insights Imaging 8(5):471–481
Souhami L, Seymour R, Roman TN et al (1993) Weekly cisplatin plus external beam radiotherapy and high dose rate brachytherapy in patients with locally advanced carcinoma of the cervix. Int J Radiat Oncol Biol Phys 27(4):871–878
Morris M, Eifel PJ, Lu J et al (1999) Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med 340(15):1137–1143
Pearcey R, Brundage M, Drouin P et al (2002) Phase III trial comparing radical radiotherapy with and without cisplatin chemotherapy in patients with advanced squamous cell cancer of the cervix. J Clin Oncol 20(4):966–972
Pötter R, Georg P, Dimopoulos JC, Grimm M, Berger D, Nesvacil N, Georg D, Schmid MP, Reinthaller A, Sturdza A et al (2011) Clinical outcome of protocol based image (MRI) guided adaptive brachytherapy combined with 3D conformal radiotherapy with or without chemotherapy in patients with locally advanced cervical cancer. Radiother Oncol 100(1):116–123
Lindegaard JC, Fokdal LU, Nielsen SK, Juul-Christensen J, Tanderup K (2013) MRI-guided adaptive radiotherapy in locally advanced cervical cancer from a Nordic perspective. Acta Oncol 52(7):1510–1519
Mazeron R, Gilmore J, Dumas I, Champoudry J, Goulart J, Vanneste B, Tailleur A, Morice P, Haie-Meder C (2013) Adaptive 3D image-guided brachytherapy: A strong argument in the debate on systematic radical hysterectomy for locally advanced cervical cancer. Oncologist 18(4):415–422
Nomden CN, de Leeuw AA, Roesink JM, Tersteeg RJ, Moerland MA, Witteveen PO, Schreuder HW, van Dorst EB, Jürgenliemk-Schulz IM (2013) Clinical outcome and dosimetric parameters of chemo-radiation including MRI guided adaptive brachytherapy with tandem-ovoid applicators for cervical cancer patients: A single institution experience. Radiother Oncol 107(1):69–74
Gill BS, Kim H, Houser CJ, Kelley JL, Sukumvanich P, Edwards RP, Comerci JT, Olawaiye AB, Huang M, Courtney-Brooks M, Beriwal S (2015) MRI-guided high-dose-rate intracavitary brachytherapy for treatment of cervical cancer: The University of Pittsburgh experience. Int J Radiat Oncol Biol Phys 91(3):540–547
Ribeiro I, Janssen H, De Brabandere M, Nulens A, De Bal D, Vergote I, Van Limbergen E (2016) Long term experience with 3D image guided brachytherapy and clinical outcome in cervical cancer patients. Radiother Oncol 120(3):447–454
Mahantshetty U, Krishnatry R, Hande V, Jamema S, Ghadi Y, Engineer R, Chopra S, Gurram L, Deshpande D, Shrviastava S (2017) Magnetic resonance image guided adaptive brachytherapy in locally advanced cervical cancer: An experience from a tertiary cancer center in a low and middle income countries setting. Int J Radiat Oncol Biol Phys 99(3):608–617
Sung Uk L, Young Ae K, Young-Ho Y et al (2017) General health status of long-term cervical cancer survivors after radiotherapy. Strahlenther Onkol 193(7):543–551
Wachter-Gerstner N, Wachter S, Reinstadler E et al (2003) The impact of sectional imaging on dose escalation in endocavitary HDR-brachytherapy of cervical cancer: Results of a prospective comparative trial. Radiother Oncol 68(1):51–59
Chen SW, Liang JA, Yang SN et al (2003) The adverse effect of treatment prolongation in cervical cancer by high-dose-rate intracavitary brachytherapy. Radiother Oncol 67(1):69–76
Fyles A, Keane TJ, Barton M et al (1992) The effect of treatment duration in the local control of cervix cancer. Radiother Oncol 25(4):273–279
Girinsky T, Rey A, Roche B et al (1993) Overall treatment time in advanced cervical carcinomas: A critical parameter in treatment outcome. Int J Radiat Oncol Biol Phys 27(5):1051–1056
Perez CA, Grigsby PW, Castro-Vita H et al (1995) Carcinoma of the uterine cervix. I. Impact of prolongation of overall treatment time and timing of brachytherapy on outcome of radiation therapy. Int J Radiat Oncol Biol Phys 32(5):1275–1288
Kim YJ, Kim JY, Kim Y et al (2016) Magnetic resonance image-guided brachytherapy for cervical cancer: Prognostic factors for survival. Strahlenther Onkol 192(12):922–930
Poetsch N, Sturdza A, Aust S et al (2019) The value of pretreatment serum butyrylcholinesterase level as a novel prognostic biomarker in patients with cervical cancer treated with primary (chemo-)radiation therapy. Strahlenther Onkol 195(5):430–440
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
R. Vojtíšek, E. Sukovská, J. Baxa, M. Budíková, P. Kovářová and J. Fínek declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Vojtíšek, R., Sukovská, E., Baxa, J. et al. Late side effects of 3T MRI-guided 3D high-dose rate brachytherapy of cervical cancer. Strahlenther Onkol 195, 972–981 (2019). https://doi.org/10.1007/s00066-019-01491-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01491-0
Keywords
- Cervical cancer
- 3D brachytherapy
- Uterovaginal brachytherapy
- 3T MRI-guided brachytherapy
- Late side effects